Abstract
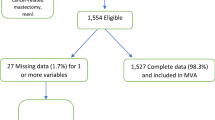
For women with breast cancer who undergo mastectomy, immediate breast reconstruction (IR) offers a cosmetic and psychological advantage. We evaluated the association between demographic, hospital, surgeon and insurance factors and receipt of IR. We conducted a retrospective hospital-based analysis with the Perspective database. Women who underwent a mastectomy for invasive breast cancer (IBC) and ductal carcinoma in situ (DCIS) from 2000 to 2010 were included. Logistic regression analysis was used to determine factors predictive of IR. Analyses were stratified by age (<50 vs. ≥50) and IBC versus DCIS. Of the 108,992 women with IBC who underwent mastectomy, 30,859 (28.3 %) underwent IR, as compared to 6,501 (44.2 %) of the 14,710 women with DCIS who underwent mastectomy underwent IR. In a multivariable model for IBC, increasing age, black race, being married, rural location, and increased comorbidities were associated with decreased IR. Odds ratios (OR) of IR increased with commercial insurance (OR 3.38) and Medicare (OR 1.66) insurance (vs. self-pay), high surgeon-volume (OR 1.19), high hospital-volume (OR 2.24), and large hospital size (OR 1.20). The results were identical for DCIS, and by age category. The absolute difference between the proportion of patients who received IR with commercial insurance compared to other insurance, increased over time. Immediate in-hospital complication rates were higher for flap reconstruction compared to implant or no reconstruction (15.2, 4.0, and 6.1 %, respectively, P < .0001). IR has increased significantly over time; however, modifiable factors such as insurance status, hospital size, hospital location, and physician volume strongly predict IR. Public policy should ensure that access to reconstructive surgery is universally available.


Similar content being viewed by others
References
Dean C, Chetty U, Forrest AP (1983) Effects of immediate breast reconstruction on psychosocial morbidity after mastectomy. Lancet 1(8322):459–462
Wilkins EG, Cederna PS, Lowery JC, Davis JA, Kim HM, Roth RS, Goldfarb S, Izenberg PH, Houin HP, Shaheen KW (2000) Prospective analysis of psychosocial outcomes in breast reconstruction: one-year postoperative results from the Michigan Breast Reconstruction Outcome Study. Plast Reconstr Surg 106(5):1014–1025 (discussion 1026–1017)
Alderman AK, Wilkins EG, Lowery JC, Kim M, Davis JA (2000) Determinants of patient satisfaction in postmastectomy breast reconstruction. Plast Reconstr Surg 106(4):769–776
Atisha D, Alderman AK, Lowery JC, Kuhn LE, Davis J, Wilkins EG (2008) Prospective analysis of long-term psychosocial outcomes in breast reconstruction: two-year postoperative results from the Michigan Breast Reconstruction Outcomes Study. Ann Surg 247(6):1019–1028
Al-Ghazal SK, Sully L, Fallowfield L, Blamey RW (2000) The psychological impact of immediate rather than delayed breast reconstruction. Eur J Surg Oncol 26(1):17–19
Fernandez-Frias AM, Aguilar J, Sanchez JA, Merck B, Pinero A, Calpena R (2009) Immediate reconstruction after mastectomy for breast cancer: which factors affect its course and final outcome? J Am Coll Surg 208(1):126–133
Petit JY, Gentilini O, Rotmensz N, Rey P, Rietjens M, Garusi C, Botteri E, De Lorenzi F, Martella S, Bosco R et al (2008) Oncological results of immediate breast reconstruction: long term follow-up of a large series at a single institution. Breast Cancer Res Treat 112(3):545–549
Morrow M, Scott SK, Menck HR, Mustoe TA, Winchester DP (2001) Factors influencing the use of breast reconstruction postmastectomy: a National Cancer Database study. J Am Coll Surg 192(1):1–8
