Abstract
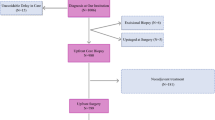
Medicaid beneficiaries with cancer are less likely to receive timely and high-quality care. This study examined whether differences in state-level Medicaid policies affect delays in time to surgery (TTS) among women diagnosed with breast cancer. Using 2006–2008 Medicaid data, we identified women aged 18–64 enrolled in Medicaid diagnosed with breast cancer. Analyses examined associations of state-specific Medicaid surgery reimbursements, Medicaid eligibility recertification period (annually vs. shorter) and required patient copayment on time from breast cancer diagnosis to receipt of breast surgery. Patients receiving neoadjuvant therapy were excluded. Separate multivariable regression analyses controlling for patient demographic characteristics and clustering by state were performed for breast conserving surgery (BCS), inpatient mastectomy, and outpatient mastectomy. The study included 7542 Medicaid beneficiaries with breast cancer: 3272 received BCS, 2156 outpatient mastectomy, and 2115 inpatient mastectomy. Higher Medicaid reimbursements for BCS were associated with decreased time from diagnosis to surgery. A 12-month (vs. <12 month) Medicaid eligibility recertification period was associated with decreased TTS for BCS and outpatient mastectomy. Black Medicaid beneficiaries (compared with non-Hispanic White beneficiaries) were more likely to experience delays for all three types of surgery, while Hispanic beneficiaries were more likely to experience delays only for outpatient mastectomy. State-level Medicaid policies and patient characteristics can affect receipt of timely surgery among Medicaid beneficiaries with breast cancer. As delays in surgery can increase morbidity and mortality, changes to state Medicaid policies and health system programs are needed to improve access to care for this vulnerable population.



Similar content being viewed by others
References
Park C (2016) Medicaid Spending Trends. https://www.macpac.gov/wp-content/uploads/2016/03/Medicaid-Spending-Trends.pdf. Accessed 7 June 2016
MACPAC (2015) MACStats: Medicaid and CHIP Data Book. https://www.macpac.gov/publication/macstats-medicaid-and-chip-data-book-2/. Accessed 7 June 2016
Coburn AF, Long SH, Marquis MS (1999) Effects of changing medicaid fees on physician participation and enrollee access. Inquiry 36:265–279
Cohen JW, Cunningham PJ (1995) Medicaid physician fee levels and children’s access to care. Health Aff (Millwood) 14:255–262
Cunningham PJ, Hadley J (2008) Effects of changes in incomes and practice circumstances on physicians’ decisions to treat charity and Medicaid patients. Milbank Q 86:91–123
Guy GP Jr (2010) The effects of cost sharing on access to care among childless adults. Health Serv Res 45:1720–1739
Resneck J Jr, Pletcher MJ, Lozano N (2004) Medicare, medicaid and access to dermatologists: the effect of patient insurance on appointment access and wait times. J Am Acad Dermatol 50:85–92
Shen YC, Zuckerman S (2005) The effect of medicaid payment generosity on access and use among beneficiaries. Health Serv Res 40:723–744
Halpern MT, Romaire MA, Haber SG, Tangka FK, Sabatino SA, Howard DH (2014) Impact of state-specific Medicaid reimbursement and eligibility policies on receipt of cancer screening. Cancer 120(19):3016–3024
Bleicher RJ, Ruth K, Sigurdson ER, Beck JR, Ross E, Wong YN, Patel SA, Boraas M, Chang EI, Topham NS, Egleston BL (2016) Time to surgery and breast cancer survival in the United States. JAMA Oncol 2(3):330–339
Colleoni M, Bonetti M, Coates AS, Castiglione-Gertsch M, Gelber RD, Price K, Rudenstam CM, Lindtner J, Collins J, Thürlimann B, Holmberg S, Veronesi A, Marini G, Goldhirsch A (2000) Early start of adjuvant chemotherapy may improve treatment outcome for premenopausal breast cancer patients with tumors not expressing estrogen receptors. The International Breast Cancer Study Group. J Clin Oncol 18(3):584–590
Hershman DL, Wang X, McBride R, Jacobson JS, Grann VR, Neugut AI (2006) Delay of adjuvant chemotherapy initiation following breast cancer surgery among elderly women. Breast Cancer Res Treat 99(3):313–321
Smith EC, Ziogas A, Anton-Culver H (2013) Delay in surgical treatment and survival after breast cancer diagnosis in young women by race/ethnicity. JAMA Surg 148(6):516–523
Chavez-MacGregor M, Clarke CA, Lichtensztajn DY, Giordano SH (2016) Delayed initiation of adjuvant chemotherapy among patients with breast cancer. JAMA Oncol 2(3):322–329
