Abstract
Purpose
To evaluate the efficacies of cyclophosphamide, methotrexate, and fluorouracil (CMF) and tegafur–uracil (UFT) as adjuvant therapy in patients with resected stage I–IIIA breast cancer by immunohistochemistry (IHC)-based subtype and to determine the relationships between clinicopathological factors and long-term outcomes.
Methods
A pooled analysis of the randomized controlled N·SAS-BC 01 and CUBC studies was conducted. Expression of hormone receptors (HRs; estrogen and progesterone receptors), human epidermal growth factor receptor 2 (HER2), and Ki67were assessed by IHC. Tumor-infiltrating lymphocytes (TILs) and nuclear/histological grades were determined by hematoxylin and eosin staining. Relapse-free survival (RFS) and overall survival (OS) were estimated by Kaplan–Meier analysis and hazard ratios were determined by Cox model adjusted for baseline tumor size and nodal status.
Results
A total of 689 patients (342 CMF and 347 UFT) were included in the analyses with a median follow-up of 11.1 years. There was no significant difference in RFS or OS between the two cohorts (RFS: 0.96 [95% confidence interval: 0.71–1.30], log-rank test p = 0.80; OS: 0.93 [0.64–1.35], p = 0.70). There was no difference in RFS or OS between the two cohorts for HR+/HER2− and HR+/HER2+ subtypes. RFS was significantly longer in patients treated with UFT compared with CMF in patients with HR−/HER2+ subtype (0.30 [0.10–0.88], p = 0.03). A high TILs level was associated with a better OS compared with low TILs level (p = 0.02).
Conclusions
This long-term follow-up study showed that RFS and OS were similar in patients with luminal-type breast cancer treated with CMF and UFT.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The Japanese Collaborative Study Group of Adjuvant Chemoendocrine Therapy for Breast Cancer (ACETBC) established adjuvant endocrine therapy with the oral fluoropyrimidine tegafur–uracil (UFT) to treat patients with early-stage breast cancer based on meta-analyses including studies conducted between 1988 and 1995 [1, 2]. However, the standard postoperative adjuvant chemotherapy in the European Union and the USA at that time was cyclophosphamide, methotrexate, and fluorouracil (CMF), and the National Surgical Adjuvant Study for Breast Cancer (N·SAS-BC) 01 and Comparative Trial of UFT + tamoxifen (TAM) with CMF + TAM in Adjuvant Therapy for Breast Cancer (CUBC) studies were, therefore, initiated in 1996 to demonstrate the non-inferiority of UFT compared with CMF in patients with resected stage I–IIIA breast cancer [3, 4]. Although neither study demonstrated non-inferiority because the target number of patients was not reached, a pooled analysis combining these studies that was conducted to overcome this issue showed that UFT was non-inferior to CMF in estrogen receptor-positive (ER+) patients [5]. Furthermore, a recent study in which the patients in these two studies were followed up for over 10 years demonstrated that the Kaplan–Meier curves for these two regimens for relapse-free survival (RFS) and overall survival (OS) appeared to be superimposable [6].
A treatment choice for breast cancer has recently been determined based on the current standard clinicopathological biomarkers, including the expression levels of hormone receptors (HRs; ER and progesterone receptor [PgR]), human epidermal growth factor receptor 2 (HER2), and Ki67 [7]. However, these markers were not completely established when the N·SAS-BC 01 and CUBC studies were initiated in 1996, and the findings are thus not fully applied in clinical practice. We therefore examined the expression of ER, PgR, HER2, Ki67, and tumor-infiltrating lymphocytes (TILs), as well as nuclear and histological grades, in tumor specimens from patients enrolled in these two studies using the currently available measurement methods.
In this cross-sectional, observational, pooled study, we evaluated the efficacies of adjuvant CMF and UFT according to immunohistochemistry (IHC)-based intrinsic subtypes and the relationships between the clinicopathological factors and updated long-term follow-up prognostic outcomes in patients with resected stage I–IIIA breast cancer enrolled in the randomized N·SAS-BC 01 and CUBC studies to identify a subset of patients responsive to UFT and CMF.