Reuben BC, Manwaring J, Neumayer LA (2009) Recent trends and predictors in immediate breast reconstruction after mastectomy in the United States. Am J Surg 198(2):237–243
Christian CK, Niland J, Edge SB, Ottesen RA, Hughes ME, Theriault R, Wilson J, Hergrueter CA, Weeks JC (2006) A multi-institutional analysis of the socioeconomic determinants of breast reconstruction: a study of the National Comprehensive Cancer Network. Ann Surg 243(2):241–249
Kruper L, Holt A, Xu XX, Duan L, Henderson K, Bernstein L, Ellenhorn J (2011) Disparities in reconstruction rates after mastectomy: patterns of care and factors associated with the use of breast reconstruction in Southern California. Ann Surg Oncol 18:2158–2165
Tseng JF, Kronowitz SJ, Sun CC, Perry AC, Hunt KK, Babiera GV, Newman LA, Singletary SE, Mirza NQ, Ames FC et al (2004) The effect of ethnicity on immediate reconstruction rates after mastectomy for breast cancer. Cancer 101(7):1514–1523
Alderman AK, Hawley ST, Janz NK, Mujahid MS, Morrow M, Hamilton AS, Graff JJ, Katz SJ (2009) Racial and ethnic disparities in the use of postmastectomy breast reconstruction: results from a population-based study. J Clin Oncol 27(32):5325–5330
Morrow M, Mujahid M, Lantz PM, Janz NK, Fagerlin A, Schwartz K, Liu L, Deapen D, Salem B, Lakhani I et al (2005) Correlates of breast reconstruction: results from a population-based study. Cancer 104(11):2340–2346
Lagu T, Rothberg MB, Nathanson BH, Pekow PS, Steingrub JS, Lindenauer PK (2011) The relationship between hospital spending and mortality in patients with sepsis. Arch Intern Med 171(4):292–299
Lindenauer PK, Pekow P, Wang K, Mamidi DK, Gutierrez B, Benjamin EM (2005) Perioperative beta-blocker therapy and mortality after major noncardiac surgery. N Engl J Med 353(4):349–361
Lindenauer PK, Pekow PS, Lahti MC, Lee Y, Benjamin EM, Rothberg MB (2010) Association of corticosteroid dose and route of administration with risk of treatment failure in acute exacerbation of chronic obstructive pulmonary disease. JAMA 303(23):2359–2367
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40(5):373–383
Deyo RA, Cherkin DC, Ciol MA (1992) Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol 45(6):613–619
Hollenbeck BK, Wei Y, Birkmeyer JD (2007) Volume, process of care, and operative mortality for cystectomy for bladder cancer. Urology 69(5):871–875
Birkmeyer JD, Sun Y, Wong SL, Stukel TA (2007) Hospital volume and late survival after cancer surgery. Ann Surg 245(5):777–783
Rothberg MB, Pekow PS, Lahti M, Brody O, Skiest DJ, Lindenauer PK (2010) Antibiotic therapy and treatment failure in patients hospitalized for acute exacerbations of chronic obstructive pulmonary disease. JAMA 303(20):2035–2042
US Department of Labor Bureau of Labor Statistics Consumer Price Index (2011). ftp://ftp.bls.gov/pub/special.requests/cpi/cpiai.txt. Accessed September 1, 2011
Tuttle TM, Jarosek S, Habermann EB, Arrington A, Abraham A, Morris TJ, Virnig BA (2009) Increasing rates of contralateral prophylactic mastectomy among patients with ductal carcinoma in situ. J Clin Oncol 27(9):1362–1367
Tuttle TM, Habermann EB, Grund EH, Morris TJ, Virnig BA (2007) Increasing use of contralateral prophylactic mastectomy for breast cancer patients: a trend toward more aggressive surgical treatment. J Clin Oncol 25(33):5203–5209
D’Souza N, Darmanin G, Fedorowicz Z (2011) Immediate versus delayed reconstruction following surgery for breast cancer. Cochrane Database Syst Rev 7:CD008674
Marin-Gutzke M, Sanchez-Olaso A (2010) Reconstructive surgery in young women with breast cancer. Breast Cancer Res Treat 123(Suppl 1):67–74
Neyt MJ, Blondeel PN, Morrison CM, Albrecht JA (2005) Comparing the cost of delayed and immediate autologous breast reconstruction in Belgium. Br J Plast Surg 58(4):493–497
