Abstract
Leigh syndrome (LS) is a progressive neurodegenerative disorder of infancy and early childhood. It is clinically diagnosed by typical manifestations and characteristic computed tomography (CT) or magnetic resonance imaging (MRI) studies. Unravelling mitochondrial respiratory chain (MRC) dysfunction behind LS is essential for deeper understanding of the disease, which may lead to the development of new therapies and cure. The aim of this study was to evaluate the clinical validity of various diagnostic tools in confirming MRC disorder in LS and Leigh-like syndrome (LL). The results of enzyme assays, molecular analysis, and cellular oxygen consumption rate (OCR) measurements were examined. Of 106 patients, 41 were biochemically and genetically verified, and 34 had reduced MRC activity but no causative mutations. Seven patients with normal MRC complex activities had mutations in the MT-ATP6 gene. Five further patients with normal activity in MRC were identified with causative mutations. Conversely, 12 out of 60 enzyme assays performed for genetically verified patients returned normal results. No biochemical or genetic background was confirmed for 19 patients. OCR was reduced in ten out of 19 patients with negative enzyme assay results. Inconsistent enzyme assay results between fibroblast and skeletal muscle biopsy samples were observed in 33% of 37 simultaneously analyzed cases. These data suggest that highest diagnostic rate is reached using a combined enzymatic and genetic approach, analyzing more than one type of biological materials where suitable. Microscale oxygraphy detected MRC impairment in 50% cases with no defect in MRC complex activities.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Leigh syndrome (LS) (OMIM 256000), also known as subacute necrotizing encephalopathy, is a progressive neurodegenerative disorder associated with primary or secondary dysfunction of mitochondrial oxidative phosphorylation. Clinical manifestations include psychomotor regression or retardation and signs of brainstem dysfunction, such as respiratory disturbance, nystagmus, ophthalmoplegia, or dysphagia (Thorburn and Rahman 1993). Symptoms often start in infancy, and many patients do not survive into childhood (Sofou et al. 2014). LS was originally defined neuropathologically by bilateral necrotic lesions in the basal ganglia and/or brainstem that were found at autopsy (Leigh 1951). Such lesions can now be observed in vivo with brain magnetic resonance imaging (MRI) or computed tomography (CT) (Gropman 2013). LS is clinically diagnosed based on typical manifestations and neuroimaging, accompanied by an elevated lactate or lactate-to-pyruvate (L/P) ratio in the blood or cerebrospinal fluid (CSF). The clinical diagnosis is followed by enzyme assays and genetic analysis to confirm the biochemical and molecular background (Baertling et al. 2014).
With advances in biochemical techniques and genomic medicine, enzyme assays and genetic analyses are now standard procedures for confirming mitochondrial respiratory chain (MRC) disorders. Numerous reports on the biochemical and molecular profiles of LS have been published, but there are limited studies on clinically diagnosed LS with negative biochemical or molecular findings (Sofou et al. 2014), and the clinical validity of these diagnostic methods remains unknown. In this report, we present the results of 106 Japanese patients with LS and Leigh-like syndrome (LL) to evaluate the clinical validity of various diagnostic methods. We also assessed the detection rate of each type of biological material for the enzyme assays to determine which was optimal for diagnosing LS/LL patients. We also assessed the usefulness of microscale oxygraphy.
Patients and methods
Patients
A total of 106 patients were included in this study. Patients were referred to either Chiba Children’s Hospital or Saitama Medical University for enzyme assay and genetic analysis of MRC disorders from February 2007 to February 2015 by pediatricians and neurologists across Japan. Written informed consent was obtained from the parents of each patient. Both institutions received approval for comprehensive MRC analysis and genetic analysis from their appropriate ethics review boards. Data on the present illness, laboratory results, and neuroimaging findings were extracted from case summaries that accompanied the samples.
We used the stringent criteria defined by Rahman as the inclusion criteria for LS (Rahman et al. 1996). Those with atypical or normal neuroimaging results, or those with typical neuroimaging but with normal lactate levels in serum and CSF were classified as LL patients (Rahman et al. 1996). Patients were excluded from the study when they were diagnosed with pyruvate dehydrogenase complex deficiency or eventually diagnosed as having other metabolic diseases.