Materials and methods
This study (UMIN000022571) was approved by the independent ethics committee at each study site and conducted in agreement with the Helsinki Declaration and ethical guidelines for medical research on humans. Written consent was obtained from patients before initiating any process in this study. If written consent could not be obtained because a patient had died or could not be reached, samples were sent to a central pathology review office after confirmation by each independent ethics committee that the various provisions based on the Ethical Guidelines for Medical and Health Research Involving Human Subjects had been met.
Previous N·SAS-BC 01 and CUBC studies
Details of the N·SAS-BC 01 and CUBC studies and subsequent analyses have been described previously [3,4,5]. In brief, patients were enrolled in the N·SAS-BC 01 and CUBC studies from October 1996 to April 2001 and from September 1996 to July 2000, respectively. Both studies included patients with resected stage I–IIIA breast cancer, irrespective of their HR status, but the N·SAS-BC 01 study enrolled high-risk (invasive ductal carcinoma with invasive size ≥ 5 mm and grade 2 or 3, or invasive lobular carcinoma, or metaplastic carcinoma), node-negative, and the CUBC study enrolled node-positive patients (ranged 1–9). Patients in both studies were treated with 6 cycles of either CMF or UFT for 2 years. Patients in the CUBC study also received TAM for 2 years, irrespective of their HR expression status, and patients with ER+, PgR+, or both in the N·SAS-BC 01 study were treated with TAM for 5 years. No patient was treated with trastuzumab in the two studies, and radiation therapy was allowed only in the N·SAS-BC 01 study. Protein expression levels of ER and PgR to assess patient characteristics were determined by enzyme immunoassay at each participating hospital.
Patients
Patients included in the previous N·SAS-BC 01 and CUBC studies with available paraffin-embedded specimens of surgically excised tumor tissue and for whom use of the specimens had been authorized by the applicable independent ethics committee were included in this study. Patients who declined consent for use of their samples were excluded from the study.
Detection and evaluation of clinicopathological factors and prognostic outcomes
The study outcomes were RFS and OS according to HR/HER2 subtypes, and the relationships between clinicopathological factors, including age, tumor size, HR, HER2, Ki67, histological grade and TILs, and updated long-term follow-up prognostic outcomes (RFS and OS) in patients treated with CMF and UFT. In this study, RFS was defined as the period from the date of randomization to the last-confirmed date of no recurrence or of death from any cause, and OS was defined as the period from the date of randomization to the date of death from any cause with a cut-off date of June 30, 2018.
Protein expression levels of ER, PgR, HER2, Ki67 and TILs, as well as nuclear and histological grades, were assessed in the paraffin-embedded sections from each patient and evaluated by central pathological review. ER, PgR, and Ki67 protein expression were detected by immunohistochemistry with monoclonal antibodies SP1, 1E2 (Roche Diagnostics K.K., Japan), and MIB-1 (DAKO Japan Agilent, Japan), respectively. ER and PgR protein expression levels were determined as the sum of the proportion score (0–5) and intensity score (0–3), and ER+ and PgR+ were defined as total scores of 3–8 and ER− and PgR− as total scores of 0–2. Based on the expression results, HR positivity (HR +) was defined as ER+ and/or PgR+, and HR negativity (HR−) as ER− and PgR−.
HER2 expression was detected by semi-quantitative IHC assay (DAKO HercepTest II, Agilent, Japan; score 0–3+) in samples from all patients, with further fluorescence in situ hybridization (FISH) analysis in those with 2+ staining (PathVysion HER-2 DNA Probe Kit; Abbott, Japan). HER2 negativity (HER2−) was defined as an IHC score of 0–2 and negative FISH, and HER2-positive (HER2+) as an IHC score of 2 or 3 and positive FISH results. Nuclear grade (grades 1–3) [8, 9], and histological grade (grades 1–3) [10] were evaluated in hematoxylin and eosin-stained sections. Expression of TILs was evaluated according to the criteria of International TILs Working Group 2014 [11,12,13]. Briefly, using an optical microscope under × 200 and × 400 magnifications, the panel pathologists classified TILs levels into the following three grades: low < 10%, intermediate ≥ 10 to ≤ 40%, and high > 40%.
