Abstract
For patients with metastatic breast cancer, we previously described that increased EZH2 expression levels were associated with an adverse outcome to tamoxifen therapy. Main objective of the present study is to investigate miR-26a and miR-101 levels, which both target EZH2, for their association with molecular pathways and with efficacy of tamoxifen as first-line monotherapy for metastatic breast cancer. Expression levels were measured using quantitative Real-Time Polymerase Chain Reaction (qRT-PCR) in primary breast cancer specimens of 235 estrogen receptor-α (ER)-positive patients. Pathway analysis was performed on microarray data available for 65 of these tumors. Logistic regression and Cox uni- and multivariate analysis were performed to relate expression levels with clinical benefit and time to progression (TTP). Increasing levels of miR-26a were significantly (P < 0.005) associated with both clinical benefit and prolonged TTP, whereas miR-101 was not. Cell cycle regulation and CCNE1 and CDC2 were the only significant overlapping pathway and genes differentially expressed between tumors with high and low levels of miR-26a and EZH2, respectively. In addition, increasing mRNA levels of CCNE1 (P < 0.05) and CDC2 (P < 0.001) were related to poor outcome. Multivariate analysis revealed miR-26a and CDC2 as an optimal set of markers associated with outcome on tamoxifen therapy, independently of traditional predictive factors. To summarize, only miR-26a levels are related with treatment outcome. Cell cycle regulation is the only overlapping pathway linked to miR-26a and EZH2 levels. Low mRNA levels of EZH2, CCNE1, and CDC2, and high levels of miR-26a are associated with favorable outcome on tamoxifen.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The anti-estrogen tamoxifen has been used for more than three decades for the treatment of estrogen receptor-α (ER)-positive breast cancer in both adjuvant and metastatic settings. The majority of breast tumors express ER, however, half of the patients with metastatic disease initially fail to respond to endocrine therapy, while the remaining patients will develop resistance during therapy. More insight into factors underlying tamoxifen resistance as well biomarkers to identify patients likely to benefit from tamoxifen is therefore needed.
We identified and validated an 81-gene signature that predicts tamoxifen resistance in patients with metastatic breast cancer [1, 2]. This signature included a member of the Enhancer of Zeste Homolog (EZH) family, which consists of EZH1 (OMIM 601674) and EZH2 (OMIM 601573). EZH2 is one of the polycomb proteins, a highly conserved group of chromatin modifiers known for their role in epigenetic memory and preservation of cellular characteristics [3]. Our in vitro studies showed that knockdown of EZH2 upregulates ER as a consequence of which sensitivity to anti-estrogen therapy increases [4]. In line with this, we have validated the predictive value of EZH2 and showed that low EZH2 levels were associated with favorable outcome on tamoxifen treatment in breast cancer patients with metastatic disease [4].
MicroRNAs (miRs) consist of a family of endogenously expressed small noncoding RNAs that target coding mRNAs to repress translation or induce degradation of their target mRNAs [5]. There is accumulating evidence that misregulation of miRs plays an important role in cancer. In breast cancer, miRs have been related with metastatic behavior, clinical outcome and ER status [6, 7]. Expression of several miRs in ER-positive breast cancer have also been associated with response to tamoxifen in cell lines (miR-221 and -222) [8], and in patients with metastatic disease treated with first-line tamoxifen (miR-30a, -30c, and -182) [9].
With respect to EZH2, miR target prediction tools have indicated that several miRs can target EZH2, but only two miRs, i.e., miR-26a and miR-101, have actually been shown to regulate EZH2 expression in different tissues [10, 11]. In the present study, we examined whether miR-26a and miR-101 were associated with EZH2 mRNA levels in breast cancer and with outcome on first-line tamoxifen therapy. In addition, using available whole genome mRNA data from a subset of tumors, the global testing approach (GTA) was performed to identify molecular pathways correlated with expression levels of miR-26a, miR-101, and EZH2 and to reveal genes, within these pathways, that associate with outcome on tamoxifen.
Patients and methods
Patients
Frozen breast tumor tissue specimens from female patients with primary operable breast cancer, who entered the clinic between 1981 and 1996 were analyzed. Follow-up, tumor staging, and response to therapy were performed as defined by standard International Union Against Cancer (Geneva, Switzerland) classification criteria [12]. This retrospective study was performed in accordance with the Code of Conduct of the Federation of Medical Scientific Societies in the Netherlands (http://www.fmwv.nl), and reported following the REMARK recommendations [13], wherever possible. The study has been approved by the medical ethics committee of the Erasmus MC Rotterdam, The Netherlands (MEC 02.953).