Measurements
Activities of MRC complexes I, II, III, and IV were assayed in mitochondria isolated from skin fibroblasts or in the crude supernatant following centrifugation at 600 g from tissues, as previously described (Kirby et al. 1999; Murayama et al. 2009). Enzyme activities of each complex were presented as the percentage of normal control mean relative to appropriate reference enzyme activities, such as citrate synthase or MRC complex II. Enzyme activity was defined as being decreased at <40% in a cell line or <30% in a tissue, as reported (Bernier et al. 2002).
The cellular oxygen consumption rate (OCR) of fibroblast-derived cell lines was measured using microscale oxygraphy (Seahorse XF96 system; Seahorse Bioscience, Billerica, MA, USA) in cases with negative enzyme assay results. Material was prepared as reported (Kopajtich et al. 2014). After measurement of the basal OCR, oligomycin, carbonyl cyanide phenylhydrazone, and rotenone were added sequentially, and OCR was recorded after each addition. Maximum respiration rate (MRR) corresponds to the OCR after the addition of carbonyl cyanide phenylhydrazone minus rotenone-insensitive OCR (Invernizzi et al. 2012). Samples were measured in a 96-well plate, using 16 wells for each sample. Each sample’s data were normalized as 20,000 cells per well. We analyzed five control samples, each one being measured at least five times. Cells in passages five through nine were used for controls and patient samples. In each run, we measured one or two controls with patient samples. OCR was expressed as percentage relative to the average of control(s).
Patients with MRC defects by enzyme assay were analyzed for mitochondrial DNA (mtDNA) mutations by whole mtDNA sequencing. Where no causative mtDNA mutations were found, we proceeded to whole-exome sequencing with next-generation sequencing for nuclear DNA (nDNA) mutations. Detailed information on this procedure was previously reported (Kohda et al. 2016). Those with negative enzyme assay results were screened for mutations using targeted gene panel of 251 nuclear genes known to cause mitochondrial diseases as well as the whole mitochondrial genome. In a few cases where referring clinicians had screened for and identified common mtDNA mutations before referring patients to our institutions, findings were negative in our enzyme assay. There was also one case in whom an outside laboratory identified an nDNA mutation, although it was biochemically negative in our assay. The results of these cases were incorporated into the study to estimate the detection rate of each diagnostic method.
Statistical analysis
Statistical analysis was performed using Microsoft Excel 2010 (Microsoft, Redmond, WA, USA). The Kruskal–Wallis H test was used to evaluate differences in continuous variables between groups, chi-squared and Fisher’s tests were used to evaluate differences between categorical variables, and Wilcoxon test was used to evaluate differences between control and patient samples. All statistical tests were two sided, and p values <0.05 were considered statistically significant.
Results
Overview
All 106 analyzed patients were from different families, and no consanguinity was reported. Seventy-five patients showed MRC defects that satisfied Bernier’s criteria (Table 1). Forty-one of those patients received a molecular diagnosis: nDNA mutations in 19 and mtDNA mutations in 22. In 34 patients, the underlying genetic mutation was not identified. Of the 31 patients with no apparent reduction in MRC activities, seven had mutations in MT-ATP6, one in MT-ND6, three in ECHS1, and one in SLC19A3. The remaining 19 patients had no biochemical defect in MRC and no confirmed genetic diagnosis, including two patients whose gene analysis was not performed due to lack of material. Microscale oxygraphy was performed in 19 available fibroblast cell lines, with no reduction in enzyme activities and a significant reduction in OCR observed in ten.
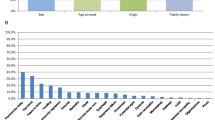
Clinical presentation
Patient clinical features and metabolic status are summarized in Table 2 according to their biochemical and genetic backgrounds:
-
1.
Positive assay and mutation identified (41 patients)
-
2.