Statistical methods
Summary statistics, number of patients, mean, standard deviation, minimum, median, and maximum values were obtained for the patients’ baseline characteristics. Between-cohort differences were evaluated using χ2 test and t test. RFS and OS were estimated using Kaplan–Meier analysis, and differences between the two treatment cohorts were tested by the log-rank test. Evaluations of RFS and OS in subgroups were adjusted for clinical characteristics chosen based on the selection criterion set at α = 0.15, namely tumor size (< 3 and ≥ 3 cm) and nodal status (0 and ≥ 1). Hazard ratios and 95% confidence intervals (CIs) were determined using univariate unadjusted Cox proportional hazards model to evaluate the prognostic factors and were summarized in forest plots. Statistical significance was set at a two-sided p < 0.05. Statistical analysis was performed using SAS version 9.4 or higher (SAS Institute, Inc., Cary, NC, USA).
Results
Patients
The study was conducted from December 2015 to November 2018. A total of 1057 patients enrolled and analyzed in the N·SAS-BC 01 and CUBC studies were involved in this pooled analysis (Fig. 1), including 707 patients in the N·SAS-BC 01 and 350 patients in the CUBC studies. Paraffin-embedded pathology specimens were available for 545 and 161 of the study patients, respectively. Seventeen patients were excluded from the study because submitted pathology specimens were ductal carcinoma in situ component, and 689 patients (342 treated with CMF and 347 treated with UFT) were therefore included in the final analyses. Characteristics of evaluable patients in the N·SAS-BC 01 and CUBC studies and those included in the present study are summarized in Supplementary Table 1.
Patient flow diagram in the previous N·SAS-BC 01 [3] and CUBC study [4] and the present study. CMF cyclophosphamide, methotrexate, and fluorouracil, CUBC comparative trial of UFT + tamoxifen with CMF + tamoxifen in adjuvant therapy for breast cancer, N·SAS-BC 01 National Surgical Adjuvant Study for Breast Cancer, UFT tegafur-uracil
The patients treated with CMF and UFT were well balanced in terms of age, tumor size, nodal stage, tumor subtype, Ki67, and TILs expression, and nuclear and histological grades (Table 1). Patients divided according to subtypes were also well balanced (Supplementary Table 2).
RFS and OS in all patients and according to HR/HER2 subtypes
The median follow-up time as of December 31, 2015 was 11.1 years (12.1 years in the N·SAS-BC 01 trial and 8.3 years in the CUBC trial) [6]. The Kaplan–Meier RFS curves for the CMF and UFT cohorts in all patients and those included in the final analysis are presented in Supplementary Fig. 1. There was no significant difference in RFS between the two cohorts for patients included in the final analysis (p = 0.80). RFS analysis by HR and HER2 receptor subtypes showed that patients with HR−/HER2+ subtype treated with UFT had a significantly higher RFS than those treated with CMF (p = 0.03). However, there was no significant difference in RFS between the treatment cohorts for any other HR/HER2 subtypes (p > 0.50, Fig. 2).
Kaplan–Meier survival curves for relapse-free survival adjusted for tumor size and nodal status in patients stratified according to HR/HER2 subtype. CI confidence interval, CMF cyclophosphamide, methotrexate, and fluorouracil, HER2 human epidermal growth factor receptor 2, HR hormone receptor, UFT tegafur–uracil
There was no significant difference in OS between the two cohorts for patients included in the final analysis (p = 0.70, Supplementary Fig. 1). OS analysis by HR and HER2 receptor subtypes showed that patients with HR−/HER2+ subtype treated with UFT had a numerically higher OS than those treated with CMF. However, there was no significant difference in OS between the treatment cohorts for any HR/HER2 subtype (p > 0.13, Fig. 3).