Tumor protein expression levels of ER and progesterone receptor (PgR) were determined and used to classify tumors as ER- and/or PgR-positive as described previously [4, 14]. The following criteria were applied to include breast tumor specimens for final analysis in this study: (1) sufficient frozen tumor material, (2) more than 30% epithelial tumor cell nuclei in haematoxylin/eosin-stained sections, and (3) specimen of good RNA quality according to predefined criteria [15]. After applying these criteria, 235 patients with ER-positive tumors, who had metastatic disease treated with tamoxifen as first-line therapy, were included in this study. From these 235 patients, 89 patients (38%) underwent breast-conserving lumpectomy and 146 patients modified mastectomy (62%). The median follow-up time of patients alive was 89 months, range 10–165 months. Hundred and sixty five patients (70%) did not receive prior adjuvant systemic therapy, while 42 patients (18%) were previously treated with adjuvant chemotherapy [25 patients (11%) with non-anthracycline-based (CMF) and 17 patients (7%) with anthracycline-based (FAC/FEC) regimens].
Twenty eight patients (12%) presented with distant metastases at initial diagnosis (M1 patients). Clinical benefit on first-line tamoxifen monotherapy, defined as a complete or partial response according to standard International Union Against Cancer (Geneva, Switzerland) classification criteria [12] or no change longer than 6 months after treatment initiation (stable disease), was observed in 148 patients (63%). Eleven patients (5%) showed a complete response, 33 (14%) a partial response, and 104 patients (44%) had stable disease. No clinical benefit occurred in 87 patients (37%). Time to progression (TTP) was defined as the time elapsed between initiation of tamoxifen therapy and first detection of disease progression.
Methods
Details of applied methodologies are available at Supplemental Methods. In brief, tissue processing, RNA isolation, cDNA synthesis, quantitative Real-Time Polymerase Chain Reaction (qRT-PCR), and expression data generation were performed as described previously [15]. For pathway analysis, samples with whole genome mRNA expression profiles available, measured on Affymetrix HG-U133A and Plus2 chips, were selected (N = 65, 28%) and only reliable, i.e., quality checked, probes (N = 10,520) were evaluated. Samples were grouped according to median expression levels of miR-26a, miR-101 or EZH2. The Global Test Approach (GTA) was used to identify KEGG/BioCarta biological pathways in genes co-expressed with the biomarker of interest [41]. Pathways were taken into account when P-values, after correction for multiple testing and resampling, were below 0.05 and genes with z-scores >1.96 were considered significant contributors to the pathways. The GTA package version 4.14.0 was run in the R version 2.9.0. Data analysis and statistics were performed as previously described [4]. Expression levels of miR-26a, miR-101, and EZH2, CCNE1, CDC2, ER, and PgR mRNA levels were transformed to reduce distribution skewness. Logistic regression analysis was used to compute the odds ratio (OR) for clinical benefit and the Cox proportional hazards model to calculate the hazard ratio (HR) for TTP. Computations were done with the STATA statistical package, release 11.1 (STATA Corp., College Station, TX). All P-values were two-sided, and P < 0.05 was considered as statistically significant.
Results
Associations with clinicopathological factors
In this study, we determined the miR-26a, miR-101, and EZH2 mRNA expression levels in 235 primary breast carcinomas. The median and interquartile ranges of expression levels for miR-26a were 0.99 and 0.41, for miR-101 were 1.03 and 0.81 and for EZH2 were 0.10 and 0.07. The miR-26a and miR-101 levels correlated with each other (r s = 0.43, P < 0.001) and showed an inverse relation with EZH2 mRNA levels (r s = −0.21 and r s = −0.15, respectively, P < 0.05). Expression levels of both miRs were not significantly related with age, tumor grade, tumor size, or nodal status (Table 1). Only miR-101 levels were associated with postmenopausal status (P = 0.036). The ER and PgR mRNA levels showed a significant positive correlation with those of miR-26a (r s = 0.21 and r s = 0.34, for both P < 0.002) and miR-101 (r s = 0.13, P = 0.04 and r s = 0.27, P < 0.001).
