Abstract
Purpose
The role of non-genetic factors as modifiers of TP53-related hereditary breast cancer (BC) risk is debated. In this regard, little is known about the impact of germline TP53 mutations on BC in sub-Saharan Africa, where the disease often presents in non-contraceptive multiparous premenopausal women with extended history of breastfeeding. Herein, we report the germline TP53 mutations found in a series of 92 Sudanese premenopausal BC patients characterized for reproductive history.
Methods
The entire TP53 coding sequence, including intron–exon boundaries and UTRs, was analyzed via DHPLC and direct sequencing, and the association of TP53 genotypes with BC risk and with individual lifetime exposures to reproductive factors was investigated with statistical tools.
Results
The germline TP53 mutation spectrum comprised 20 variants, 15 in the non-coding and 5 in the coding region. The latter included a deleterious missense mutation, c.817C>T (p.Arg273Cys), in a unique patient, and the common and functionally relevant coding polymorphism at amino acid 72 [Pro72Arg (rs1042522)]. The non-coding mutations included c.919+1G>A, a known deleterious splice site mutation, also in a unique patient. Notably, the 2 carriers of deleterious TP53 mutations clustered in the subset of cases with stronger reproductive history relative to childbearing age. When analyzed in comparison to population controls, the codon 72 polymorphism did not reveal associations with BC.
Conclusions
Our study suggests that the codon 72 Arg>Pro polymorphism is not implicated in premenopausal BC susceptibility, whereas multiparity and breastfeeding might be BC risk factors for carriers of deleterious TP53 mutations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Breast cancer (BC) is the most prevalent type of tumor in women who carry a deleterious germline TP53 mutation in the setting of the Li–Fraumeni syndrome (LFS, OMIM #151623) [1]. However, putatively deleterious germline TP53 mutations (OMIM #191170) are also associated with less prominent cancer phenotypes and, in genome-wide studies, seem to be more frequent than the estimated prevalence of the LFS [2]. In fact, TP53 mutations are found in ~ 2–3% of premenopausal BC patients unselected for the LFS criteria [3] and in < 1% to ~ 7% of the early onset BC cases (age < 30 years) in population-based series [4]. This suggests that non-genetic factors modify TP53-related inherited BC risk. In this regard, it is well known that reproductive history and exogenous exposure to female hormones are the most consistent modifiers of BC risk after genetic predisposition and age [5].
In Africa, BC often presents in multiparous women in the middle of their childbearing years, who are mostly unexposed to hormonal contraceptives and generally report long lifetime duration of breastfeeding [6,7,8]. Hence, the characterization of TP53 carriers in sub-Saharan African BC series might shed some light on the role of reproductive history as a modifier of TP53-related hereditary BC risk.
The majority of the genetic studies about BC in sub-Saharan Africa is focused on the analysis of the mutational spectra of the BRCA1/2 genes [9]. With regard to the TP53 gene, two cases of female BC in native sub-Saharan African mutation carriers were recently reported within a familial LFS context [10], but, to our knowledge, comprehensive data on germline TP53 variation in sub-Saharan African BC case series are still lacking.
Here, we describe the spectrum of germline TP53 mutations found in a mono-institutional Sudanese premenopausal BC series comprising 92 cases, that were consecutively recruited between 1999 and 2004, when the Sudanese fertility rate ranged from 5.54 to 5.20 [11,12,13].
Materials and methods
Patients and controls
The study was approved by the Institutional Ethical Committees of the National Cancer Institute, University of Gezira (NCI-UG) and “G. d’Annunzio” University. The 92 pathologically confirmed BC patients, all diagnosed within 45 years of age (mean age: 36.3 ± 5.9 years; range: 23–45 years) had been selected on a consecutive basis among the BC patients treated at NCI-UG from May 1999 through December 2004, as we previously described [11, 12]. Medical records were reviewed with regard to individual, pathological, clinical, and reproductive data (including self-reported information on age at menarche). Hormone receptor data were not available, due to poor fixation and storage of tissue blocks, a problem that we already highlighted [6]. A group of 180 control subjects (111 males and 69 females) was recruited from the Wad Medani city region (mean age 36.1 ± 10.4 years, range 20–70 years; male/female ratio 111/69; mean age of females 38.4 ± 10.1 years, range 20–65 years; mean age of males 34.7 ± 10.4 years; range 20–70 years). Due to the limited amounts of DNA, variable numbers of these controls were used to verify variant frequencies. Acid citrate–dextrose anticoagulated blood (10 ml) was collected from each patient and control and preserved at − 20 °C in aliquots. All patients and controls gave informed consent to the study, according to guidelines set by the NCI-UG.