Kaplan–Meier survival curves for overall survival adjusted for tumor size and nodal status in patients stratified according to HR/HER2 subtype. CI confidence interval, CMF cyclophosphamide, methotrexate, and fluorouracil, HER2 human epidermal growth factor receptor 2, HR hormone receptor, UFT tegafur–uracil
Subgroup analyses of RFS in patients included in the final analysis and according to HR/HER2 subtypes
Subgroup analyses according to baseline characteristics showed no significant differences in the RFS between the two treatment cohorts (Fig. 4). Although it did not reach statistical significance, RFS in patients treated with UFT tended to be longer in patients with HR−/HER2+ subtype (hazard ratio 0.38 [0.13–1.09], p = 0.07) and in patients with high TILs levels (hazard ratio 0.24 [0.05–1.10], p = 0.07).
Similarly, baseline characteristics had no significant impact on the RFS following CMF or UFT treatment in patients with HR+/HER2− subtype (Fig. 5).
Subgroup analyses showed no notable trend in OS between the two treatment cohorts in patients included in the final analysis or in those stratified according to HR/HER2 subtypes (data not shown).
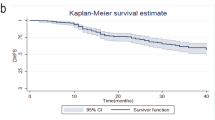
Analysis of TILs expression levels as a prognostic factor
At 10 years, there were 59, 10, and 4 OS events, and the OS rates were 86.5% (95% CI 82.9–89.4), 92.3% (86.1–95.8), and 93.4% (83.2–97.5) in patients with low, intermediate, and high TILs levels, respectively. Among patients included in the final analysis, patients with high TILs levels showed a significantly improved OS compared to those with low TILs levels (p = 0.02, Fig. 6).
Similar trends in OS were found in patients with HR−/HER2− and HR−/HER2+ breast cancer, but no difference was detected in HR+/HER2− subtype irrespective of TILs levels (Fig. 7).
Kaplan–Meier survival curves for overall survival according to tumor-infiltrating lymphocyte level (low, intermediate, high) adjusted for tumor size and nodal status in patients stratified according to HR/HER2 subtype. CI confidence interval, H high, HER2 human epidermal growth factor receptor 2, HR hormone receptor, I intermediate, L low, ND not determined
Discussion
The present study re-evaluated the efficacies of UFT and CMF using a pooled analysis of randomized controlled studies and newly obtained clinicopathological data and updated long-term prognosis outcomes. Although the statistical power was not sufficient to test the non-inferiority, our results showed similar efficacies of UFT and CMF in patients with luminal-type breast cancer. This study was also clinically significant because it demonstrated the efficacies of UFT and CMF in preventing late recurrence in Japanese patients with luminal-type breast cancer, which is a major clinical concern [14].
The efficacy of UFT determined by RFS and OS was similar to that of CMF in patients with HR+/HER2− and HR+/HER2+ subtypes and was significantly better in patients with HR−/HER2+ subtype. These results indicate that UFT is effective in patients with these subtypes, and its less toxic nature suggests that it may be a suitable option for patients who are intolerant of standard therapy. To the best of our knowledge, this is the first study demonstrating a better prognosis with UFT in patients with HR−/HER2+ subtype. However, further studies with larger sample sizes are needed to verify our results and to clarify the mechanism responsible for the better prognosis in patients with this specific subtype. Although the differences were not significant, both RFS and OS were slightly shorter in the UFT compared with the CMF cohort patients with HR−/HER2− subtype. Further studies are therefore needed to find more suitable therapeutic options for patients with this subtype.
Our results showed that high levels of TILs were associated with a favorable prognosis among the patients included in the final analysis and among patients with HR−/HER2− and HR−/HER2+ subtypes that are consistent with previous studies [15,16,17]. However, the results showed no effect of TILs level on prognosis in patients with HR+/HER2− subtype, suggesting that TILs may play a different role in these patients compared with patients with HR+ subtypes. Regarding the HR+/HER2+ subtype, more samples are needed to draw a solid conclusion about this relationship. The interactions between tumor cells and immune cells have only recently become a focus of investigations, and information on the relationship between TILs and prognostic outcomes is still lacking. However, given that chemotherapy and adjuvant therapy also affect the immune system, the current data including over 10 years of follow-up data and clinicopathological factors correlated at an individual patient level are expected to improve our understanding of such interactions.