Associations with clinical benefit and time to progression
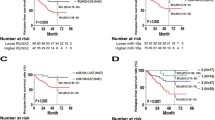
Expression levels of miR-26a, miR-101 and EZH2 mRNA levels were evaluated in uni- and multivariate analysis for their associations with clinical benefit (Supplemental Table 2) and TTP (Table 2) in patients with metastatic breast cancer treated with tamoxifen as first-line monotherapy. The miR-101 levels were not related with clinical benefit (OR = 0.84, P = 0.40) nor with TTP (Table 2). As continuous variable, increasing levels of miR-26a were significantly associated with clinical benefit (OR = 32.1, P < 0.001) and with favorable TTP (HR = 0.13, P < 0.001; Table 2). Increasing mRNA levels of EZH2 were related to lower chance of clinical benefit (OR = 0.61, P = 0.02) and shorter TTP (HR = 1.26, P = 0.02). Analysis of miR-26a and EZH2 categorized in thirds (i.e. three quantiles) showed that the third with highest levels of miR-26a was related to clinical benefit (OR = 4.10, P < 0.001) and with prolonged TTP (HR = 0.43, P < 0.001), whereas the third with the highest EZH2 levels correlated with treatment failure (OR = 0.34, P = 0.002) and shorter TTP (HR = 1.91, P < 0.001). Kaplan–Meier curves as function of categorized expression levels of miR-26a and EZH2 visualize their association with TTP (Fig. 1). The median differences in TTP were 6.5 months between patients with high and low expression levels for miR-26a and 5.6 months for those with high and low EZH2 expression levels. In multivariate analysis, when added separately to the base model of predictive factors, miR-26a and EZH2 were significantly associated with clinical benefit and TTP, both as continuous and as categorized variables. Patients with high miR-26a levels showed clinical benefit (OR = 3.31, P = 0.005) and the longest TTP (HR = 0.52, P < 0.001), whereas those with high EZH2 levels had less benefit (OR = 0.39, P = 0.02) and shorter TTP (HR = 1.80; P = 0.001). The results of the multivariate analysis show the independence of miR-26a and EZH2 from traditional predictive factors included in the base model.
Kaplan–Meier curves of TTP as a function of miR-26a, EZH2, CCNE1, and CDC2 expression levels. Patients were evenly divided into three groups according to their expression levels. Curves were generated as function of low, intermediate, and high miR-26a, EZH2, CCNE1, and CDC2 expression levels. Patients at risk at different time points are indicated
Pathway analysis for miR-26a and EZH2
In an exploratory pathway analysis with GTA, we evaluated 109 KEGG/BioCarta biological pathways and 10,520 mRNAs for differentially expressed pathways and genes. GTA identified only two pathways which significantly correlated with miR-26a, and 10 pathways with EZH2 mRNA expression (Table 3). The cyclins and cell cycle regulation pathway, and genes CCNE1 and CDC2 were the only overlapping pathway and genes between miR-26a and EZH2 that contributed significantly (Fig. 2). Increased expressions of CCNE1 and CDC2 were observed in samples with low miR-26a levels and in samples with high EZH2 levels.
Global testing approach result of the cyclins and cell cycle regulation pathway. This pathway was overlapping between miR-26a- and EZH2-related pathways. Red bars illustrate high expression levels of the pathway gene in samples with high miR-26a or EZH2 levels, whereas green bars indicate high expression levels in samples with low miR-26a or EZH2 levels. The number of vertical markers in a bar indicates the significance and the height of a bar the contribution of a gene to the pathway. The continuous line shows the threshold for significance; bars with more than two lines above this border are significantly (P < 0.05) differentially expressed genes within the pathway, which are also indicated with an asterisk. Only CCNE1 and CDC2 showed significant associations with both miR-26a and EZH2
To confirm this exploratory analysis, the predictive value of CCNE1 and CDC2 was evaluated by qRT-PCR. The median and interquartile mRNA levels were 0.03 and 0.03 for CCNE1 (N = 226), and 9.94 and 7.11 for CDC2 (N = 230), respectively. The mRNA levels of CCNE1 and CDC2 correlated with each other (r s = 0.44, P < 0.001) and showed a positive association with EZH2 mRNA levels (r s = 0.45 and r s = 0.57, for both P < 0.001) and an inverse relation with miR-26a (r s = −0.44 and r s = −0.30, respectively, for both P ≤ 0.001). The ER and PgR mRNA expression levels showed an inverse correlation with those of CCNE1 (r s = −0.14, P = 0.03 and r s = −0.24, P < 0.001) and CDC2 (r s = −0.07, P = 0.32 and r s = −0.27, (P < 0.001). Expression levels of CDC2 and CCNE1 were not related with age, menopausal status, tumor grade, tumor size, or nodal status (Table 1). In univariate analysis, increasing mRNA levels of CCNE1 were related to treatment failure (OR = 0.67, P = 0.005; Supplemental Table 2) and shorter TTP (HR = 1.27, P < 0.001; Table 2). In addition, increased expression of CDC2 was associated with poor clinical benefit (OR = 0.45, P < 0.001) and TTP (HR = 1.53, P < 0.001). In multivariate analysis, CCNE1 and CDC2, when added separately to the base model, were both independent from traditional predictive factors for their association with clinical benefit and TTP (Supplemental Table 2; Table 2). Categorized into thirds, Kaplan–Meier survival analysis showed that patients with higher mRNA levels of CCNE1 and CDC2 had a shorter TTP (Fig. 1). Compared to the group with low tumor levels of CCNE1, those with high levels of CNNE1 had an OR of 0.33 (P = 0.002) and a HR of 1.87 (P < 0.001), respectively. Patients with high tumor levels of CDC2 had an OR of 0.28 (P < 0.001) and even a HR of 2.07 (P < 0.001), respectively, compared with those with low tumor CDC2 levels. These results indicate that an activated cell cycle regulation pathway through increased expressions of CCNE1 and CDC2 is significantly associated with poor outcome on tamoxifen therapy. Moreover, two additional cyclins and cell cycle regulation pathway genes (E2F1 and CCNB1) were evaluated, next to CCNE2 (not in GTA because it failed quality control), to confirm the involvement of the cell cycle regulation pathway in the response to tamoxifen. All three genes showed a significant association with TTP in uni- and multivariate analyses as continuous variables, i.e., E2F1 had a HR of 1.38 (P = 0.013), CCNE2 had a HR of 1.38 (P < 0.001) and CCNB1 had a HR of 1.86 (P < 0.001) (Supplemental Table 3).