TP53 mutation analysis
Genomic DNA was isolated from peripheral blood using the QIAamp DNA Blood Mini Kit (QIAGEN, Chatsworth, CA). The entire TP53 coding sequence (NM_000546), including intron–exon boundaries and UTRs, was analyzed via DHPLC using a Wave®Nucleic Acid Fragment Analysis System (Transgenomic Inc., San Jose, CA). To detect homozygous variants, the PCR-amplified samples were tested also after mixing with an aliquot of known wild-type DNA (2µl:5 µl). Samples with altered DHPLC profiles were directly sequenced using an ABI PRISMTM3100 genetic analyzer (Applied Biosystems, Foster City, CA). Primers for TP53 exons 1–11 were reported by Verselis et al. [14], those used for UTRs are listed in the online resources (Table ESM_1). Variants were always confirmed in replicate assays. Nomenclature follows the guidelines of the Human Genome Variation Society (HGVS, http://www.HGVS.org/varnomen), clinical significance and geographic distribution were assessed using ClinVar (https://www.ncbi.nlm.nih.gov/clinvar/), the International Agency for Research on Cancer (IARC) TP53 database [15], MutPred2 [http://mutpred.mutdb.org], Ensemble (1000 Genomes Project, phase 3) [https://www.ensembl.org/] and COSMIC [https://cancer.sanger.ac.uk/cosmic]. Variants with minor allele frequency (MAF) ≥ 1% were considered neutral [16], those with MAF < 1% and deleterious mutations were searched in healthy controls.
Statistical analyses
A logistic regression model was applied to test the association of TP53 genotypes and haplotypes with BC risk. Results were expressed as odds ratio (OR) and relative 95% confidence interval (95% CI). For each polymorphism with minor allele frequency (MAF) ≥ 5%, the Hardy–Weinberg equilibrium (HW) was tested using the Hardy–Weinberg calculator (http://ihg.gsf.de/cgi-bin/hw/hwa1.pl). The threshold of statistical significance was set at p = 0.05. Data analysis was performed using SPSS Advanced Statistics TM 13 (2004, Chicago, IL, USA).
To approximate individual lifetime exposures to reproductive factors, we developed reproductive factor scores for each patient meeting verifiable data requirements (age at menarche, number of pregnancies, and reported breastfeeding of infants). Given the difficulty of obtaining precise information on the individual duration of the breastfeeding periods, we considered a period of 24 months for each child, based on the frequency of extended breast feeding at 2 years of age in rural Sudan for the period during which the BC cases were recruited [17]. The reproductive factor scores were generated by subtracting the total period in months estimated to be occupied by pregnancies and breastfeeding to the cumulative number of fertile months calculated from menarche to BC diagnosis. Relative to the median, the factor score values ranged from negative (−) to positive (+), thus identifying 2 subsets of patients, respectively, defined by stronger (−) versus weaker (+) reproductive history relative to childbearing age. Fisher’s exact test was used to analyze the significance of the differences in the frequencies of deleterious mutations and codon 72 genotypes (homozygous and heterozygous) between the 2 subsets of cases defined by reproductive factor score values.
Results and discussion
We characterized for germline TP53 mutations 92 female BC patients selected based on diagnosis within 45 years of age. Overall, we found 20 germline TP53 variants (Table 1), of which 5 in the coding region (2 missense, including a deleterious mutation plus a common coding polymorphism and 3 synonymous) and 15 in the non-coding region (6 intronic, including 5 polymorphisms plus a known deleterious splice site mutation, and 9 in the UTRs, of which 5 were known polymorphisms and 4 novel). The findings were consistent with the expected higher frequency of non-coding sequence variation [15, 16, 18].
The two deleterious mutations were c.817C>T (p.Arg273Cys), detected in a patient diagnosed with BC at age 32 (case S6), and (c.919+1G>A), detected in a patient diagnosed at age 30 (case S13). No reliable family history data were retrievable for these cases, as is usually the case in rural sub-Saharan Africa [7]. The p.Arg273Cys mutation, located in the DNA-binding domain, is reported with both somatic (706-fold) and germline (35-fold) status in the TCAG [http://dgv.tcag.ca] and IARC [http://www-p53.iarc.fr/; R19] TP53 databases. The c.919+1G>A mutation, that targets the splice donor site of intron 8, is also reported in the IARC database as germline (sixfold) and somatic (13-fold). Thus, the prevalence of identified deleterious TP53 mutations was 2.17% (2/92), i.e., comparable to that found in Western premenopausal BC series [3]. Ours is likely an underestimate, because we did not investigate regulatory elements outside the UTRs. Besides, our screening techniques, highly sensitive for point mutations and small insertions/deletions (the most common TP53 mutation types), do not detect genomic rearrangements.
