Abstract
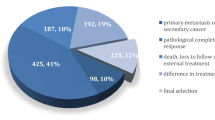
The purpose of this study was to investigate the correlation of T-cadherin expression with clinicopathological features and prognosis in patients with axillary lymph node-positive breast cancer. Based on the immunohistochemistry results, all 142 patients with operable axillary lymph node-positive breast cancer were divided into the T-cadherin-negative and T-cadherin-positive groups. Clinical data including the association of T-cadherin expression with clinicopathological features and prognosis were analyzed using the Chi square test and Fisher’s exact test using SPSS 13.0 software. The impact of T-cadherin expression on the 5-year disease-free survival (DFS) and the 5-year overall survival (OS) of these patients was measured using the log-rank test. DFS and OS were analyzed using both Kaplan–Meier function and Cox regression analyses. Compared with the T-cadherin-positive group (55.07, 28.99, and 13.4 %, respectively; P = 0.030, P = 0.0132, and P = 0.009), tumor size >2 cm, lymph-vascular invasion, and pathological stage III disease were seen more frequently in the T-cadherin-negative group (72.60, 49.32, and 31.51 %, respectively). Both 5-year DFS and 5-year OS were poorer in the T-cadherin-negative group than in the T-cadherin-positive group (log-rank test = 9.295, P = 0.002; log-rank test = 5.718, P = 0.017). On multivariate analysis, T-cadherin-negative expression remained an independent prognostic factor for DFS (P = 0.002) but not for OS (P = 0.067). Our results suggested that negative T-cadherin expression has a worse prognosis in patients with axillary lymph node-positive breast cancer.


Similar content being viewed by others
References
Fan L, Strasser-Weippl K, Li JJ, St Louis J, Finkelstein DM, Yu KD, Chen WQ, Shao ZM, Goss PE (2014) Breast cancer in China. Lancet Oncol 15(7):279–289. doi:10.1016/S1470-2045(13)70567-9
Won HS, Lee KE, Sung SH, Choi MY, Jo JY, Nam EM, Mun YC, Seong CM, Lee SN (2014) Topoisomerase II alpha and microtubule-associated protein- tau as a predictive marker in axillary lymph node positive breast cancer. Tumori 100(1):80–86. doi:10.1700/1430.15820
Munzone E, Bagnardi V, Rotmensz N, Sporchia A, Mazza M, Pruneri G, Intra M, Sciandivasci A, Gentilini O, Luini A, Viale G, Veronesi P, Colleoni M (2014) Prognostic relevance of peritumoral vascular invasion in immunohistochemically defined subtypes of node-positive breast cancer. Breast Cancer Res Treat 146(3):573–582. doi:10.1007/s10549-014-3043-2
Yip CH, Taib NA, Tan GH, Ng KL, Yoong BK, Choo WY (2009) Predictors of axillary lymph node metastases in breast cancer: is there a role for minimal axillary surgery? World J Surg 33(1):54–57. doi:10.1007/s00268-008-9782-7
Sakakibara M, Fujimori T, Miyoshi T, Nagashima T, Fujimoto H, Suzuki HT, Ohki Y, Fushimi K, Yokomizo J, Nakatani Y, Miyazaki M (2012) Aldehyde dehydrogenase 1-positive cells in axillary lymph node metastases after chemotherapy as a prognostic factor in patients with lymph node-positive breast cancer. Cancer 118(16):3899–3910. doi:10.1002/cncr.26725
Elkhodary TR, Ebrahim MA, Hatata EE, Niazy NA (2014) Prognostic value of lymph node ratio in node-positive breast cancer in Egyptian patients. J Egypt Natl Canc Inst 26(1):31–35. doi:10.1016/j.jnci.2013.10.001
Andrews JL, Kim AC, Hens JR (2012) The role and function of cadherins in the mammary gland. Breast Cancer Res 14(1):203. doi:10.1186/bcr3065
Stemmler MP (2008) Cadherins in development and cancer. Mol BioSyst 4(8):835–850. doi:10.1039/B719215K
Gheldof A, Berx G (2013) Cadherins and epithelial-to-mesenchymal transition. Prog Mol Biol Transl Sci 116:317–336. doi:10.1016/B978-0-12-394311-8.00014-5
Guillaume E, Comunale F, Do Khoa N, Planchon D, Bodin S, Gauthier-Rouviere C (2013) Flotillin microdomains stabilize cadherins at cell–cell junctions. J Cell Sci 126(22):5293–5304. doi:10.1016/B978-0-12-394311-8.00014-5
Hebbard LW, Garlatti M, Young LJ, Cardiff RD, Oshima RG, Ranscht B (2008) T- cadherin supports angiogenesis and adiponectin association with the vasculature in a mouse mammary tumor model. Cancer Res 68(5):1407–1416. doi:10.1158/0008-5472.CAN-07-2953
Philippova M, Pfaff D, Kyriakakis E, Buechner SA, Iezzi G, Spagnoli GC, Schoenenberger AW, Erne P, Resink TJ (2013) T- cadherin loss promotes experimental metastasis of squamous cell carcinoma. Eur J Cancer 49(8):2048–2058. doi:10.1016/j.ejca.2012.12.026
Adachi Y, Takeuchi T, Nagayama T, Ohtsuki Y, Furihata M (2009) Zeb1- mediated T- cadherin repression increases the invasive potential of gallbladder cancer. FEBS Lett 583(2):430–436. doi:10.1016/j.febslet.2008.12.042