Mutation only (12 patients)
-
3.
Positive assay only (34 patients)
-
4.
Negative assay and no confirmed genetic diagnosis (19 patients).
There was no apparent clinical difference between groups. Patient status, age of living patients, LS/LL ratio, and median age at onset were similar. Besides regression and developmental delay, seizure and respiratory distress were the two major clinical symptoms observed in each group. There were no differences in serum or CSF lactate levels between groups. The mean serum and CSF L/P ratios for the whole cohort were 23.0 ± 13.2 and 24.1 ± 18.9, respectively, which were higher than the L/P ratios in normal individuals (Saudubray and Charpentier 2001), with no significant difference between groups.
Enzyme assay
A total of 154 samples (92 fibroblast, 56 skeletal muscle, four liver, one cardiac muscle, and one lymph node) were submitted for enzyme assay, and a total of 151 assays (91 fibroblasts, 55 skeletal muscle, four liver, and one cardiac muscle sample) were completed. Of these, 89 assays (59%) exhibited decreased activity: fibroblasts, 54/91 (59%); skeletal muscle, 31/55 (56%); liver, 4/4 (100%); and cardiac muscle, 0/1 (0%), confirming MRC disorder in 75 (71%) of the 106 patients analyzed. No significant difference was found between the detection rate of fibroblasts and skeletal muscle biopsy samples. Isolated complex I defect was most frequently observed (37 patients), followed by isolated complex IV (17). Combined complex defects were observed in 20 patients, and the most frequently observed combination was defects of complexes I and IV (13).
In 42 patients, more than one type of tissue material was assayed; results were inconsistent in 17. Excluding those with mutations in the MT-ATP6 gene, 37 patients had both skeletal muscle biopsy samples and fibroblasts assayed; results were inconsistent in 13 (Supplementary Table 1). Inconsistency was observed in four patients with nDNA mutations, in one with mtDNA mutation, and in eight with no genetic background confirmed. For genetically verified patients excluding those with mutations in the MT-ATP6 gene, 60 samples were analyzed by enzyme assay; 12 returned normal or nonsignificant results, the majority of which were from patients with nDNA mutations (Supplementary Table 2).
Oxygen consumption rate
The OCR was measured in 19 of the 31 LS/LL patients who presented normal enzyme assay results. Seven cases with mtDNA mutations were omitted. Analysis was precluded in three cases from whom fibroblast cell lines were not available. In an additional two patients, cell lines did not react properly to the experiment, and results were not obtained. Based on MRR distribution in our five controls, a reduction to <71.6% was considered a significant decline (p < 0.05). In 19 patients, it ranged from 36% to 136%, with a median of 69% of normal control(s). Ten patients showed a significant decline, suggesting mitochondrial respiratory dysfunction (Table 3).
mtDNA analysis
Analysis of mtDNA mutation was performed for 103 patients and were identified in 30 patients across seven different genes (Table 4), resulting in a yield of 29%. MT-ATP6 was the gene most frequent (ten patients). We also identified 19 patients with 11 different mutations in mtDNA genes related to complex I.
Previously unreported variants were considered as potential novel causative mutations of LS/LL when they coincided with positive enzyme assay results. Mutation m.14439G>A was shown to be pathogenic using cybrid analysis (Uehara et al. 2014). One of two cases with a mutation in m.14487T>C showed a reduction in enzyme activity of complex I. Mutations m.3946G>A and m.14687A>G had been reported to cause other mitochondrial diseases (Kirby et al. 2004; Spruijt et al. 2007; Bruno et al. 2003) and were considered as causative in our patients who showed defects in respective MRC complexes. Enzyme analysis of patients with confirmed pathogenic mutations m.3697G>A, m.10158T>C, m.10191T>C, m.13513G>A, and m.14459G>A all showed defects in complex I (Kohda et al. 2016).
nDNA analysis
Seventy-six patients proceeded to nDNA analysis, and 17 patients were identified with mutations in nine genes related to MRC complexes (SURF1, NDUFA1, NDUFAF6, NDUFS4, NDUFS6, NDUFV2, BOLA3, SCO2, and GTPBP3, see Table 4). Mutations in NDUFAF6 and SURF1 were most frequent (five patients each), with all patients showing reduced activity in complex I (NDUFAF6) or IV (SURF1). Mutations in genes related to complex I constituted more than half of the nDNA mutations. The genetic defects were all in agreement with the biochemical defects.