This study had some limitations. First, all patients in the CUBC study were treated with TAM, irrespective of their HR expression status, for 2 years. However, the current recommendation is that only HR+ patients should receive TAM for > 5 years. The potential impact of 2-year rather than 5-year TAM treatment on RFS and OS in HR+ patients in the CUBC study thus needs to be taken into consideration when interpreting the present results. Second, treatment regimens investigated in the previous N·SAS-BC 01 and CUBC studies differ from the current standard therapy. For example, no patients with HER2+ in the N·SAS-BC 01 and CUBC studies were treated with trastuzumab, because trastuzumab had not yet been approved when these studies were carried out. In addition, the current standard postoperative adjuvant chemotherapy consists of anthracyclines or taxanes, whereas CMF therapy is currently determined as useful in certain circumstances only. Furthermore, the previous Trial Assigning Individualized Options for Treatment (TAILORx) demonstrated no benefit of adding chemotherapy to hormone therapy in the majority of node-negative HR+/HER2− breast cancer patients, determined based on the 21-gene recurrence score 11–25 using Oncotype DX [18], indicating that the present study included patients who may not benefit from adjuvant chemotherapy. A future study is needed to compare the efficacy of UFT with the current standard therapy using real-world data, to identify a patient population that responds favorably to the UFT therapy. Third, tumor sections were collected from 708 out of 1057 patients, which suggests a potential bias in the sample collection. Indeed, a significant difference in the number of lymph nodes was found between eligible patients in the previous two studies and those included in this study (Supplementary Table 1, p < 0.0001) because more specimens were collected in patients in the N·SAS-BC 01 study than the CUBC study. However, no significant difference was found between two treatment cohorts in the present study.
Breast cancer subtypes have been studied based on a set of gene expression patterns, and commercially available genomic tests, such as Oncotype DX, have been effectively utilized to determine the tailored treatment for each patient’s cancer subtype [18, 19]. Further studies using genomic tests are expected to identify a set of recurrence risk factors and to find which risk factors respond to UFT therapy.
In conclusion, the present pooled analysis of two randomized controlled studies demonstrated that RFS and OS in the UFT and CMF cohorts were similar in patients with luminal-type breast cancer.
Data availability
Data generated or analyzed during this study are on file with and are not publicly available.
Abbreviations
- CI:
-
Confidence interval
- CMF:
-
Cyclophosphamide, methotrexate, and 5-fluorouracil
- CUBC:
-
Comparative Trial of UFT + TAM with CMF + TAM in Adjuvant Therapy for Breast Cancer
- ER:
-
Estrogen receptor
- FISH:
-
Fluorescence in situ hybridization
- HER2:
-
Human epidermal growth factor receptor 2
- HR:
-
Hormone receptor
- N·SAS-BC:
-
National Surgical Adjuvant Study for Breast Cancer
- OS:
-
Overall survival
- PgR:
-
Progesterone receptor
- RFS:
-
Relapse-free survival
- TAM:
-
Tamoxifen
- TILs:
-
Tumor-infiltrating lymphocytes
- UFT:
-
Tegafur–uracil
References
