Abstract
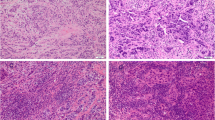
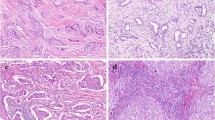
The purpose of the present study was to determine the optimal threshold for stromal tumor-infiltrating lymphocytes (TILs) and investigate its predictive and prognostic value in HER2-positive breast cancer treated with trastuzumab-based neoadjuvant chemotherapy (NAC). Levels of stromal TILs were evaluated using hematoxylin and eosin-stained sections of core biopsies from 116 patients. We investigated the correlation between stromal TILs and pathological response to identify its optimal threshold. Using receiver operating characteristic curve analysis, a 30 % threshold best discriminated pathological complete response (pCR) from non-pCR subgroups (P < 0.001). Lymphocyte-rich breast cancer (LRBC) was defined as having ≥30 % stromal TILs level, and was used for analysis. For analyses of predictive factors, multivariate analysis indicated that LRBC was a strong predictor of pCR with an odds ratio of 5.23 (P < 0.001). Negative hormone receptor (HR) status was also significantly associated with pCR (P = 0.028). LRBC significantly predicted pCR in both HR-positive and HR-negative tumors (P = 0.016 and 0.006, respectively). For survival analyses, LRBC was the only independent predictor of improved event-free survival (EFS) among baseline clinicopathological factors in multivariate analysis (P = 0.012). When pathological response was included, both LRBC and pCR were independent predictors of better EFS (P = 0.040 and 0.045, respectively). LRBC significantly predicted longer EFS in the non-pCR subgroup (P = 0.018), whereas LRBC was not significantly associated with EFS in the pCR subgroup (P = 0.825). A 30 % threshold for stromal TILs optimally identified response to trastuzumab-based NAC in HER2-positive breast cancer; its predictive and prognostic value was also validated in our study.






Similar content being viewed by others
References
Kohler BA, Sherman RL, Howlader N et al (2015) Annual report to the nation on the status of cancer, 1975-2011, featuring incidence of breast cancer subtypes by race/ethnicity, poverty, and state. J Natl Cancer Inst 107:djv048. doi:10.1093/jnci/djv048
Ross JS, Slodkowska EA, Symmans WF et al (2009) The HER-2 receptor and breast cancer: ten years of targeted anti-HER-2 therapy and personalized medicine. Oncologist 14:320–368. doi:10.1634/theoncologist.2008-0230
Moja L, Tagliabue L, Balduzzi S et al (2012) Trastuzumab containing regimens for early breast cancer. Cochrane Database Syst Rev 4:CD006243. doi:10.1002/14651858.CD006243.pub2
Buzdar AU, Ibrahim NK, Francis D et al (2005) Significantly higher pathologic complete remission rate after neoadjuvant therapy with trastuzumab, paclitaxel, and epirubicin chemotherapy: results of a randomized trial in human epidermal growth factor receptor 2-positive operable breast cancer. J Clin Oncol 23:3676–3685. doi:10.1200/JCO.2005.07.032
Gianni L, Eiermann W, Semiglazov V et al (2010) Neoadjuvant chemotherapy with trastuzumab followed by adjuvant trastuzumab versus neoadjuvant chemotherapy alone, in patients with HER2-positive locally advanced breast cancer (the NOAH trial): a randomised controlled superiority trial with a parallel HER2-negative cohort. Lancet 375:377–384. doi:10.1016/S0140-6736(09)61964-4
Gianni L, Eiermann W, Semiglazov V et al (2014) Neoadjuvant and adjuvant trastuzumab in patients with HER2-positive locally advanced breast cancer (NOAH): follow-up of a randomised controlled superiority trial with a parallel HER2-negative cohort. Lancet Oncol 15:640–647. doi:10.1016/S1470-2045(14)70080-4
Untch M, Fasching PA, Konecny GE et al (2011) Pathologic complete response after neoadjuvant chemotherapy plus trastuzumab predicts favorable survival in human epidermal growth factor receptor 2-overexpressing breast cancer: results from the TECHNO trial of the AGO and GBG study groups. J Clin Oncol 29:3351–3357. doi:10.1200/JCO.2010.31.4930
Denkert C, Loibl S, Noske A et al (2010) Tumor-associated lymphocytes as an independent predictor of response to neoadjuvant chemotherapy in breast cancer. J Clin Oncol 28:105–113. doi:10.1200/JCO.2009.23.7370
Denkert C, von Minckwitz G, Brase JC et al (2015) Tumor-infiltrating lymphocytes and response to neoadjuvant chemotherapy with or without carboplatin in human epidermal growth factor receptor 2-positive and triple-negative primary breast cancers. J Clin Oncol 33:983–991. doi:10.1200/JCO.2014.58.1967
Loi S, Michiels S, Salgado R et al (2014) Tumor infiltrating lymphocytes are prognostic in triple negative breast cancer and predictive for trastuzumab benefit in early breast cancer: results from the FinHER trial. Ann Oncol 25:1544–1550. doi:10.1093/annonc/mdu112