The 4 novel UTR variants were found in individual patients and not in control chromosomes from the Wad Medani population (Table 1). It cannot be excluded that these variants could influence TP53 mRNA stability and translational efficiency, but their evaluation requires functional assays, which are beyond the scope of the present report.
Apart from the above mentioned, the remaining 14 variants, found in several cases, correspond to known polymorphisms (Table 1). Still, polymorphisms may affect TP53 protein level or functions, especially when altering the coding sequence, and could thus influence BC risk. In particular, there is a debate on the common TP53 polymorphism at amino acid 72 [Pro72Arg (rs1042522)], here referred to as P72 and R72, which was one of the 4 most frequent polymorphisms in our case series (Table 1) [19, 20]. The P72 variant, that has weaker transcriptional activity and lower apoptotic potential [21, 22], is linked to poor prognosis after adjuvant therapy, rather than to BC risk [23], while R72 is associated with increased mitochondrial function, metastatic capability [24], and higher affinity for the E6 oncoprotein of the human papillomaviruses [25]. In this regard, it was reported that Sudanese BC patients show an excess of homozygous R72 compared to controls [26]. However, in the present case series, the frequencies of P72 and R72 (RS1042522) did not significantly differ between cases and controls, which does not support an association of this polymorphism with premenopausal BC risk (Table 2).
The other 3 polymorphisms with MAF ≥ 5% were c.74+38G>C (rs1642785), c.96+56 ins16 (rs17878362), reportedly linked to P72 and associated with cancer risk in non-Africans [27], and c.672+62A>G (rs1625895) (Tables 1, 2). The frequencies of these variants, verified in population controls (Table 2), were in agreement with the Hardy–Weinberg equilibrium for c.672+62A>G (Table 2) and, rather than showing association with BC, were unbalanced towards controls for both c.74+38G>C (p = 0.022) and c.96+56 ins16 (p = 0.031).
In the general female population, early parity is associated with decreased long-term risk of BC, however, regardless of age at delivery, the risk slightly and transiently increases in the first 3–5 years after childbirth [28]. At present, there is still a lack of data concerning the influence of reproductive history on BC risk in carriers of TP53 mutations. Experimental evidence from a mouse model shows that parity protects p53-deficient mice from developing mammary preneoplasia [29].
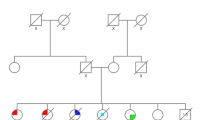
In the currently studied BC series, the available information allowed to create reproductive factor scores for 85/92 cases. These scores were based on the estimated cumulative number of months not occupied by pregnancy and breastfeeding during the fertile period up to breast cancer diagnosis. Relative to the median value (267), the factor score differences ranged from − 148.49 to + 160.09 and identified 2 subsets of cases, designated A (35 cases, lower 95% CI of mean from − 148.49 to − 19.71) and B (38 cases, upper 95% CI of mean from 11.34 to 160.09), defined by stronger (subset A) versus weaker (subset B) reproductive history adjusted for childbearing age (Fig. 1). The two carriers of deleterious TP53 mutations, S6, c.817C>T (p.Arg273Cys), age 32, and S13 (c.919+1G>A), age 30, respectively, reporting 6 and 4 live births before BC diagnosis, joined subset A (individual reproductive factor scores: − 86.77 and − 68.77, respectively). This suggests that, differently from the murine model [29], parity and breastfeeding could be harmful for TP53 mutation carriers. The codon 72 polymorphism did not reveal relevant associations with reproductive history, except a non-significant excess of codon 72 heterozygotes in subset A (Fig. 1).
Reproductive factor scores expressed in terms of individual histograms for 85 breast cancer patients. Relative to the median, the factor scores differences ranged from − 148.49 to + 160.09 and identified 2 subsets of cases, designated A (35 cases, lower 95% CI of mean from − 148.49 to − 19.71) and B (38 cases, upper 95% CI of mean from 11.34 to 160.09), respectively, with stronger (A) and weaker (B) reproductive history. The 12 cases between the blue dashed lines fall outside the CIs. The two carriers of deleterious TP53 mutations (red arrows) are in cluster A. Codon 72 heterozygotes (gray histograms) are more numerous in subset A, but without statistical significance. Homozygous carriers of P72 (black histograms) and R72 (white histograms) split between the two subsets
Conclusions
In conclusion, this study shows that in our Sudanese context, the common and debated polymorphism at codon 72 is not associated with premenopausal BC, and suggests that parity and breastfeeding represent BC risk factors for TP53 mutation carriers. Given the relatively small size of our case series, our findings should be interpreted with caution and confirmatory studies in Sudan and other sub-Saharan African countries are needed.