Kasumi F, Yoshimoto M, Uchino J, Abe R, Nomura Y, Sugimachi K, Nakazato H, Abe O (2003) Meta-analysis of five studies on tegafur plus uracil (UFT) as post-operative adjuvant chemotherapy for breast cancer. Oncology 64:146–153. https://doi.org/10.1159/000067763
Noguchi S, Koyama H, Uchino J, Abe R, Miura S, Sugimachi K, Akazawa K, Abe O (2005) Postoperative adjuvant therapy with tamoxifen, tegafur plus uracil, or both in women with node-negative breast cancer: a pooled analysis of six randomized controlled trials. J Clin Oncol 23:2172–2184. https://doi.org/10.1200/JCO.2005.02.158
Watanabe T, Sano M, Takashima S, Kitaya T, Tokuda Y, Yoshimoto M, Kohno N, Nakagami K, Iwata H, Shimozuma K, Sonoo H, Tsuda H, Sakamoto G, Ohashi Y (2009) Oral uracil and tegafur compared with classic cyclophosphamide, methotrexate, fluorouracil as postoperative chemotherapy in patients with node-negative, high-risk breast cancer: National Surgical Adjuvant Study for Breast Cancer 01 Trial. J Clin Oncol 27:1368–1374. https://doi.org/10.1200/JCO.2008.18.3939
Park Y, Okamura K, Mitsuyama S, Saito T, Koh J, Kyono S, Higaki K, Ogita M, Asaga T, Inaji H, Komichi H, Kohno N, Yamazaki K, Tanaka F, Ito T, Nishikawa H, Osaki A, Koyama H, Suzuki T (2009) Uracil-tegafur and tamoxifen vs cyclophosphamide, methotrexate, fluorouracil, and tamoxifen in post-operative adjuvant therapy for stage I, II, or IIIA lymph node-positive breast cancer: a comparative study. Br J Cancer 101:598–604. https://doi.org/10.1038/sj.bjc.6605218
Ohashi Y, Watanabe T, Sano M, Koyama H, Inaji H, Suzuki T (2010) Efficacy of oral tegafur-uracil (UFT) as adjuvant therapy as compared with classical cyclophosphamide, methotrexate, and 5-fluorouracil (CMF) in early breast cancer: a pooled analysis of two randomized controlled trials (N·SAS-BC 01 trial and CUBC trial). Breast Cancer Res Treat 119:633–641. https://doi.org/10.1007/s10549-009-0635-3
Yonemori K, Ohsumi S, Takao S, Tokuda Y, Ito Y, Nakagami K, Takahashi M, Yoshidome K, Nakayama T, Yamaguchi Y, Ohashi Y, Inaji H, Watanabe T (2019) Long-term follow-up of two randomized controlled trials (N-SAS-BC01 trial and CUBC trial) comparing oral tegafur-uracil (UFT) versus classical cyclophosphamide, methotrexate, and 5-fluorouracil (CMF) as adjuvant therapy in early breast cancer. Cancer Res SABCS. https://doi.org/10.1158/1538-7445.SABCS18-P1-13-09
Curigliano G, Burstein HJ, Winer EP, Gnant M, Dubsky P, Loibl S, Colleoni M, Regan MM, Piccart-Gebhart M, Senn HJ, Thürlimann B et al (2017) De-escalating and escalating treatments for early-stage breast cancer: the St. Gallen International Expert Consensus on the Primary Therapy of Early Breast Cancer 2017. Ann Oncol 28:1700–1712. https://doi.org/10.1093/annonc/mdx308
Wolff AC, Hammond ME, Hicks DG, Dowsett M, McShane LM, Allison KH, Allred DC, Bartlett JM, Bilous M, Fitzgibbons P, Hanna W, Jenkins RB, Mangu PB, Paik S, Perez EA, Press MF, Spears PA, Vance GH, Viale G, Hayes DF (2013) American Society of Clinical Oncology; College of American Pathologists Recommendations for human epidermal growth factor receptor 2 testing in breast cancer: American Society of Clinical Oncology/College of American Pathologists clinical practice guideline update. J Clin Oncol 31:3997–4013. https://doi.org/10.1200/JCO.2013.50.9984
Tsuda H, Akiyama F, Kurosumi M, Sakamoto G, Watanabe T (1998) Establishment of histological criteria for high-risk node-negative breast carcinoma for a multi-institutional randomized clinical trial of adjuvant therapy. Japan National Surgical Adjuvant Study of Breast Cancer (NSAS-BC) Pathology Section. Jpn J Clin Oncol 28:486–491. https://doi.org/10.1093/jjco/28.8.486