Four cases were identified with a mutation in ECHS1, a gene involved in valine degradation. An outside laboratory identified one more patient with a mutation in the same gene (Yamada et al. 2015). Accumulation of toxic intermediates caused by impairment in this pathway is suspected to cause MRC complex defect (Peters et al. 2014). Three of our five patients showed no decline in enzyme activities, one patient showed a defect in complex IV and another in complex I. Lastly, one patient was identified with a mutation in SLC19A3, a gene encoding a thiamine transporter, which is essential for cerebral thiamine metabolism.
Mutations in all these genes except BOLA3 had been reported to cause LS (Tiranti et al. 1998; Budde et al. 2000; Fernandez-Moreira et al. 2007; McKenzie et al. 2011; Kopajtich et al. 2014; Peters et al. 2014; Gerards et al. 2013). BOLA3 had been identified in patients with other mitochondrial diseases (Cameron et al. 2011; Haack et al. 2013), and our case was previously reported as the first evidence of this mutation in an LS patient (Kohda et al. 2016).
Discussion
We demonstrated the importance of combining multiple methods of diagnosing LS/LL patients. Genetic analysis identified a causative mutation in 51% (53/104) of analyzed cases. Enzyme assay recognized MRC complex defects in 71% (75/106) of patients. With those approaches combined, MRC defects were confirmed in 82% (87/106) of cases. The highest diagnostic rate was reached by a combined enzymatic and genetic approach. Seven patients with normal enzyme activities had mutations in the MT-ATP6 gene, which encodes for complex V, which is measured in few laboratories. Screening for MT-ATP6 mutations should be performed in such settings at an early stage of diagnosis, as they comprise a significant proportion of LS/LL etiology, and screening is readily available.
Detection rates in our study of various biopsy samples were <60% individually, which confirms previous results. Most importantly, the rate in muscle biopsies was no higher than in fibroblast cell lines, a finding not reported previously. For the diagnosis of mitochondrial diseases, skeletal muscle is often considered the tissue of choice (Thorburn and Rahman 1993), and fibroblasts have been considered less sensitive than skeletal muscle biopsy samples, detecting MRC defects in only half of cases with positive skeletal muscle assay results (Thorburn et al. 2004; Heuvel et al. 2004). A similar sensitivity was observed in our study, although skeletal muscle biopsy samples returned negative results in six out of 19 cases with reduced MRC activity in fibroblasts, resulting in similar overall detection rates. Tissue specificity of mitochondrial diseases was attributed to heteroplasmy of mtDNA, but inconsistencies between materials were frequently observed in nDNA-mutated cases. These findings suggest that, when possible, more than one type of patient biological sample should be analyzed, regardless of genetic background, to improve the detection rate of mitochondrial disorder.
In pediatric practice, it can be difficult to obtain multiple biological samples, and physicians must choose selectively. Although tissues used for analysis should be taken from the most affected organ (Munnich and Rustin 2001), this is difficult to apply in principle to LS/LL, a neurodegenerative disorder of the central nervous system. So the choice would be between skeletal muscle biopsy samples and cultured fibroblast cell lines in most cases. Skeletal muscle biopsy is invasive and requires general anesthesia, which poses a risk to pediatric patients (Baertling et al. 2014). Fibroblasts, on the other hand can be obtained in office settings with local anesthesia. If only one type of material can be obtained, fibroblasts should be prioritized, as cell lines from cultured fibroblasts can be used in future studies such as those involving cybrid analysis and rescue experiments to verify the pathogenicity of novel variations (Haas et al. 2008). Should no defect be observed in fibroblasts, or if the clinical status calls for a rapid result, skeletal muscle biopsy should also be considered.
