Abstract
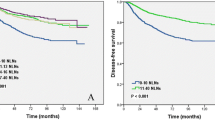
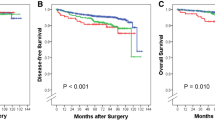
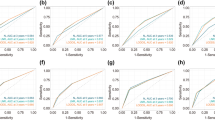
Patients with node-positive breast cancer are currently classified according to pN stage. Lymph node ratio (LNR), the ratio of positive to total removed lymph nodes, maybe a more useful prognostic factor in these patients. We therefore compared LNR and pN staging as prognostic factors in patients with node-positive breast cancer. Using two large prospective databases of the Korean Breast Cancer Registry (KBCR) and the Asan Medical Center (AMC) Breast Cancer Center of patients with LN-positive breast cancer from 1988 to 2005, we compared the ability of LNR and pN stage to predict patient survival by Cox regression analysis in the overall patient cohort and in subgroups categorized by age and intrinsic subtype. Patients were categorized into low- (≤0.20), intermediate- (>0.20 and ≤0.65), and high-risk (>0.65) LNR groups. The difference in mortality risk was greater among LNR groups than among patients staged pN1, pN2, and pN3, as assessed by disease-free survival (DFS), cancer-specific survival (CSS), and overall survival (OS) rates. In contrast to LNR risk categories, the survival curves for pN1 and pN2 stage patients overlapped in those aged <35 years and those with her2/neu-enriched or triple-negative tumors. These findings were validated by analyzing a nationwide registry of 15,488 node-positive patients, which showed that patients with pN1 and intermediate LNR risk had poorer DFS (HR 1.7, 95% CI 1.4–2.2) and CSS (HR 1.6, 95% CI 1.1–2.2) than patients with pN2 and low LNR risk. LNR is a better predictor of prognosis than pN stage in women with breast cancer, especially in high-risk patients, including younger women and women with her2/neu-enriched or triple-negative tumors. Treatment decisions should be based on LNR rather than on pN stage.


Similar content being viewed by others
References
Fisher B, Bauer M, Wickerham DL, Redmond CK, Fisher ER, Cruz AB et al (1983) Relation of number of positive axillary nodes to the prognosis of patients with primary breast cancer. An NSABP update. Cancer 52:1551–1557
Danko ME, Bennett KM, Zhai J, Marks JR, Olson JA (2010) Improved staging in node-positive breast cancer patients using lymph node ratio: results in 1,788 patients with long-term follow-up. J Am Coll Surg 210:797–805
Truong PT, Woodward WA, Thames HD, Ragaz J, Olivotto IA, Buchholz TA (2007) The ratio of positive to excised nodes identifies high-risk subsets and reduces inter-institutional differences in locoregional recurrence risk estimates in breast cancer patients with 1-3 positive nodes: an analysis of prospective data from British Columbia and the M. D. Anderson Cancer Center. Int J Radiat Oncol Biol Phys 68:59–65
Vinh-Hung V, Verkooijen HM, Fioretta G, Neyroud-Caspar I, Rapiti E, Vlastos G et al (2009) Lymph node ratio as an alternative to pN staging in node-positive breast cancer. J Clin Oncol 27:1062–1068
Woodward WA, Vinh-Hung V, Ueno NT, Cheng YC, Royce M, Tai P et al (2006) Prognostic value of nodal ratios in node-positive breast cancer. J Clin Oncol 24:2910–2916
Hatoum HA, Jamali FR, El-Saghir NS, Musallam KM, Seoud M, Dimassi H et al (2009) Ratio between positive lymph nodes and total excised axillary lymph nodes as an independent prognostic factor for overall survival in patients with nonmetastatic lymph node-positive breast cancer. Ann Surg Oncol 16:3388–3395
Greenstein AJ, Litle VR, Swanson SJ, Divino CM, Packer S, Wisnivesky JP (2008) Prognostic significance of the number of lymph node metastases in esophageal cancer. J Am Coll Surg 206:239–246
Chan JK, Kapp DS, Cheung MK, Osann K, Shin JY, Cohn D et al (2007) The impact of the absolute number and ratio of positive lymph nodes on survival of endometrioid uterine cancer patients. Br J Cancer 97:605–611
Hyung WJ, Noh SH, Yoo CH, Huh JH, Shin DW, Lah KH et al (2002) Prognostic significance of metastatic lymph node ratio in T3 gastric cancer. World J Surg 26:323–329
Siewert JR, Bottcher K, Stein HJ, Roder JD (1998) Relevant prognostic factors in gastric cancer: ten-year results of the German gastric cancer study. Ann Surg 228:449–461
Berger AC, Watson JC, Ross EA, Hoffman JP (2004) The metastatic/examined lymph node ratio is an important prognostic factor after pancreaticoduodenectomy for pancreatic adenocarcinoma. Am Surg 70:235–240 (discussion 240)
Herr HW (2003) Superiority of ratio based lymph node staging for bladder cancer. J Urol 169:943–945
Truong PT, Olivotto IA, Kader HA, Panades M, Speers CH, Berthelet E (2005) Selecting breast cancer patients with T1–T2 tumors and one to three positive axillary nodes at high postmastectomy locoregional recurrence risk for adjuvant radiotherapy. Int J Radiat Oncol Biol Phys 61:1337–1347
Ahn SH, Son BH, Kim SW, Kim SI, Jeong J, Ko SS et al (2007) Poor outcome of hormone receptor-positive breast cancer at very young age is due to tamoxifen resistance: nationwide survival data in Korea—a report from the Korean breast cancer society. J Clin Oncol 25:2360–2368
