Abstract
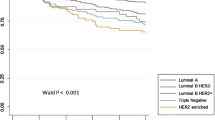
The objective of this study is to define the survival outcomes associated with distinct molecular phenotypes defined by immunohistochemical staining of paraffin-embedded tissues among invasive breast cancer cases identified from the Nurses’ Health Study (NHS). Tissue microarrays were constructed from archived tissue blocks of women diagnosed with breast cancer in the NHS (1976–1997). Invasive non-metastatic breast cancer tumors (n = 1,945) were classified into 1 of 5 molecular phenotypes based on immunohistochemistry assays for estrogen receptor (ER), progesterone receptor (PR), HER2, cytokeratin (CK) 5/6, epidermal growth factor receptor (EGFR) and grade. Survival outcomes were estimated using the Kaplan–Meier product limit method. Cox-proportional hazards models were fitted to determine the association of molecular phenotype with survival outcomes after adjusting for covariates. 1,279 (65.8%) tumors were classified as luminal A, 279 (14.3%) as luminal B, 95 (4.9%) as HER2 type, 203 (10.4%) as basal-like and 89 (4.6%) tumors were unclassified. The 5-year breast cancer-specific survival estimates for women with luminal A, luminal B, HER2-type, basal-like and unclassified tumors were 96, 88, 81, 89 and 85%, respectively. In the multivariable model, compared to cases with luminal A tumors, cases with luminal B (HR 1.90, 95% CI 1.33–2.71), HER2-type (HR 1.36, 95% CI 0.87–2.12), basal-like (HR 1.58, 95% CI 1.05–2.39) and unclassified (HR 1.38, 95% CI 0.87–2.20) tumors had higher hazard of breast cancer death. Similar trends were observed for both overall and recurrence-free survival. In conclusion, compared to women who have luminal A tumors those with luminal B, HER2-type, basal-like and unclassified tumors had a worse prognosis, when tumor subtype was defined by immunohistochemistry. This method may provide a cost-effective means of determining prognosis in the clinical setting.

Similar content being viewed by others
Abbreviations
- ER:
-
Estrogen receptor
- PR:
-
Progesterone receptor
- HER2:
-
Human epidermal growth factor receptor 2
- CK5/6:
-
Cytokeratin 5/6
- EGFR:
-
Epidermal growth factor receptor
- NHS:
-
Nurses’ Health Study
- TMA:
-
Tissue microarray
- OS:
-
Overall survival
- BCS:
-
Breast cancer specific survival
- RFS:
-
Recurrence-free survival
- BMI:
-
Body mass index
- HR:
-
Hazard ratio
- 95% CI:
-
95 percent confidence interval
References
Sorlie T, Perou CM, Tibshirani R et al (2001) Gene expression patterns of breast carcinomas distinguish tumor subclasses with clinical implications. Proc Natl Acad Sci USA 98:10869–10874
Sorlie T, Tibshirani R, Parker J et al (2001) Repeated observation of breast tumor subtypes in independent gene expression data sets. Proc Natl Acad Sci USA 100:8418–8423
Van’t Veer LJ, Dai H, van de Vijver MJ et al (2002) Gene expression profiling predicts clinical outcome of breast cancer. Nature (Lond.) 415:530–536
Sotiriou C, Neo SY, McShane LM et al (2003) Breast cancer classification and prognosis based on gene expression profiles from a population based study. Proc Natl Acad Sci USA 100:10393–10398
Hu Z, Fan C, Oh DS et al (2006) The molecular portraits of breast tumors are conserved across microarray platforms. BMC Genomics 7:96
Sorlie T, Wang Y, Xiao C et al (2006) Distinct molecular mechanisms underlying clinically relevant subtypes of breast cancer: gene expression analysises across three different platforms. BMC Genomics 7:127
Fan C, Oh DS, Wessels L et al (2006) Concordance among gene-expression-based predictors for breast cancer. N Engl J Med 355:560–569
Nielson TO, Hsu FD, Jensen K et al (2004) Immunohistochemical and clinical characterization of the basal-like subtype of invasive breast cancer. Clin Cancer Res 10:5367–5374
Abd El-Rehim DM, Ball G, Pinder SE et al (2005) High-throughput protein expression analysis using tissue microarray technology of a large well-characterized series identifies biologically distinct classes of breast cancer confirming recent cDNA expression analyses. Int J Cancer 116:340–350