Multivariate analysis of miR-26a, EZH2, CCNE1, and CDC2
To determine a set of predictive biomarkers, the expression of miR-26a levels and of EZH2, CCNE1, and CDC2 mRNA levels were added simultaneously in a multivariate analysis to evaluate their relationship with TTP. Both CCNE1 and EZH2 mRNA levels lost their predictive value when included with miR-26a and CDC2, defining miR-26a and CDC2 levels as the set of predictive biomarkers associated with TTP. The HRs in the simultaneous analysis of miR-26a and CDC2 as continuous variables were 0.22 (P < 0.001) and 1.38 (P = 0.001), respectively (Table 2). Their contribution to the multivariate base model was independent from traditional predictive factors included in the model (Table 2). Converting miR-26a and CDC2 levels into a score followed by categorization into thirds resulted in a HR of 1.90 for the group with intermediate scores and a HR of 3.03 for the group with highest scores (see Supplemental Figure 1 for Kaplan–Meier survival curves).
Discussion
This study shows that miR-26a levels associate with outcome of metastatic disease on first-line tamoxifen monotherapy, whereas miR-101 does not. Patients with clinical benefit have high miR-26a and low EZH2 mRNA levels. Additionally, only the cell cycle regulation pathway with its genes CCNE1 and CDC2 overlap between miR-26a and EZH2 linked molecular pathways. These two genes also correlate with treatment outcome. The miR-26a and CDC2 levels that regulate EZH2 levels and activity were identified as a set of predictive biomarkers for treatment outcome.
Overexpression of EZH2 was observed in prostate and breast cancer in which it was associated with aggressive clinical behavior [16, 17]. We demonstrated that decreased EZH2 mRNA levels were predictive for favorable outcome on tamoxifen in metastatic breast cancer [4]. Both miR-26a and miR-101 repress EZH2 expression [10, 11, 18]. Although miR-26a and miR-101 expressions correlate with EZH2 levels in our current study, only miR-26a had a significant association with outcome on tamoxifen. Expression of miR-26a is repressed by estrogens in vitro and is induced in breast cancer patients treated with anti-estrogen neoadjuvant therapy [19] whereas miR-101 expression is upregulated by androgen stimulation [18], but is not regulated by estrogens [19, 20]. The fact that androgens stimulate miR-101 expression, whereas estrogens repress miR-26a expression needs to be elucidated, but suggests that EZH2 repression by miR-26a and miR-101 might be tissue as well as hormone dependent. That only miR-26a and not miR-101 has a relation with treatment outcome is because these miRs target many other genes. Of the genes predicted to be targets of miR-26a (1,012 targets) and miR-101 (1,198 targets), only a few (66 genes, including EZH2) are targeted by both miRs (data not shown). We cannot exclude another relevant gene for endocrine therapy outcome as specific miR-26a target which is not targeted by miR-101. This certainly needs further exploration but is not within the scope of the current study.