Harlan LC, Greene AL, Clegg LX, Mooney M, Stevens JL, Brown ML (2005) Insurance status and the use of guideline therapy in the treatment of selected cancers. J Clin Oncol 23(36):9079–9088
Bernard DS, Farr SL, Fang Z (2010) National estimates of out-of-pocket health care expenditure burdens among nonelderly adults with cancer: 2001 to 2008. J Clin Oncol 29(20):2821–2826
Du XL, Fang S, Vernon SW, El-Serag H, Shih YT, Davila J, Rasmus ML (2007) Racial disparities and socioeconomic status in association with survival in a large population-based cohort of elderly patients with colon cancer. Cancer 110(3):660–669
Sprague BL, Trentham-Dietz A, Gangnon RE, Ramchandani R, Hampton JM, Robert SA, Remington PL, Newcomb PA (2011) Socioeconomic status and survival after an invasive breast cancer diagnosis. Cancer 117(7):1542–1551
McBride RB, Lebwohl B, Hershman DL, Neugut AI (2010) Impact of socioeconomic status on extent of lymph node dissection for colon cancer. Cancer Epidemiol Biomarkers Prev 19(3):738–745
Mackillop WJ, Zhang-Salomons J, Groome PA, Paszat L, Holowaty E (1997) Socioeconomic status and cancer survival in Ontario. J Clin Oncol 15(4):1680–1689
Fobair P, Stewart SL, Chang S, D’Onofrio C, Banks PJ, Bloom JR (2006) Body image and sexual problems in young women with breast cancer. Psychooncology 15(7):579–594
Zebrack B, Bleyer A, Albritton K, Medearis S, Tang J (2006) Assessing the health care needs of adolescent and young adult cancer patients and survivors. Cancer 107(12):2915–2923
Bleyer A, Barr R (2009) Cancer in young adults 20 to 39 years of age: overview. Semin Oncol 36(3):194–206
Bleyer A (2007) Young adult oncology: the patients and their survival challenges. CA Cancer J Clin 57(4):242–255
Agarwal S, Pappas L, Neumayer L, Agarwal J (2011) An analysis of immediate postmastectomy breast reconstruction frequency using the surveillance, epidemiology, and end results database. Breast J 17(4):352–358
Alderman AK, Atisha D, Streu R, Salem B, Gay A, Abrahamse P, Hawley ST (2011) Patterns and correlates of postmastectomy breast reconstruction by US plastic surgeons: results from a national survey. Plast Reconstr Surg 127(5):1796–1803
Schrag D, Cramer LD, Bach PB, Cohen AM, Warren JL, Begg CB (2000) Influence of hospital procedure volume on outcomes following surgery for colon cancer. JAMA 284(23):3028–3035
Liu JH, Zingmond DS, McGory ML, SooHoo NF, Ettner SL, Brook RH, Ko CY (2006) Disparities in the utilization of high-volume hospitals for complex surgery. JAMA 296(16):1973–1980
Bilimoria KY, Bentrem DJ, Feinglass JM, Stewart AK, Winchester DP, Talamonti MS, Ko CY (2008) Directing surgical quality improvement initiatives: comparison of perioperative mortality and long-term survival for cancer surgery. J Clin Oncol 26(28):4626–4633
Keating NL, Kouri E, He Y, Weeks JC, Winer EP (2009) Racial differences in definitive breast cancer therapy in older women: are they explained by the hospitals where patients undergo surgery? Med Care 47(7):765–773
Acknowledgments
Dr. Hershman is the recipient of a Grant from the National Cancer Institute (NCI R01 CA134964). Ms. Richards is the recipient of a T32 fellowship (NCI CA09529).
Conflict of interest
The authors have no potential conflicts of interest to report.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hershman, D.L., Richards, C.A., Kalinsky, K. et al. Influence of health insurance, hospital factors and physician volume on receipt of immediate post-mastectomy reconstruction in women with invasive and non-invasive breast cancer. Breast Cancer Res Treat 136, 535–545 (2012). https://doi.org/10.1007/s10549-012-2273-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-012-2273-4