Abd El-Rehim DM, Pinder SE, Paish CE et al (2004) Expression of luminal and basal cytokeratins in human breast carcinoma. J Pathol 203:661–671
van de Rijn M, Perou CM, Tibshirani R et al (2002) Expression of cytokeratins17 and 5 identifies a group of breast carcinomas with poor clinical outcome. Am J Pathol 161:1991–1996
Cheang MCU, Voduc D, Bajdik C et al (2008) Basal-like breast defined by five biomarkers has superior prognostic value than triple-negative phenotype. Clin Cancer Res 14:1368–1376
Carey LA, Dees EC, Sawyer L, Gatti L, Moore DT, Collichio F, Ollila DW, Sartor CI, Graham ML, Perou CM (2007) The triple negative paradox: primary tumor chemosensitivity of breast cancer subtypes. Clin Cancer Res 13:2329–2334
Carey LA, Perou CM, Livasy CA, Dressler LG, Cowan D, Conway K, Karaca G, Troester MA, Tse CK, Edmiston S, Deming SL, Geradts J, Cheang MC, Nielsen TO, Moorman PG, Earp HS, Millikan RC (2006) Race, breast cancer subtypes, and survival in the Carolina Breast Cancer Study. JAMA 295:2492–2502
Tamimi RM, Baer HJ, Marotti J, Galan M, Galaburda L, Fu Y et al (2008) Comparison of molecular phenotypes of ductal carcinoma in situ and invasive breast cancer. Breast Cancer Res 100:218–221
Sathiakumar N, Delzell E, Abdalla O (1998) Using the National Death Index to obtain underlying cause of death codes. J Occup Environ Med 40:808–813
Rutqvist LE (1985) Validity of certified causes of death in breast carcinoma patients. Acta Radiol Oncol 24:385–390
Stampfer MJ, Willett WC, Speizer FE et al (1984) Test of the National Death Index. Am J Epidemiol 119:837–839
Harris J, Lippman M, Morrow M, Osborne C (2004) Diseases of the breast, 3rd edn. Lippincott, Philadelphia
Slamon DJ, Leyland-Jones B, Shak S et al (2001) Use of chemotherapy plus a monoclonal antibody against HER2 for metastatic breast cancer that overexpresses HER2. N Engl J Med 344:783–792
Romond EH, Perez EA, Bryant J et al (2005) Trastuzumab plus adjuvant chemotherapy for operable HER2-positive breast cancer. N Engl J Med 353:1673–1684
Piccart-Gebhart MJ, Procter M, Leyland-Jones B et al (2005) Trastuzumab after adjuvant chemotherapy in HER2-positive breast cancer. N Engl J Med 353:1659–1672
Joensuu H, Kellokumpu-Lehtinen PL, Bono P et al (2006) Adjuvant docetaxel or vinorelbine with or without trastuzumab for breast cancer. N Engl J Med 354:809–820
Dawood S, Kristine B, Hortobagyi GN, Giordano SH (2008) Prognosis of women with stage IV breast cancer by HER2 status and trastuzumab treatment: An institutional based review. J Clin Oncol 26(suppl):1018
Early Breast Cancer Trialists’ Collaborative Group (2005) Effects of chemotherapy and hormonal therapy for early breast cancer on recurrence and 15-year survival: an overview of the randomized trials. Lancet 365:1687–1717
Acknowledgments
We thank Dr. Yineng Fu for central pathology review of all the breast cancer cases included in this study. We are grateful to the participants of the Nurses’ Health Study for their outstanding dedication and commitment to the study. This study was supported by GlaxoSmithKline (WE234 (EPI40307)), Public Health Service Grants CA087969, and SPORE in Breast Cancer CA089393, from the National Cancer Institute, National Institutes of Health, Department of Health and Human Services and Breast Cancer Research Fund. Dr. Graham Colditz was supported in part by an American Cancer Society Cissy Hornung Clinical Research Professorship.
Conflict of interest
The authors declare that they have no competing interests.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Dawood, S., Hu, R., Homes, M.D. et al. Defining breast cancer prognosis based on molecular phenotypes: results from a large cohort study. Breast Cancer Res Treat 126, 185–192 (2011). https://doi.org/10.1007/s10549-010-1113-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-010-1113-7