Our pathway analyses identified only the cell cycle regulation pathway to be correlated with miR-26a and EZH2 levels. The genes CDK7, CCNE1, CDC2, and CDKN2D for miR-26a and CCNB1, CCNE1, CDC2, CCND2, and E2F1 for EZH2 were differentially expressed within this pathway. CCNE2 and CDK2, important genes in this pathway, were not included in the analyses because their probes failed quality control. The association of EZH2 with cell cycle regulation is extensively reported [21, 22]. Moreover, the Targetscan algorithm predicted cyclins D2, E1, and E2 (CCND2, CCNE1, and CCNE2), and cyclin dependent kinase 6 (CDK6), which all play a role in the G1–S transition, as miR-26a targets [23]. Finally, estrogens that regulate G1 cyclin-dependent kinases [24] and tamoxifen has a cytostatic effect on breast cancer cells and arrest them in G0/G1 phase [25].
Based on our study, CCNE1 and CDC2 were the only overlapping genes for miR-26a and EZH2. We have shown earlier Cyclin E as prognostic marker for lymph node-negative breast cancer [26]. Now, we show that in the metastatic disease setting, high CCNE1 mRNA levels correlate with poor outcome on tamoxifen. In concordance, patients with high CCNE protein levels had less benefit from tamoxifen in an adjuvant setting [27], and the overexpression of low molecular weight CCNE isoforms was associated with resistance to fulvestrant [28] and letrozole [29]. CCNE1 is a kinase and regulatory subunit of CDK2 that accumulates at the G1–S phase [30].
The second gene, CDC2 [also known as cyclin-dependent kinase 1 (CDK1)], correlated with miR-26a and EZH2 and treatment outcome. CDC2 is a mitotic cyclin-dependent Ser/Thr protein kinase and the master controller of mammalian cell–cycle regulation which is activated by CDK7 phosphorylation [31, 32]. At present, expression of CDC2 has been linked to response to tamoxifen in cell line models [33], and we now show an 8-month delay in disease progression in patients with the lowest CDC2 mRNA levels compared with those with the highest expression levels. Thus, the status of the cell cycle regulation pathway, specified by CCNE1 and CDC2 levels but also confirmed by CCNB1, CCNE2, and E2F1, seems to play a role in how the metastasis will respond to first-line tamoxifen therapy.
Multivariate analysis of miR-26a, EZH2, CCNE1, and CDC2 to determine their associations with treatment outcome showed that the predictive values of EZH2 and CCNE1 levels were less significant than those of miR-26a and CDC2. Interestingly, not only miR-26a but also CDC2 have a physical interaction with EZH2 (Fig. 3), although with opposite effects on EZH2 functioning. As mentioned, miR-26a binds to the 3′-UTR of EZH2 and inhibits transcription of EZH2. On the other hand, CDC2 (CDK1) and CDK2 have been shown to activate EZH2 by phosphorylation of its Thr350 residue [34–36]. This Thr350 phosphorylation is necessary for EZH2 recruitment at target loci and for maintenance of H2K27me3 levels [34]. Since EZH2 expression and activity are higher in proliferating rather than differentiating cells [22], both miR-26a and CDC2 may define endocrine-responsive or -resistant phenotypes of ER-positive breast cancer cells through their modulation of EZH2 levels and activity. In ER-negative breast cancer cells, EZH2 knockdown results in increased CDC2 and pCDC2 protein expressions [37], but recently it was suggested that EZH2 in ER-negative tumors functions as a transcriptional activator but acts as a repressor in ER-positive tumors [38].
The regulatory network of EZH2. A model for the modulation of the expression and activity of EZH2 based on our results and available data in the literature. Binding of miR-101 and miR-26a to the 3′-UTR blocks transcription of EZH2 [10, 11]. Our data linked expression levels of miR-26a and EZH2 by the GTA of pathways to the cyclins and cell cycle regulation pathway with two significant genes [CCNE1 and CDC2 (CDK1)]. CDC2 (CDK1) and CDK2 activate EZH2 through the phosphorylation of its Thr350 residue [34–36]. Our study shows that, in breast cancer, miR-26a and CDC2 might be involved in the regulation EZH2 expression and activity, respectively, and as a result associate with response to tamoxifen
Therapeutics that can modulate miR-26a, CDC2, or EZH2 activity might be an attractive strategy for patients resistant to tamoxifen to resensitize them for anti-estrogen treatment. Systemic administration of miR-26a with adeno-associated virus in mouse models results in decreased cancer cell proliferation and suppressed tumor progression [23]. Preclinical evaluation of CDC2 and CDK2 inhibitors revealed G2/M arrest and cell death in both anti-estrogen-sensitive and resistant cells [33]. Hydrolase inhibitors, such as DZNep, induce EZH2 depletion in breast cancer cell lines and result in cell cycle arrest and apoptosis [39, 40]. At the end, all these treatments target EZH2 levels and activity. We hypothesize that patients resistant to tamoxifen with low miR-26a and high CDC2 and EZH2 levels in their primary tumor may benefit from these treatment strategies in order to overcome tamoxifen resistance.