References
Mai PL, Best AF, Peters JA, DeCastro RM, Khincha PP, Loud JT, Bremer RC, Rosenberg PS, Savage SA (2016) Risks of first and subsequent cancers among TP53 mutation carriers in the National Cancer Institute Li-Fraumeni syndrome cohort. Cancer 122(23):3673–3681
Amadou A, Waddington Achatz MI, Hainaut P (2018) Revisiting tumor patterns and penetrance in germline TP53 mutation carriers: temporal phases of Li-Fraumeni syndrome. Curr Opin Oncol 30(1):23–29
Lalloo F, Varley J, Moran A, Ellis D, O’dair L, Pharoah P, Antoniou A, Hartley R, Shenton A, Seal S et al (2006) BRCA1, BRCA2 and TP53 mutations in very early-onset breast cancer with associated risks to relatives. Eur J Cancer 42(8):1143–1150
Mouchawar J, Korch C, Byers T, Pitts TM, Li E, McCredie MR, Giles GG, Hopper JL, Southey MC (2010) Population-based estimate of the contribution of TP53 mutations to subgroups of early-onset breast cancer: Australian breast cancer family study. Cancer Res 70(12):4795–4800
Kelsey JL, Gammon MD (1991) The epidemiology of breast cancer. CA Cancer J Clin 41(3):146–165
Awadelkarim KD, Arizzi C, Elamin EO, Hamad HM, De Blasio P, Mekki SO, Osman I, Biunno I, Elwali NE, Mariani-Costantini R et al (2008) Pathological, clinical and prognostic characteristics of breast cancer in Central Sudan versus Northern Italy: implications for breast cancer in Africa. Histopathology 52(4):445–456
Mariani-Costantini R (2013) Diagnosis: breast cancer screening in rural African communities. Nat Rev Clin Oncol 10(4):185–186
Jedy-Agba E, McCormack V, Adebamowo C, Dos-Santos-Silva I (2016) Stage at diagnosis of breast cancer in sub-Saharan Africa: a systematic review and meta-analysis. Lancet Glob Health 4(12):e923–e935
Abbad A, Baba H, Dehbi H, Elmessaoudi-Idrissi M, Elyazghi Z, Abidi O, Radouani F (2018) Genetics of breast cancer in African populations: a literature review. Glob Health Epidemiol Genom 3:e8
Macaulay S, Goodyear QC, Kruger M, Chen W, Essop F, Krause A (2018) The first two confirmed sub-Saharan African families with germline TP53 mutations causing Li-Fraumeni syndrome. Fam Cancer 17(4):607–613
Awadelkarim KD, Aceto G, Veschi S, Elhaj A, Morgano A, Mohamedani AA, Eltayeb EA, Abuidris D, Di Gioacchino M, Battista P et al (2007) BRCA1 and BRCA2 status in a Central Sudanese series of breast cancer patients: interactions with genetic, ethnic and reproductive factors. Breast Cancer Res Treat 102(2):189–199
Biunno I, Aceto G, Awadelkarim KD, Morgano A, Elhaj A, Eltayeb EA, Abuidris DO, Elwali NE, Spinelli C, De Blasio P et al (2014) BRCA1 point mutations in premenopausal breast cancer patients from Central Sudan. Fam Cancer 13(3):437–444
United Nations, Department of Economic and Social Affairs, Population Division (2017). World Fertility Data 2017 (POP/DB/Fert/Rev2017)
Verselis SJ, Rheinwald JG, Fraumeni JF, Li FP (2000) Novel p53 splice site mutations in three families with Li-Fraumeni syndrome. Oncogene 19(37):4230–4235
Petitjean A, Mathe E, Kato S, Ishioka C, Tavtigian SV, Hainaut P, Olivier M (2007) Impact of mutant p53 functional properties on TP53 mutation patterns and tumor phenotype: lessons from recent developments in the IARC TP53 database. Hum Mutat 28(6):622–629
Altshuler DM, Gibbs RA, Peltonen L, Dermitzakis E, Schaffner SF, Yu F, Bonnen PE, de Bakker PI, Deloukas P, Gabriel SB et al (2010) Integrating common and rare genetic variation in diverse human populations. Nature 467(7311):52–58
Sudan Nutrition Profile (2005) Food and Nutrition Division, Food and Agriculture Organization of the United Nations
