Summary
Introduction
Patients’ perceptions of having had freedom of choice in treatment decision-making are shown to have implications for their quality of life. It is, therefore, important to determine what factors underlie these perceptions. One factor that has been studied is whether or not patients believed that their doctor had offered choice of treatment. However, even when choice is actually offered, patients may still feel that they have no choice. Little attention has been paid to other factors that may contribute to patients’ perceptions of having had no choice. Our purpose was to explore (1) whether early-stage breast cancer patients perceived to have had a choice with regard to adjuvant chemotherapy, and (2) their reasons for having perceived no choice.
Patients and methods
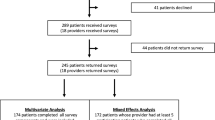
The determinants of no choice that we examined were: (1) (preferred) involvement in treatment decision-making, (2) perceived clinical benefits of chemotherapy (e.g., cure), (3) perceived psychological benefits (e.g., less worries), and (4) perception of being able to cope with the side effects. All predictors, as well as patient and clinical characteristics, were entered simultaneously in a multiple logistic regression analysis and non-significant predictors were removed step-by-step, until only significant predictors (p<0.05) remained. Because determinants may differ between patients with experience of chemotherapy and those without, both treatment groups were analyzed separately.
Results
Four hundred and forty-six patients filled out the questionnaire (62%). Sixty-six percent of patients who had been treated with chemotherapy and 86% of inexperienced patients had perceived no treatment choice. In both treatment groups, patients who preferred a shared role or a passive role in treatment decision-making were statistically significantly more likely to have perceived no treatment choice than patients who preferred an active role. Surprisingly, beliefs about the clinical and psychological benefits of chemotherapy did not influence patients’ perceptions of having had choice of treatment.
Conclusion
If we adhere to patient autonomy and shared decision making, we may consider the perception of no treatment choice as a negative outcome of treatment decision-making. However, if this is the result of the patients’ preference for less active involvement in treatment decision-making, the topic of perception of no treatment choice may be viewed in a different light.
Similar content being viewed by others
References
Deadman JM, Leinster SJ, Owens RG, Dewey ME, Slade PD, Taking responsibility for cancer treatment Soc Sci Med 53: 669–677, 2001
Hack TF, Degner LF, Dyck DG, Relationship between preferences for decisional control and illness information among women with breast cancer: a quantitative and qualitative analysis Soc Sci Med 39: 279–289, 1994
Morris J, Royle GT, Offering patients a choice of surgery for early breast cancer: a reduction in anxiety and depression in patients and their husbands Soc Sci Med 26: 583–585, 1988
Street RL, Voigt B, Patient participation in deciding breast cancer treatment and subsequent quality of life Med Decis Making 17: 298–306, 1997
Mandelblatt JS, Edge SB, Meropol NJ, et al. Predictors of long-term outcomes in older breast cancer survivors: perceptions versus patterns of care J Clin Oncol 21: 855–863, 2003
Polsky D, Keating NL, Weeks JC, Schulman KA, Patient choice of breast cancer treatment: impact on health state preferences Med Care 40: 1068–1079, 2002
Al-Ghazal SK, Fallowfield L, Blamey RW, Comparison of psychological aspects and patient satisfaction following breast conserving surgery, simple mastectomy and breast reconstruction Eur J Cancer 36: 1938–1943, 2000
King MT, Kenny P, Shiell A, Hall J, Boyages J, Quality of life three months and one year after first treatment for early stage breast cancer: influence of treatment and patient characteristics Qual Life Res 9: 789–800, 2000
Krupat E, Fancey M, Cleary PD, Information and its impact on satisfaction among surgical patients Soc Sci Med 51: 1817–1825, 2000
Charles C, Redko C, Whelan T, Gafni A, Reyno L, Doing nothing is no choice: lay constructions of treatment decision-making among women with early-stage breast cancer Soc Health Illness 20: 71–95, 1998
Henman MJ, Butow PN, Brouwn RF, Boyle F, Tattersall MHN, Lay constructions of decision-making in cancer Psycho-Oncol 11: 295–306, 2002
Jansen SJT, Otten W, Baas-Thijssen MCM, Stiggelbout AM, Improved communication can help patients make better decisions with regard to adjuvant chemotherapy Psycho-oncol 12: 830–830, 2003