Salgado R, Denkert C, Campbell C et al (2015) Tumor-infiltrating lymphocytes and associations with pathological complete response and event-free survival in HER2-positive early-stage breast cancer treated with lapatinib and trastuzumab: a secondary analysis of the NeoALTTO trial. JAMA Oncol 1:448–454. doi:10.1001/jamaoncol.2015.0830
Ono M, Tsuda H, Shimizu C et al (2012) Tumor-infiltrating lymphocytes are correlated with response to neoadjuvant chemotherapy in triple-negative breast cancer. Breast Cancer Res Treat 132:793–805. doi:10.1007/s10549-011-1554-7
Salgado R, Denkert C, Demaria S et al (2015) The evaluation of tumor-infiltrating lymphocytes (TILs) in breast cancer: recommendations by an International TILs Working Group 2014. Ann Oncol 26:259–271. doi:10.1093/annonc/mdu450
Loi S, Sirtaine N, Piette F et al (2013) Prognostic and predictive value of tumor-infiltrating lymphocytes in a phase III randomized adjuvant breast cancer trial in node-positive breast cancer comparing the addition of docetaxel to doxorubicin with doxorubicin-based chemotherapy: BIG 02-98. J Clin Oncol 31:860–867. doi:10.1200/JCO.2011.41.0902
Issa-Nummer Y, Darb-Esfahani S, Loibl S et al (2013) Prospective validation of immunological infiltrate for prediction of response to neoadjuvant chemotherapy in HER2-negative breast cancer–a substudy of the neoadjuvant GeparQuinto trial. PLoS ONE 8:e79775. doi:10.1371/journal.pone.0079775
Vaz-Luis I, Winer EP, Lin NU (2013) Human epidermal growth factor receptor-2-positive breast cancer: does estrogen receptor status define two distinct subtypes? Ann Oncol 24:283–291. doi:10.1093/annonc/mds286
Lee HJ, Park IA, Park SY et al (2014) Two histopathologically different diseases: hormone receptor-positive and hormone receptor-negative tumors in HER2-positive breast cancer. Breast Cancer Res Treat 145:615–623. doi:10.1007/s10549-014-2983-x
Wang Y-C, Morrison G, Gillihan R et al (2011) Different mechanisms for resistance to trastuzumab versus lapatinib in HER2-positive breast cancers—role of estrogen receptor and HER2 reactivation. Breast Cancer Res 13:R121. doi:10.1186/bcr3067
von Minckwitz G, Untch M, Blohmer J-U et al (2012) Definition and impact of pathologic complete response on prognosis after neoadjuvant chemotherapy in various intrinsic breast cancer subtypes. J Clin Oncol 30:1796–1804. doi:10.1200/JCO.2011.38.8595
Cortazar P, Zhang L, Untch M et al (2014) Pathological complete response and long-term clinical benefit in breast cancer: the CTNeoBC pooled analysis. Lancet 384:164–172. doi:10.1016/S0140-6736(13)62422-8
Takada M, Ishiguro H, Nagai S et al (2014) Survival of HER2-positive primary breast cancer patients treated by neoadjuvant chemotherapy plus trastuzumab: a multicenter retrospective observational study (JBCRG-C03 study). Breast Cancer Res Treat 145:143–153. doi:10.1007/s10549-014-2907-9
Untch M, Rezai M, Loibl S et al (2010) Neoadjuvant treatment with trastuzumab in HER2-positive breast cancer: results from the GeparQuattro study. J Clin Oncol 28:2024–2031. doi:10.1200/JCO.2009.23.8451
Luporsi E, André F, Spyratos F et al (2012) Ki-67: level of evidence and methodological considerations for its role in the clinical management of breast cancer: analytical and critical review. Breast Cancer Res Treat 132:895–915. doi:10.1007/s10549-011-1837-z
Denkert C, Loibl S, Muller BM et al (2013) Ki67 levels as predictive and prognostic parameters in pretherapeutic breast cancer core biopsies: a translational investigation in the neoadjuvant GeparTrio trial. Ann Oncol 24:2786–2793. doi:10.1093/annonc/mdt350
Bianchini G, Gianni L (2014) The immune system and response to HER2-targeted treatment in breast cancer. Lancet Oncol 15:e58–e68. doi:10.1016/S1470-2045(13)70477-7
Acknowledgments
This work was supported by research grants from the Beijing Municipal Science & Technology Commission (Nos. D090507043409010 and Z131107002213007) and from the Beijing Municipal Commission of Health and Family Planning (No. 2009-1011).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare.
Rights and permissions
About this article
Cite this article
Liu, S., Duan, X., Xu, L. et al. Optimal threshold for stromal tumor-infiltrating lymphocytes: its predictive and prognostic value in HER2-positive breast cancer treated with trastuzumab-based neoadjuvant chemotherapy. Breast Cancer Res Treat 154, 239–249 (2015). https://doi.org/10.1007/s10549-015-3617-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-015-3617-7