Elston CW, Ellis IO (1991) Pathological prognostic factors in breast cancer I. The value of histological grade in breast cancer: experience from a large study with long-term follow-up. Histopathology 19:403–410. https://doi.org/10.1111/j.1365-2559.1991.tb00229.x
Salgado R, Denkert C, Demaria S, Sirtaine N, Klauschen F, Pruneri G, Wienert S, Van den Eynden G, Baehner FL, Penault-Llorca F, Perez EA, Thompson EA, Symmans WF, Richardson AL, Brock J, Criscitiello C, Bailey H, Ignatiadis M, Floris G, Sparano J, Kos Z, Nielsen T, Rimm DL, Allison KH, Reis-Filho JS, Loibl S, Sotiriou C, Viale G, Badve S, Adams S, Willard-Gallo K, Loi S (2015) The evaluation of tumor-infiltrating lymphocytes (TILs) in breast cancer: recommendations by an International TILs Working Group 2014. Ann Oncol 26:259–271
Kurozumi S, Inoue K, Matsumoto H, Fujii T, Horiguchi J, Oyama T, Kurosumi M, Shirabe K (2019) Prognostic utility of tumor-infiltrating lymphocytes in residual tumor after neoadjuvant chemotherapy with trastuzumab for HER2-positive breast cancer. Sci Rep 9:1583
Hendry S, Salgado R, Gevaert T et al (2017) Assessing tumor infiltrating lymphocytes in solid tumors: a practical review for pathologists and proposal for a standardized method from the International Immuno-Oncology Biomarkers Working Group. Part 1: assessing the host immune response, TILs in invasive breast carcinoma and ductal carcinoma in situ, metastatic tumor deposits and areas for further research. Adv Anat Pathol 24:235–251
Jatoi I, Anderson WF, Jeong JH, Redmond CK (2011) Breast cancer adjuvant therapy: time to consider its time-dependent effects. J Clin Oncol 29:2301–2304. https://doi.org/10.1200/JCO.2010.32.3550
Loi S, Sirtaine N, Piette F, Salgado R, Viale G, Van Eenoo F, Rouas G, Francis P, Crown JP, Hitre E, de Azambuja E, Quinaux E, Di Leo A, Michiels S, Piccart MJ, Sotiriou C (2013) Prognostic and predictive value of tumor-infiltrating lymphocytes in a phase III randomized adjuvant breast cancer trial in node-positive breast cancer comparing the addition of docetaxel to doxorubicin with doxorubicin-based chemotherapy: BIG 02–98. J Clin Oncol 31:860–867. https://doi.org/10.1200/JCO.2011.41.0902
Adams S, Gray RJ, Demaria S, Goldstein L, Perez EA, Shulman LN, Martino S, Wang M, Jones VE, Saphner TJ, Wolff AC, Wood WC, Davidson NE, Sledge GW, Sparano JA, Badve SS (2014) Prognostic value of tumor-infiltrating lymphocytes in triple-negative breast cancers from two phase III randomized adjuvant breast cancer trials: ECOG 2197 and ECOG 1199. J Clin Oncol 32:2959–2966. https://doi.org/10.1200/JCO.2013.55.0491
Denkert C, von Minckwitz G, Darb-Esfahani S, Lederer B, Heppner BI, Weber KE, Budczies J, Huober J, Klauschen F, Furlanetto J, Schmitt WD, Blohmer JU, Karn T, Pfitzner BM, Kümmel S, Engels K, Schneeweiss A, Hartmann A, Noske A, Fasching PA, Jackisch C, van Mackelenbergh M, Sinn P, Schem C, Hanusch C, Untch M, Loibl S (2018) Tumour-infiltrating lymphocytes and prognosis in different subtypes of breast cancer: a pooled analysis of 3771 patients treated with neoadjuvant therapy. Lancet Oncol 19:40–50. https://doi.org/10.1016/S1470-2045(17)30904-X