Sutherland HJ, Llewellyn-Thomas HA, Lockwood GA, Tritchler DL, Till JE, Cancer patients: their desire for information and participation in treatment decisions J R Soc Med 82: 260–263, 1989
Degner LF, Kristjanson LJ, Bowman D, et al. Information needs and decisional preferences in women with breast cancer JAMA 277: 1485–1492, 1997
Siegel S, Castellan Jr NJ, 1988 Nonparametric Statistics for the Behavioral Sciences. McGraw-Hill Book Company, New York
Fallowfield L, Offering choice of surgical treatment to women with breast cancer Patient Educ Couns 30: 209–214, 1997
Richards MA, Ramirez AJ, Degner LF, Fallowfield LJ, Maher EJ, Neuberger J, Offering choice of treatment to patients with cancers. A review based on a symposium held at the 10th annual conference of The British Psychosocial Oncology Group, December 1993 Eur J Cancer 31A: 112–116, 1995
Arora NK, McHorney CA, Patient preferences for medical decision making: who really wants to participate? Med Care 38: 335–341, 2000
Beaver K, Luker KA, Owens RG, Leinster SJ, Degner LF, Sloan JA, Treatment decision making in women newly diagnosed with breast cancer Cancer Nurs 19: 8–19, 1996
Bilodeau BA, Degner LF, Information needs, sources of information, and decisional roles in women with breast cancer Oncol Nurs Forum 23: 691–696, 1996
Davison BJ, Degner LF, Morgan TR, Information and decision-making preferences of men with prostate cancer Oncol Nurs Forum 22: 1401–1408, 1995
Gattellari M, Butow PN, Tattersall MH, Sharing decisions in cancer care Soc Sci Med 52: 1865–1878, 2001
Maly RC, Umezawa Y, Leake B, Silliman RA, Determinants of participation in treatment decision-making by older breast cancer patients Breast Cancer Res Tr 85: 201–209, 2004
Blanchard CG, Labrecque MS, Ruckdeschel JC, Blanchard EB, Information and decision-making preferences of hospitalized adult cancer patients Soc Sci Med 27: 1139–1145, 1988
Cassileth BR, Zupkis RV, Sutton-Smith K, March V, Information and participation preferences among cancer patients Ann Intern Med 92: 832–836, 1980
Degner LF, Sloan JA, Decision making during serious illness: what role do patients really want to play? J Clin Epidemiol 45: 941–950, 1992
Jansen SJT, Otten W, Baas-Thijssen MCM, van de Velde CJH, Nortier JWR, Stiggelbout AM, Explaining differences in attitude towards adjuvant chemotherapy between experienced and inexperienced breast cancer patients J Clin Oncol 23: 6623–6630, 2005
Acknowledgement
This study was supported by a grant from the Dutch Cancer Society (UL 2000-2334).
Author information
Authors and Affiliations
Corresponding author
Appendix A
Appendix A
(Preferred) Involvement in treatment decision-making: |
(1) I have left the choice of whether I have adjuvant chemotherapy or not to my doctor. |
(2) I can judge for myself whether adjuvant chemotherapy is necessary. |
(3) People differ in the degree to which they want to take part in treatment decision-making about adjuvant chemotherapy. Some patients prefer to leave decisions about chemotherapy up to their doctor, while others prefer to participate in these decisions. Please check the statement that best describes what you prefer:a |
I prefer that the doctor makes the decision about treatment with adjuvant chemotherapy. |
I prefer that the doctor makes the decision about treatment with adjuvant chemotherapy, but strongly considers my opinion. |
I prefer that the doctor and I make the decision about treatment with adjuvant chemotherapy together on an equal basis. |
I prefer that I make the decision about treatment with adjuvant chemotherapy, but strongly consider the doctor’s opinion. |
I prefer that I make the decision about treatment with adjuvant chemotherapy. |
Perceived clinical benefits: |
If I am treated with adjuvant chemotherapy, then ... |
(4) My life will be prolonged. |
(5) The risk of the disease coming back will be less. |
(6) My chance of being cured will be greater. |
Perceived psychological benefits |
If I am treated with adjuvant chemotherapy, then ... |
(7) I believe that I will have done everything I can to be cured. |
(8) I will think that I am actively contributing something towards my cure. |
(9) I will be less worried about the disease recurring. |
Being able to cope with the side-effects of treatment |
Do you think that you could cope with the side-effects of adjuvant chemotherapy if they consisted of: |
(10) Mild nausea, mild fatigue, and mild hair loss? |
(11) Severe nausea, severe fatigue, and severe hair loss? |
Rights and permissions
About this article
Cite this article
Jansen, S.J., Otten, W. & Stiggelbout, A.M. Factors affecting patients’ perceptions of choice regarding adjuvant chemotherapy for breast cancer. Breast Cancer Res Treat 99, 35–45 (2006). https://doi.org/10.1007/s10549-006-9178-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-006-9178-z