Relatively high numbers of enzyme assays return negative results in genetically verified cases of LS/LL (Sofou et al. 2014). In our study, the rate of negative assay results in genetically verified cases was 20%, excluding MT-ATP6 mutated cases. This observation implies that a normal MRC result in muscle and/or fibroblast cell line does not exclude the possibility of a mitochondrial disorder. A reasonable proportion of MRC defects may remain undetected if negative enzyme assay results prevent us from proceeding to genetic analysis. Interestingly, negative assay results were more frequently observed in cases with nDNA than mtDNA mutations. In addition, genetic causes such as ECHS1 mutations, which are not directly related to components of the MRC complexes, have been associated with LS/LL. In such cases, each separate MRC complex may not show reduced activity and thus remain undetected by enzyme assay. If marker substances detected by basic metabolic analysis leads directly to diagnosis, as is the case with urinary organic acids in ECHS1 mutation, the next step is to proceed directly to analyzing the candidate gene.
In addition to genetic screening and spectrophotometric assays that measure the activity of individual respiratory complexes, we used microscale oxygraphy to help analyze mitochondrial activity. Microscale oxygraphy has a high efficiency for detecting mitochondrial respiratory defects in genetically proven mitochondrial disease patients, an observation by Invernizzi but not adopted by many diagnostic laboratories (Invernizzi et al. 2012). Half the cases in our cohort with no apparent defect in activities of MRC complexes showed a significant decline in OCR. Moreover, two nDNA mutations were identified in this group. Although evidence needs to be accumulated, this finding suggests the promising value of microscale oxygraphy as a screening tool to detect MRC defect, especially in cases in whom each complex remains intact. If cellular OCR shows a significant reduction, genetic screening should be considered, even if MRC defects were not detected by enzyme assays of fibroblasts or peripheral organs.
With advances in molecular technologies, genetic screening is becoming increasingly utilized over enzyme analysis and invasive biopsies (Lake et al. 2016; Taylor et al 2014). Enzyme assays are considered a confirmatory method for diagnosis of LS/LL in cases with ambiguous genetic results or where genetic analysis fails to detect causative mutations (Morava and Brown 2015). However, in our study, gene analysis could not identify underlying mutations in 45% of cases with reduced MRC complex activities. The genetic spectrum of LS/LL is still expanding, and biochemical data obtained via enzyme assays enable the efficient selection of candidate genes (Thorburn et al. 2004) and provide essential information in the pathogenicity of identified gene variants. Thus, enzyme analysis remains an important part of the diagnostic process of mitochondrial disorders.
Based on our increasing understanding of the biological and molecular background of the disease, new therapeutic methods are being proposed (Martinelli et al. 2012; Morava and Brown 2015). Precise biochemical and genetic diagnosis is imperative in considering the possible gene-specific therapeutic options. It is also essential to provide appropriate genetic counseling. All available biochemical and molecular methods should be combined to not only diagnose the disease but also to provide optimal care to the LS/LL patients.