In summary, we have shown that high miR-26a and low EZH2 mRNA levels associate with clinical benefit and prolonged TTP. The cell cycle regulation pathway and its genes CCNE1 and CDC2 correlate significantly with miR-26a and EZH2 levels and with outcome on tamoxifen. Multivariate analysis revealed miR-26a and CDC2 as sets of biomarkers to predict outcome on tamoxifen in metastatic breast cancer. Our findings might help one to improve the identification of individual patients resistant to tamoxifen, who may benefit from therapeutics that block EZH2 expression and activity.
References
Jansen MP, Foekens JA, van Staveren IL, Dirkzwager-Kiel MM, Ritstier K, Look MP, Meijer-van Gelder ME, Sieuwerts AM, Portengen H, Dorssers LC et al (2005) Molecular classification of tamoxifen-resistant breast carcinomas by gene expression profiling. J Clin Oncol 23(4):732–740
Kok M, Linn SC, Van Laar RK, Jansen MP, van den Berg TM, Delahaye LJ, Glas AM, Peterse JL, Hauptmann M, Foekens JA et al (2009) Comparison of gene expression profiles predicting progression in breast cancer patients treated with tamoxifen. Breast Cancer Res Treat 113(2):275–283
Schuettengruber B, Chourrout D, Vervoort M, Leblanc B, Cavalli G (2007) Genome regulation by polycomb and trithorax proteins. Cell 128(4):735–745
Reijm EA, Jansen MP, Ruigrok-Ritstier K, van Staveren IL, Look MP, van Gelder ME, Sieuwerts AM, Sleijfer S, Foekens JA, Berns EM (2011) Decreased expression of EZH2 is associated with upregulation of ER and favorable outcome to tamoxifen in advanced breast cancer. Breast Cancer Res Treat 125(2):387–394
Wahid F, Shehzad A, Khan T, Kim YY (2010) MicroRNAs: synthesis, mechanism, function, and recent clinical trials. Biochim Biophys Acta 1803:1231–1241
Foekens JA, Sieuwerts AM, Smid M, Look MP, de Weerd V, Boersma AW, Klijn JG, Wiemer EA, Martens JW (2008) Four miRNAs associated with aggressiveness of lymph node-negative, estrogen receptor-positive human breast cancer. Proc Natl Acad Sci USA 105(35):13021–13026
Verghese ET, Hanby AM, Speirs V, Hughes TA (2008) Small is beautiful: microRNAs and breast cancer-where are we now? J Pathol 215(3):214–221
Miller TE, Ghoshal K, Ramaswamy B, Roy S, Datta J, Shapiro CL, Jacob S, Majumder S (2008) MicroRNA-221/222 confers tamoxifen resistance in breast cancer by targeting p27Kip1. J Biol Chem 283(44):29897–29903
Rodriguez-Gonzalez FG, Sieuwerts AM, Smid M, Look MP, Meijer-van Gelder ME, de Weerd V, Sleijfer S, Martens JW, Foekens JA (2011) MicroRNA-30c expression level is an independent predictor of clinical benefit of endocrine therapy in advanced estrogen receptor positive breast cancer. Breast Cancer Res Treat 127(1):43–51
Varambally S, Cao Q, Mani RS, Shankar S, Wang X, Ateeq B, Laxman B, Cao X, Jing X, Ramnarayanan K et al (2008) Genomic loss of microRNA-101 leads to overexpression of histone methyltransferase EZH2 in cancer. Science 322(5908):1695–1699
Wong CF, Tellam RL (2008) MicroRNA-26a targets the histone methyltransferase Enhancer of Zeste homolog 2 during myogenesis. J Biol Chem 283(15):9836–9843
Hayward JL, Carbone PP, Heuson JC, Kumaoka S, Segaloff A, Rubens RD (1977) Assessment of response to therapy in advanced breast cancer: a project of the Programme on Clinical Oncology of the International Union Against Cancer, Geneva, Switzerland. Cancer 39(3):1289–1294
McShane LM, Altman DG, Sauerbrei W, Taube SE, Gion M, Clark GM (2006) REporting recommendations for tumor MARKer prognostic studies (REMARK). Breast Cancer Res Treat 100(2):229–235
Foekens JA, Portengen H, van Putten WL, Peters HA, Krijnen HL, Alexieva-Figusch J, Klijn JG (1989) Prognostic value of estrogen and progesterone receptors measured by enzyme immunoassays in human breast tumor cytosols. Cancer Res 49(21):5823–5828