Gagliato Dde M, Gonzalez-Angulo AM, Lei X, Theriault RL, Giordano SH, Valero V, Hortobagyi GN, Chavez-Macgregor M (2014) Clinical impact of delaying initiation of adjuvant chemotherapy in patients with breast cancer. J Clin Oncol 32(8):735–744
Wu XC, Lund MJ, Kimmick GG, Richardson LC, Sabatino SA, Chen VW, Fleming ST, Morris CR, Huang B, Trentham-Dietz A, Lipscomb J (2012) Influence of race, insurance, socioeconomic status and hospital type on receipt of guideline-concordant adjuvant systemic therapy for locoregional breast cancers. J Clin Oncol 30(2):142–150
Fedewa SA, Edge SB, Stewart AK, Halpern MT, Marlow NM, Ward EM (2011) Race and ethnicity are associated with delays in breast cancer treatment 2003–2006. J Health Care Poor Underserved 22(1):128–141
Mosunjac M, Park J, Strauss A, Birdsong G, Du V, Rizzo M, Gabram SG, Lund MJ (2012) Time to treatment for patients receiving BCS in a public and a private university hospital in Atlanta. Breast J 18(2):163–167
Ward E, Halpern M, Schrag N, Cokkinides V, DeSantis C, Bandi P, Siegel R, Stewart A, Jemal A (2008) Association of insurance with cancer care utilization and outcomes. CA Cancer J Clin 58(1):9–31
Elmore JG, Nakano CY, Linden HM, Reisch LM, Ayanian JZ, Larson EB (2005) Racial inequities in the timing of breast cancer detection, diagnosis and initiation of treatment. Med Care 43(2):141–148
Gorin SS, Heck JE, Cheng B, Smith SJ (2006) Delays in breast cancer diagnosis and treatment by racial/ethnic group. Arch Intern Med 166(20):2244–2252
Gwyn K, Bondy ML, Cohen DS, Lund MJ, Liff JM, Flagg EW, Brinton LA, Eley JW, Coates RJ (2004) Racial differences in diagnosis, treatment and clinical delays in a population-based study of patients with newly diagnosed breast carcinoma. Cancer 100(8):1595–1604
Kroenke CH, Rosner B, Chen WY, Kawachi I, Colditz GA, Holmes MD (2004) Functional impact of breast cancer by age at diagnosis. J Clin Oncol 22(10):1849–1856
Rosenberg SM, Newman LA, Partridge AH (2015) Breast cancer in young women: rare disease or public health problem? JAMA Oncol 1(7):877–878
Koroukian SM, Cooper GS, Rimm AA (2003) Ability of medicaid claims data to identify incident cases of breast cancer in the ohio medicaid population. Health Serv Res 38(3):947–960
Nattinger AB, Laud PW, Bajorunaite R, Sparapani RA, Freeman JL (2004) An algorithm for the use of medicare claims data to identify women with incident breast cancer. Health Serv Res 39(6 Pt 1):1733–1749
Warren JL, Feuer E, Potosky AL, Riley GF, Lynch CF (1999) Use of medicare hospital and physician data to assess breast cancer incidence. Med Care 37(5):445–456
Ku L, MacTaggart P, Pervez F, Rosenbaum S (2009) Improving medicaid’s continuity of coverage and quality of care. Association for Community Affiliated Plans, Washington DC. http://www.communityplans.net/Portals/0/ACAP%20Docs/Improving%20Medicaid%20Final%20070209.pdf. Accessed 7 June 2016
MACPAC. Report to the Congress on Medicaid and CHIP, Chapter 2 (2014) https://www.macpac.gov/wp-content/uploads/2015/01/Promoting_Continuity_of_Medicaid_Coverage_among_Adults_under_65.pdf. Accessed 7 June 2016
Sommers BD, Rosenbaum S (2011) Issues in health reform: how changes in eligibility may move millions back and forth between medicaid and insurance exchanges. Health Aff (Millwood) 30(2):228–236
Deyo RA, Cherkin DC, Ciol MA (1992) Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol 45(6):613–619
Asplin BR, Rhodes KV, Levy H, Lurie N, Crain AL, Carlin BP, Kellermann AL (2005) Insurance status and access to urgent ambulatory care follow-up appointments. JAMA 294(10):1248–1254
Hall AG, Lemak CH, Steingraber H, Schaffer S (2008) Expanding the definition of access: it isn’t just about health insurance. J Health Care Poor Underserved 19(2):625–638
Resneck JS Jr, Isenstein A, Kimball AB (2006) Few medicaid and uninsured patients are accessing dermatologists. J Am Acad Dermatol 55(6):1084–1088
Dall TM, Storm MV, Chakrabarti R, Drogan O, Keran CM, Donofrio PD, Henderson VW, Kaminski HJ, Stevens JC, Vidic TR (2013) Supply and demand analysis of the current and future US neurology workforce. Neurology 81(5):470–478
Funding
This study was supported by the American Cancer Society (Grant # RSGI-12-009-01-CHPS).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Halpern, M.T., Schrag, D. Effects of state-level medicaid policies and patient characteristics on time to breast cancer surgery among medicaid beneficiaries. Breast Cancer Res Treat 158, 573–581 (2016). https://doi.org/10.1007/s10549-016-3879-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-016-3879-8