Takeuchi T, Liang SB, Ohtsuki Y (2002) Downregulation of expression of a novel cadherin molecule, T- cadherin, in basal cell carcinoma of the skin. Mol Carcinog 35(4):173–179. doi:10.1002/mc.10088
Mukoyama Y, Utani A, Matsui S, Zhou S, Miyachi Y, Matsuyoshi N (2007) T- cadherin enhances cell-matrix adhesiveness by regulating beta1 integrin trafficking in cutaneous squamous carcinoma cells. Genes Cells 12(6):787–796. doi:10.1111/j.1365-2443.2007.01092.x
Kuphal S, Martyn AC, Pedley J, Crowther LM, Bonazzi VF, Parsons PG, Bosserhoff AK, Hayward NK, Boyle GM (2009) H- cadherin expression reduces invasion of malignant melanoma. Pigment Cell Melanoma Res 22(3):296–306. doi:10.1111/j.1755-148X.2009.00568.x
Ellmann L, Joshi MB, Resink TJ, Bosserhoff AK, Kuphal S (2012) BRN2 is a transcriptional repressor of CDH13 (T- cadherin) in melanoma cells. Invest 92(12):1788–1800. doi:10.1038/labinvest.2012.140
Makarla PB, Saboorian MH, Ashfaq R, Toyooka KO, Toyooka S, Minna JD, Gazdar AF, Schorge JO (2005) Promoter hypermethylation profile of ovarian epithelial neoplasms. Clin Cancer Res 11(15):5365–5369. doi:10.1158/1078-0432.CCR-04-2455
Hibi K, Kodera Y, Ito K, Akiyama S, Nakao A (2004) Methylation pattern of CDH13 gene in digestive tract cancers. Br J Cancer 91(6):1139–1142. doi:10.1038/sj.bjc.6602095
Tang Y, Dai Y, Huo J (2012) Decreased expression of T- cadherin is associated with gastric cancer prognosis. Hepatogastroenterology 59(116):1294–1298. doi:10.5754/hge12016
Kim DS, Kim MJ, Lee JY, Kim YZ, Kim EJ, Park JY (2007) Aberrant methylation of E-cadherin and H- cadherin genes in nonsmall cell lung cancer and its relation to clinicopathologic features. Cancer 11(12):2785–2792. doi:10.1002/cncr.23113
Takeuchi T, Misaki A, Chen BK, Ohtsuki Y (1999) H- cadherin expression in breast cancer. Histopathology 35(1):87–88
Toyooka KO, Toyooka S, Virmani AK, Sathyanarayana UG, Euhus DM, Gilcrease M, Minna JD, Gazdar AF (2001) Loss of expression and aberrant methylation of the CDH13 (H-cadherin) gene in breast and lung carcinomas. Cancer Res 61(11):4556–4560
Andreeva AV, Kutuzov MA (2010) Cadherin 13 in cancer. Genes Chromosomes Cancer 49(9):775–790. doi:10.1002/gcc.20787
Ciatto C, Bahna F, Zampieri N, VanSteenhouse HC, Katsamba PS, Ahlsen G, Harrison OJ, Brasch J, Jin X, Posy S, Vendome J, Ranscht B, Jessell TM, Honig B, Shapiro L (2010) T- cadherin structures reveal a novel adhesive binding mechanism. Nat Struct Mol Biol 17(3):339–347. doi:10.1038/nsmb.1781
Lee SW (1996) H- cadherin, a novel cadherin with growth inhibitory functions and diminished expression in human breast cancer. Nat Med 2(7):776–782
Celebiler Cavusoglu A, Kilic Y, Saydam S, Canda T, Başkan Z, Sevinc AI, Sakizli M (2009) Predicting invasive phenotype with CDH1, CDH13, CD44, and TIMP3 gene expression in primary breast cancer. Cancer Sci 100(12):2341–2345. doi:10.1111/j.1349-7006.2009.01333.x
Feng W, Orlandi R, Zhao N, Carcangiu ML, Tagliabue E, Xu J, Bast RC Jr, Yu Y (2010) Tumor suppressor genes are frequently methylated in lymph node metastases of breast cancers. BMC Cancer 20(10):378
Wang Y, Yin Q, Yu Q, Zhang J, Liu Z, Wang S, Lv S, Niu Y (2011) A retrospective study of breast cancer subtypes:the risk of relapse and the relations with treatments. Breast Cancer Res Treat 130(2):489–498. doi:10.1007/s10549-011-1709-6
Takahashi T, Saegusa S, Sumino H, Nakahashi T, Iwai K, Morimoto S, Nojima T, Kanda T (2005) Adiponectin, T- cadherin and tumour necrosis factor-alpha in damaged cardiomyocytes from autopsy specimens. J Int Med Res 33(2):236–244
Wang M, Kong D, Zhou Y, Wang W (2014) Expression and predictive value of prognosis of T-cadherin in breast cancer. Chin J Oper Proc Gen Surg 8(2):157–160
Qasim BJ, Ali HH, Hussein AG (2013) Immunohistochemical expression of matrix metalloproteinase-7 in human colorectal adenomas using specified automated cellular image analysis system: a clinicopathological study. Saudi J Gastroenterol. 19(1):23–27
Cimino-Mathews A, Hicks JL, Illei PB et al (2012) Androgen receptor expression is usually maintained in initial surgically resected breast cancer metastases but is often lost in end-stage metastases found at autopsy. Hum Pathol 43:1003–1011
Acknowledgments
This work was supported by the Science and Technology Development Plan of Jining No.1 People’s Hospital.
Conflict of interest
The authors declare no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kong, Dd., Yang, J., Li, L. et al. T-cadherin association with clinicopathological features and prognosis in axillary lymph node-positive breast cancer. Breast Cancer Res Treat 150, 119–126 (2015). https://doi.org/10.1007/s10549-015-3302-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-015-3302-x