Sieuwerts AM, Meijer-van Gelder ME, Timmermans M, Trapman AM, Garcia RR, Arnold M, Goedheer AJ, Portengen H, Klijn JG, Foekens JA (2005) How ADAM-9 and ADAM-11 differentially from estrogen receptor predict response to tamoxifen treatment in patients with recurrent breast cancer: a retrospective study. Clin Cancer Res 11(20):7311–7321
Bachmann IM, Halvorsen OJ, Collett K, Stefansson IM, Straume O, Haukaas SA, Salvesen HB, Otte AP, Akslen LA (2006) EZH2 expression is associated with high proliferation rate and aggressive tumor subgroups in cutaneous melanoma and cancers of the endometrium, prostate, and breast. J Clin Oncol 24(2):268–273
Kleer CG, Cao Q, Varambally S, Shen R, Ota I, Tomlins SA, Ghosh D, Sewalt RG, Otte AP, Hayes DF et al (2003) EZH2 is a marker of aggressive breast cancer and promotes neoplastic transformation of breast epithelial cells. Proc Natl Acad Sci USA 100(20):11606–11611
Cao P, Deng Z, Wan M, Huang W, Cramer SD, Xu J, Lei M, Sui G (2010) MicroRNA-101 negatively regulates Ezh2 and its expression is modulated by androgen receptor and HIF-1alpha/HIF-1beta. Mol Cancer 9:108
Maillot G, Lacroix-Triki M, Pierredon S, Gratadou L, Schmidt S, Benes V, Roche H, Dalenc F, Auboeuf D, Millevoi S et al (2009) Widespread estrogen-dependent repression of microRNAs involved in breast tumor cell growth. Cancer Res 69(21):8332–8340
Sachdeva M, Wu H, Ru P, Hwang L, Trieu V, Mo YY (2011) MicroRNA-101-mediated Akt activation and estrogen-independent growth. Oncogene 30(7):822–831
Czermin B, Melfi R, McCabe D, Seitz V, Imhof A, Pirrotta V (2002) Drosophila enhancer of Zeste/ESC complexes have a histone H3 methyltransferase activity that marks chromosomal polycomb sites. Cell 111(2):185–196
Margueron R, Li G, Sarma K, Blais A, Zavadil J, Woodcock CL, Dynlacht BD, Reinberg D (2008) Ezh1 and Ezh2 maintain repressive chromatin through different mechanisms. Mol Cell 32(4):503–518
Kota J, Chivukula RR, O’Donnell KA, Wentzel EA, Montgomery CL, Hwang HW, Chang TC, Vivekanandan P, Torbenson M, Clark KR et al (2009) Therapeutic microRNA delivery suppresses tumorigenesis in a murine liver cancer model. Cell 137(6):1005–1017
Planas-Silva MD, Weinberg RA (1997) Estrogen-dependent cyclin E-cdk2 activation through p21 redistribution. Mol Cell Biol 17(7):4059–4069
Osborne CK, Boldt DH, Clark GM, Trent JM (1983) Effects of tamoxifen on human breast cancer cell cycle kinetics: accumulation of cells in early G1 phase. Cancer Res 43(8):3583–3585
Sieuwerts AM, Look MP, Meijer-van Gelder ME, Timmermans M, Trapman AM, Garcia RR, Arnold M, Goedheer AJ, de Weerd V, Portengen H et al (2006) Which cyclin E prevails as prognostic marker for breast cancer? Results from a retrospective study involving 635 lymph node-negative breast cancer patients. Clin Cancer Res 12(11 Pt 1):3319–3328
Waltersson MA, Askmalm MS, Nordenskjold B, Fornander T, Skoog L, Stal O (2009) Altered expression of cyclin E and the retinoblastoma protein influences the effect of adjuvant therapy in breast cancer. Int J Oncol 34(2):441–448
Akli S, Zheng PJ, Multani AS, Wingate HF, Pathak S, Zhang N, Tucker SL, Chang S, Keyomarsi K (2004) Tumor-specific low molecular weight forms of cyclin E induce genomic instability and resistance to p21, p27, and antiestrogens in breast cancer. Cancer Res 64(9):3198–3208
Akli S, Bui T, Wingate H, Biernacka A, Moulder S, Tucker SL, Hunt KK, Keyomarsi K (2010) Low-molecular-weight cyclin E can bypass letrozole-induced G1 arrest in human breast cancer cells and tumors. Clin Cancer Res 16(4):1179–1190
Bagheri-Yarmand R, Nanos-Webb A, Biernacka A, Bui T, Keyomarsi K (2010) Cyclin E deregulation impairs mitotic progression through premature activation of Cdc25C. Cancer Res 70(12):5085–5095
Satyanarayana A, Kaldis P (2009) Mammalian cell-cycle regulation: several Cdks, numerous cyclins and diverse compensatory mechanisms. Oncogene 28(33):2925–2939