References
Baertling F, Rodenburg RJ, Schaper J et al (2014) A guide to diagnosis and treatment of Leigh syndrome. J Neurol Neurosurg Psychiatry 85(3):257–265
Bernier FP, Boneh A, Dennett X, Chow CW, Cleary MA, Thorburn DR (2002) Diagnostic criteria for respiratory chain disorders in adults and children. Neurology 59(9):1406–1411
Bruno C, Sacco O, Santorelli FM et al (2003) Mitochondrial myopathy and respiratory failure associated with a new mutation in the mitochondrial transfer ribonucleic acid glutamic acid gene. J Child Neurol 18(4):300–303
Budde SM, van den Heuvel LP, Janssen AJ et al (2000) Combined enzymatic complex I and III deficiency associated with mutations in the nuclear encoded NDUFS4 gene. Biochem Biophys Res Commun 275(1):63–68
Cameron JM, Janer A, Levandovskiy V et al (2011) Mutations in iron-sulfur cluster scaffold genes NFU1 and BOLA3 cause a fatal deficiency of multiple respiratory chain and 2-oxoacid dehydrogenase enzymes. Am J Hum Genet 89(4):486–495
Fernandez-Moreira D, Ugalde C, Smeets R et al (2007) X-linked NDUFA1 gene mutations associated with mitochondrial encephalomyopathy. Ann Neurol 61(1):73–83
Gerards M, Kamps R, van Oevelen J et al (2013) Exome sequencing reveals a novel Moroccan founder mutation in SLC19A3 as a new cause of early-childhood fatal Leigh syndrome. Brain 136(3):882–890
Gropman AL (2013) Neuroimaging in mitochondrial disorders. Neurotherapeutics 10(2):273–285
Haack TB, Rolinski B, Haberberger B et al (2013) Homozygous missense mutation in BOLA3 causes multiple mitochondrial dysfunctions syndrome in two siblings. J Inherit Metab Dis 36(1):55–62
Haas RH, Parikh S, Falk MJ et al (2008) The in-depth evaluation of suspected mitochondrial disease. Mol Genet Metab 94(1):16–37
Heuvel LP, Smeitink JA, Rodenburg RJT (2004) Biochemical examination of fibroblasts in the diagnosis and research of oxidative phosphorylation (OXPHOS) defects. Mitochondrion 4(5-6):395–401
Invernizzi F, D’Amato I, Jensen PB, Ravaqlia S, Zeviani M, Tiranti V (2012) Microscale oxygraphy reveals OXPHOS impairment in MRC mutant cells. Mitochondrion 12(2):328–335
Kirby DM, Crawford M, Cleary MA, Dahl HH, Dennett X, Thorburn DR (1999) Respiratory chain complex I deficiency: an underdiagnosed energy generation disorder. Neurology 52(6):1255–1264
Kirby DM, McFarland R, Ohtake A et al (2004) Mutations of the mitochondrial ND1 gene as a cause of MELAS. J Med Genet 41(10):784–789
Kohda M, Tokuzawa Y, Kishita Y et al (2016) A comprehensive genomic analysis reveals the genetic landscape of mitochondrial respiratory chain complex deficiencies. PLoS Genet 12(1):e1005679. doi:10.1371/journal.pgen.1005679
Kopajtich R, Nicholls TJ, Rorbach J et al (2014) Mutations in GTPBP3 cause a mitochondrial translation defect associated with hypertrophic cardiomyopathy, lactic acidosis, and encephalopathy. Am J Hum Genet 95(6):708–720
Lake NJ, Compton AG, Rahman S, Thorburn DR (2016) Leigh syndrome: one disorder, more than 75 monogenic causes. Ann Neurol 79(2):190–203
Leigh D (1951) Subacute necrotizing encephalomyelopathy in an infant. J Neurol Neurosurg Psychiatry 1(14):216–221
Martinelli D, Catteruccia M, Piemonte F et al (2012) EPI-743 reverses the progression of the pediatric mitochondrial disease--genetically defined Leigh syndrome. Mol Genet Metab 107(3):383–388
McKenzie M, Tucker EJ, Compton AG et al (2011) Mutations in the gene encoding C8orf38 block complex I assembly by inhibiting production of the mitochondria-encoded subunit ND1. J Mol Biol 414(3):413–426
Morava E, Brown GK (2015) Next generation mitochondrial disease: change in diagnostics with eyes on therapy. J Inherit Metab Dis 38(3):387–388
Munnich A, Rustin P (2001) Clinical spectrum and diagnosis of mitochondrial disorders. Am J Med Genet 106(1):4–17
Murayama K, Nagasaka H, Tsuruoka T et al (2009) Intractable secretory diarrhea in a Japanese boy with mitochondrial respiratory chain complex I deficiency. Eur J Pediatr 168(3):297–302