Bland KI, Scott-Conner CE, Menck H, Winchester DP (1999) Axillary dissection in breast-conserving surgery for stage I and II breast cancer: a national cancer data base study of patterns of omission and implications for survival. J Am Coll Surg 188:586–595 (discussion 595–586)
Clarke M, Collins R, Darby S, Davies C, Elphinstone P, Evans E et al (2005) Effects of radiotherapy and of differences in the extent of surgery for early breast cancer on local recurrence and 15-year survival: an overview of the randomised trials. Lancet 366:2087–2106
Ibrahim EM, Elkhodary TR, Zekri JM, Bahadur Y, El-Sayed ME, Al-Gahmi AM et al (2010) Prognostic value of lymph node ratio in poor prognosis node-positive breast cancer patients in Saudi Arabia. Asia Pac J Clin Oncol 6:130–137
Bollet MA, Sigal-Zafrani B, Mazeau V, Savignoni A, de la Rochefordière A, Vincent-Salomon A et al (2007) Age remains the first prognostic factor for loco-regional breast cancer recurrence in young (<40 years) women treated with breast conserving surgery first. Radiother Oncol 82:272–280
Coulombe G, Tyldesley S, Speers C, Paltiel C, Aquino-Parsons C, Bernstein V et al (2007) Is mastectomy superior to breast-conserving treatment for young women? Int J Radiat Oncol Biol Phys 67:1282–1290
Punglia RS, Morrow M, Winer EP, Harris JR (2007) Local therapy and survival in breast cancer. N Engl J Med 356:2399–2405
Voduc KD, Cheang MC, Tyldesley S, Gelmon K, Nielsen TO, Kennecke H (2010) Breast cancer subtypes and the risk of local and regional relapse. J Clin Oncol 28:1684–1691
Millar EKA, Graham PH, O’Toole SA, McNeil CM, Browne L, Morey AL et al (2009) Prediction of local recurrence, distant metastases, and death after breast-conserving therapy in early-stage invasive breast cancer using a five-biomarker panel. J Clin Oncol 27:4701–4708
Nguyen PL, Taghian AG, Katz MS, Niemierko A, Abi Raad RF, Boon WL et al (2008) Breast cancer subtype approximated by estrogen receptor, progesterone receptor, and HER-2 is associated with local and distant recurrence after breast-conserving therapy. J Clin Oncol 26:2373–2378
Gervasoni JE, Taneja C, Chung MA, Cady B (2000) Biologic and clinical significance of lymphadenectomy. Surg Clin North Am 80:1631–1673
Greco M, Gennaro M, Valagussa P, Agresti R, Ferraris C, Ferrari B et al (2000) Impact of nodal status on indication for adjuvant treatment in clinically node negative breast cancer. Istituto Nazionale per lo Studio e las Cura dei Tumori. Ann Oncol 11:1137–1140
Cady B (2000) A contemporary view of axillary dissection. Ann Surg 232:8–9
Overgaard M, Nielsen HM, Overgaard J (2007) Is the benefit of postmastectomy irradiation limited to patients with four or more positive nodes, as recommended in international consensus reports? A subgroup analysis of the DBCG 82 b&c randomized trials. Radiother Oncol 82:247–253
Cheng JC, Chen CM, Liu MC, Tsou MH, Yang PS, Jian JJ et al (2002) Locoregional failure of postmastectomy patients with 1–3 positive axillary lymph nodes without adjuvant radiotherapy. Int J Radiat Oncol Biol Phys 52:980–988
Yang PS, Chen CM, Liu MC, Jian JM, Horng CF, Liu MJ et al (2010) Radiotherapy can decrease locoregional recurrence and increase survival in mastectomy patients with T1 to T2 breast cancer and one to three positive nodes with negative estrogen receptor and positive lymphovascular invasion status. Int J Radiat Oncol Biol Phys 77:516–522
Chen JJ, Wu J (2010) Management strategy of early-stage breast cancer patients with a positive sentinel lymph node: With or without axillary lymph node dissection. Crit Rev Oncol Hematol 79(3):293–301
Moghaddam Y, Falzon M, Fulford L, Williams NR, Keshtgar MR (2010) Comparison of three mathematical models for predicting the risk of additional axillary nodal metastases after positive sentinel lymph node biopsy in early breast cancer. Br J Surg. doi:10.1002/bjs.7181
van den Hoven I, Kuijt GP, Voogd AC, van Beek MW, Roumen RM (2010) Value of memorial Sloan-Kettering cancer center nomogram in clinical decision making for sentinel lymph node-positive breast cancer. Br J Surg. doi:10.1002/bjs.7186
Jakub JW, Bryant K, Huebner M, Hoskin T, Boughey JC, Reynolds C et al. (2010) The number of axillary lymph nodes involved with metastatic breast cancer does not affect outcome as long as all disease is confined to the sentinel lymph nodes. Ann Surg Oncol. doi:10.1245/s10434-010-1202-1
Barranger E, Coutant C, Flahault A, Delpech Y, Darai E, Uzan S (2005) An axilla scoring system to predict non-sentinel lymph node status in breast cancer patients with sentinel lymph node involvement. Breast Cancer Res Treat 91:113–119
Punglia RS, Morrow M, Winer EP, Harris JR (2007) Local therapy and survival in breast cancer. N Engl J Med 356:2399–2405
Conflict of interest
The authors declare no conflict of interest. The authors confirm that there is no financial arrangement with anyone.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ahn, S.H., Kim, H.J., Lee, J.W. et al. Lymph node ratio and pN staging in patients with node-positive breast cancer: a report from the Korean breast cancer society. Breast Cancer Res Treat 130, 507–515 (2011). https://doi.org/10.1007/s10549-011-1730-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-011-1730-9