Malumbres M, Barbacid M (2009) Cell cycle, CDKs and cancer: a changing paradigm. Nat Rev Cancer 9(3):153–166
Johnson N, Bentley J, Wang LZ, Newell DR, Robson CN, Shapiro GI, Curtin NJ (2010) Pre-clinical evaluation of cyclin-dependent kinase 2 and 1 inhibition in anti-estrogen-sensitive and resistant breast cancer cells. Br J Cancer 102(2):342–350
Chen S, Bohrer LR, Rai AN, Pan Y, Gan L, Zhou X, Bagchi A, Simon JA, Huang H (2010) Cyclin-dependent kinases regulate epigenetic gene silencing through phosphorylation of EZH2. Nat Cell Biol 12(11):1108–1114
Wei Y, Chen YH, Li LY, Lang J, Yeh SP, Shi B, Yang CC, Yang JY, Lin CY, Lai CC et al (2011) CDK1-dependent phosphorylation of EZH2 suppresses methylation of H3K27 and promotes osteogenic differentiation of human mesenchymal stem cells. Nat Cell Biol 13(1):87–94
Kaneko S, Li G, Son J, Xu CF, Margueron R, Neubert TA, Reinberg D (2010) Phosphorylation of the PRC2 component Ezh2 is cell cycle-regulated and up-regulates its binding to ncRNA. Genes Dev 24(23):2615–2620
Gonzalez ME, Li X, Toy K, DuPrie M, Ventura AC, Banerjee M, Ljungman M, Merajver SD, Kleer CG (2009) Downregulation of EZH2 decreases growth of estrogen receptor-negative invasive breast carcinoma and requires BRCA1. Oncogene 28(6):843–853
Lee ST, Li Z, Wu Z, Aau M, Guan P, Karuturi RK, Liou YC, Yu Q (2011) Context-specific regulation of NF-kappaB target gene expression by EZH2 in breast cancers. Molecular cell 43(5):798–810
Hayden A, Johnson PW, Packham G, Crabb SJ (2011) S-adenosylhomocysteine hydrolase inhibition by 3-deazaneplanocin A analogues induces anti-cancer effects in breast cancer cell lines and synergy with both histone deacetylase and HER2 inhibition. Breast Cancer Res Treat 127(1):109–119
Tan J, Yang X, Zhuang L, Jiang X, Chen W, Lee PL, Karuturi RK, Tan PB, Liu ET, Yu Q (2007) Pharmacologic disruption of polycomb-repressive complex 2-mediated gene repression selectively induces apoptosis in cancer cells. Genes Dev 21(9):1050–1063
Smid M, Wang Y, Zhang Y, Sieuwerts AM, Yu J, Klijn JG, Foekens JA, Martens JW (2008) Subtypes of breast cancer show preferential site of relapse. Cancer Res 68(9):3108–3114
Acknowledgments
The authors are especially grateful to Renée Foekens, Anne van Galen, Frank Gerritse, Jozien Helleman, Marion Meijer-van Gelder, Wendy Prager-van der Smissen, Marcel Smid, Mieke Timmermans, Anita Trapman, Arzu Umar, and Vanja de Weerd for their contribution and technical support. The authors thank also the surgeons, pathologists, and internists of the St. Clara Hospital, Ikazia Hospital, St. Franciscus Gasthuis at Rotterdam, and Ruwaard van Putten Hospital at Spijkenisse for the supply of tumor tissues and/or their assistance in the collection of clinical follow-up data. This study was in part supported by TI Pharma (T3-108-1, granted to MPHM Jansen and EMJJ Berns) and the Netherlands Genomics Initiative (NGI)/the Netherlands Organization for Scientific Research (NWO) (JWM Martens, S Sleijfer, and JA Foekens).
Funding
This work was supported in part by Top Institute Pharma, Leiden, The Netherlands, Project No. T3-108, and the National Genomics Initiative (NGI) of the Netherlands Organization for Scientific Research (NWO).
Conflict of interest
None of the authors has a conflict of interest.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Additional information
E. A. Reijm and M. P. H. M. Jansen contributed equally.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Jansen, M.P.H.M., Reijm, E.A., Sieuwerts, A.M. et al. High miR-26a and low CDC2 levels associate with decreased EZH2 expression and with favorable outcome on tamoxifen in metastatic breast cancer. Breast Cancer Res Treat 133, 937–947 (2012). https://doi.org/10.1007/s10549-011-1877-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-011-1877-4