Peters H, Buck N, Wanders R et al (2014) ECHS1 mutations in Leigh disease: a new inborn error of metabolism affecting valine metabolism. Brain 137(Pt 11):2903–2908
Rahman S, Blok RB, Dahl H-HM et al (1996) Leigh syndrome: clinical features and biochemical and DNA abnormalities. Ann Neurol 39(3):343–351
Saudubray J-M, Charpentier C (2001) Clinical phenotypes: diagnosis/algorithms. In: Scriver CR, Sly WS (eds) The metabolic and molecular bases of inherited diseases, 8th edn. McGraw-Hills, New York, pp 1327–1403
Sofou K, De Coo IF, Isohanni P et al (2014) A multicenter study on Leigh syndrome: disease course and predictors of survival. Orphanet J Rare Dis 9:52
Spruijt L, Smeets HJ, Hendrickx A et al (2007) A MELAS-associated ND1 mutation causing leber hereditary optic neuropathy and spastic dystonia. Arch Neurol 64(6):890–893
Taylor RW, Pyle A, Griffin H et al (2014) Use of whole-exome sequencing to determine the genetic basis of multiple mitochondrial respiratory chain complex deficiencies. JAMA 312(1):68–77
Thorburn DR, Rahman S (1993) Mitochondrial DNA-associated Leigh syndrome and NARP. In: Pagon RA, Adam MP, Ardinger HH et al (eds) GeneReviews. University of Washington, Seattle
Thorburn DR, Chow CW, Kirby DM (2004) Respiratory chain enzyme analysis in muscle and liver. Mitochondrion 4(5–6):363–375
Tiranti V, Hoertnagel K, Carrozzo R et al (1998) Mutations of SURF-1 in Leigh disease associated with cytochrome c oxidase deficiency. Am J Hum Genet 63(6):1609–1621
Uehara N, Mori M, Tokuzawa Y et al (2014) New MT-ND6 and NDUFA1 mutations in mitochondrial respiratory chain disorders. Ann Clin Transl Neurol 1(5):361–369
Yamada K, Aiba K, Kitaura Y et al (2015) Clinical, biochemical and metabolic characterization of a mild form of human short-chain enoyl-CoA hydratase deficiency: significance of increased N-acetyl-S-(2-carboxypropyl)cysteine excretion. J Med Genet 52(10):691–698
Acknowledgements
We thank all the patients and their doctors in charge for supplying us with data. We also thank Dr Holger Prokisch and Mr Vicente Yepez for their professional advice.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
None.
Details of funding
This work was supported in part by the Practical Research Project for Rare/Intractable Diseases from the Japan Agency for Medical Research and Development, AMED to Kei Murayama (http://www.amed.go.jp/en/) and the Project Promoting Clinical Trials for Development of New Drugs and Medical Devices, Japan Medical Association, from the Japan Agency for Medical Research and Development, AMED to Akira Ohtake (http://www.jmacct.med.or.jp/en/what-we-do/investigator.html).
This work was also supported by an Innovative Cell Biology by Innovative Technology grant (Cell Innovation Program) from the Ministry of Education, Culture, Sports, Science and Technology (MEXT), Japan to Yasushi Okazaki (http://cell-innovation.nig.ac.jp/mext-life/english/index.html), the Support Project, and a Strategic Research Center in Private Universities grant from MEXT, Japan to Saitama Medical University Research Center for Genomic Medicine (http://www.mext.go.jp/a_menu/koutou/shinkou/07021403/002/002/1218299.htm). Further, this work was supported by Grants-in-Aid of the Research on Intractable Diseases (Mitochondrial Disorder) from the Ministry of Health, Labor and Welfare of Japan, and a special research grant from Takeda Science Foundation (http://www.takeda-sci.or.jp/) to YO. The authors confirm independence from the sponsors.
Informed consent
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000. Informed consent was obtained from parents of all patients for being included in the study.
Additional information
Communicated by: Shamima Rahman
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Ogawa, E., Shimura, M., Fushimi, T. et al. Clinical validity of biochemical and molecular analysis in diagnosing Leigh syndrome: a study of 106 Japanese patients. J Inherit Metab Dis 40, 685–693 (2017). https://doi.org/10.1007/s10545-017-0042-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10545-017-0042-6