Sparano JA, Gray RJ, Makower DF, Pritchard KI, Albain KS, Hayes DF, Geyer CE Jr, Dees EC, Goetz MP, Olson JA Jr, Lively T, Badve SS, Saphner TJ, Wagner LI, Whelan TJ, Ellis MJ, Paik S, Wood WC, Ravdin PM, Keane MM, Moreno HLG, Reddy PS, Goggins TF, Mayer IA, Brufsky AM, Toppmeyer DL, Kaklamani VG, Berenberg JL, Abrams J, Sledge GW Jr (2018) Adjuvant chemotherapy guided by a 21-gene expression assay in breast cancer. N Engl J Med 379:111–121. https://doi.org/10.1056/NEJMoa1804710
Sparano JA, Gray RJ, Ravdin PM, Makower DF, Pritchard KI, Albain KS, Hayes DF, Geyer CE Jr, Dees EC, Goetz MP, Olson JA Jr, Lively T, Badve SS, Saphner TJ, Wagner LI, Whelan TJ, Ellis MJ, Paik S, Wood WC, Keane MM, Moreno HLG, Reddy PS, Goggins TF, Mayer IA, Brufsky AM, Toppmeyer DL, Kaklamani VG, Berenberg JL, Abrams J, Sledge GW Jr (2019) Clinical and genomic risk to guide the use of adjuvant therapy for breast cancer. N Engl J Med 380:2395–2405. https://doi.org/10.1056/NEJMoa1904819
Acknowledgements
This study was supported by SRL Medisearch Inc. Writing and editing of the manuscript were assisted by ASCA Corporation.
Funding
The research fund was provided to SRL Medisearch Inc. by Taiho Pharmaceutical under the study contract.
Author information
Authors and Affiliations
Contributions
SO, SS, NM, HT, HI, and TW contributed to the study conception and design. HT, FA, and MK conducted the central pathological review. Material preparation was performed by SO, NM, AS, NS, ST, SO, and YT. Data collection and analysis were performed by YO. The first draft of the manuscript was written by SO and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
S. Ohno received research grants from Taiho Pharmaceutical, Eisai, and honoraria from Chugai, AstraZeneca, Eli Lilly, Pfizer, and Eisai. SS received honoraria from Chugai, Eisai, AstraZeneca, Takeda, Novartis, Kyowa Kirin, Eli Lilly, MSD, and Pfizer; research grants from Daiichi Sankyo, Taiho Pharmaceutical, Eisai, Novartis, Takeda, and Chugai; and consultant fees from Chugai, Novartis, and Kyowa Kirin. NM received honoraria from Chugai, AstraZeneca, Pfizer, Eli Lilly, Eisai, and Takeda and research grants to the institution from Chugai, AstraZeneca, Kyowa Kirin, MSD, Novartis, Pfizer, Eli Lilly, Eisai, Nippon Kayaku, and Daiichi Sankyo. HT received research grants from Chugai and Taiho Pharmaceutical; and personal fees from Roche Diagnostics, Konica Minolta, Eisai, AstraZeneca, and Bristol-Myers Squibb. NS received personal fees from Chugai, Eisai, Pfizer, Sysmex, Taiho Pharmaceutical, Kyowa Kirin, and Eli Lilly Japan for outside the submitted work. S Ohsumi received lecture fee from AstraZeneca. YO received executive compensation from Statcom; honoraria from Daiichi Sankyo, Chugai, Shionogi, Taiho Pharmaceutical, Sanofi, and EP-CRSU; and research grant from Medical Member System for outside the submitted work. All other authors declare that they have no conflict of interest.
Ethical approval
The study was approved by the independent ethics committee at each study site and was conducted in agreement with the Helsinki Declaration, ethical guidelines for medical research on humans, and ethics guidelines for human genome/gene analysis research.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ohno, S., Saji, S., Masuda, N. et al. Relationships between pathological factors and long-term outcomes in patients enrolled in two prospective randomized controlled trials comparing the efficacy of oral tegafur–uracil with CMF (N·SAS-BC 01 trial and CUBC trial). Breast Cancer Res Treat 186, 135–147 (2021). https://doi.org/10.1007/s10549-020-06018-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-020-06018-1