Iafrate AJ, Feuk L, Rivera MN, Listewnik ML, Donahoe PK, Qi Y, Scherer SW, Lee C (2004) Detection of large-scale variation in the human genome. Nat Genet 36(9):949–951
van Heemst D, Mooijaart SP, Beekman M, Schreuder J, de Craen AJ, Brandt BW, Slagboom PE, Westendorp RG (2005) group LLs: variation in the human TP53 gene affects old age survival and cancer mortality. Exp Gerontol 40(1–2):11–15
Whibley C, Pharoah PD, Hollstein M (2009) p53 polymorphisms: cancer implications. Nat Rev Cancer 9(2):95–107
Dumont P, Leu JI, Della Pietra AC, George DL, Murphy M (2003) The codon 72 polymorphic variants of p53 have markedly different apoptotic potential. Nat Genet 33(3):357–365
Jeong BS, Hu W, Belyi V, Rabadan R, Levine AJ (2010) Differential levels of transcription of p53-regulated genes by the arginine/proline polymorphism: p53 with arginine at codon 72 favors apoptosis. FASEB J 24(5):1347–1353
Toyama T, Zhang Z, Nishio M, Hamaguchi M, Kondo N, Iwase H, Iwata H, Takahashi S, Yamashita H, Fujii Y (2007) Association of TP53 codon 72 polymorphism and the outcome of adjuvant therapy in breast cancer patients. Breast Cancer Res 9(3):R34
Basu S, Gnanapradeepan K, Barnoud T, Kung CP, Tavecchio M, Scott J, Watters A, Chen Q, Kossenkov AV, Murphy ME (2018) Mutant p53 controls tumor metabolism and metastasis by regulating PGC-1α. Genes Dev 32(3–4):230–243
Lawson JS, Glenn WK, Salyakina D, Delprado W, Clay R, Antonsson A, Heng B, Miyauchi S, Tran DD, Ngan CC et al (2015) Human Papilloma viruses and breast cancer. Front Oncol 5:277
Eltahir HA, Adam AA, Yahia ZA, Ali NF, Mursi DM, Higazi AM, Eid NA, Elhassan AM, Mohammed HS, Ibrahim ME (2012) p53 codon 72 arginine/proline polymorphism and cancer in Sudan. Mol Biol Rep 39(12):10833–10836
Sagne C, Marcel V, Amadou A, Hainaut P, Olivier M, Hall J (2013) A meta-analysis of cancer risk associated with the TP53 intron 3 duplication polymorphism (rs17878362): geographic and tumor-specific effects. Cell Death Dis 4:e492
Liu Q, Wuu J, Lambe M, Hsieh SF, Ekbom A, Hsieh CC (2002) Transient increase in breast cancer risk after giving birth: postpartum period with the highest risk (Sweden). Cancer Causes Control 13(4):299–305
Díaz-Cruz ES, Furth PA (2010) Deregulated estrogen receptor alpha and p53 heterozygosity collaborate in the development of mammary hyperplasia. Cancer Res 70(10):3965–3974
Acknowledgements
This paper is dedicated to the memory of Professor Piero Musiani, who facilitated KDA’s research stage at CeSI-MeT, G. d’Annunzio University.
Funding
This research was funded by MIUR 60% funds to G.A. and R.M-C. KDA was partly supported by a generous contribution from Cassa di Risparmio della Provincia di Chieti S.p.A., Chieti, Italy.
Author information
Authors and Affiliations
Contributions
G.A., C.M., and K.D.A. performed genetic analyses; K.D.A and N.E.E. recruited patients and controls and verified clinical and reproductive data; M.d.N., M.R.P., and F.V. performed analytical and statistical calculations and provided critical feedback; G.A. and RM-C designed the study; RM-C wrote the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Ethical approval
The study was approved by the Institutional Ethical Committees of the National Cancer Institute, University of Gezira (NCI-UG) and “G. d’Annunzio” University.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Aceto, G.M., Awadelkarim, K.D., Di Nicola, M. et al. Germline TP53 mutation spectrum in Sudanese premenopausal breast cancer patients: correlations with reproductive factors. Breast Cancer Res Treat 175, 479–485 (2019). https://doi.org/10.1007/s10549-019-05168-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-019-05168-1