Abstract
Alkaptonuria (AKU) is a rare inherited metabolic disorder of tyrosine metabolism that results from a defect in an enzyme called homogentisate 1,2-dioxygenase. The result of this is that homogentisic acid (HGA) accumulates in the body. HGA is central to the pathophysiology of this disease and the consequences observed; these include spondyloarthropathy, rupture of ligaments/muscle/tendons, valvular heart disease including aortic stenosis and renal stones. While AKU is considered to be a chronic progressive disorder, it is clear from published case reports that fatal acute metabolic complications can also occur. These include oxidative haemolysis and methaemoglobinaemia. The exact mechanisms underlying the latter are not clear, but it is proposed that disordered metabolism within the red blood cell is responsible for favouring a pro-oxidant environment that leads to the life threatening complications observed. Herein the role of red blood cell in maintaining the redox state of the body is reviewed in the context of AKU. In addition previously reported therapeutic strategies are discussed, specifically with respect to why reported treatments had little therapeutic effect. The potential use of nitisinone for the management of patients suffering from the acute metabolic decompensation in AKU is proposed as an alternative strategy.


Similar content being viewed by others
Abbreviations
- AKU:
-
Alkaptonuria
- HGA:
-
Homogentisic acid
- HGD:
-
Homogentisate-1,2-dioxygenase
- BQA:
-
1,4-benzoquinone-2-acetic acid
- AKI:
-
Acute kidney injury
- CKD:
-
Chronic kidney disease
- NAC:
-
N-acetyl cysteine
- RBCs:
-
Red blood cells
- MetHb:
-
Methaemoglobin
- PPP:
-
Pentose phosphate pathway
- NADH:
-
Nicotinamide adenine dinucleotide
- NADPH:
-
Nicotinamide adenine dinucleotide phosphate
- ROS:
-
Reactive oxygen species
- G6PD:
-
Glucose-6-phosphate dehydrogenase
References
Abreo K, Abreo F, Zimmerman SW et al (1983) A fifty-year-old man with skin pigmentation, arthritis, chronic renal failure and methemoglobinemia. Am J Med Genet 14:97–114
Agarwal R, Vasavada N, Sachs NG et al (2004) Oxidative stress and renal injury with intravenous iron in patients with chronic kidney disease. Kid Inter 65:2279–2289
Al-Omar MA, Beedham C, Alsarra IA (2004) Pathological roles of reactive oxygen species and their defence mechanisms. Saudi Pharm J 12:1–18
Bataille S, Moal V, Aquaron RR et al (2014) Hemolysis: a fatal complication of alkaptonuria in a severe renal failure patient. Clin Nephrol 81(5):374–376
Beutler E, Baluda MC (1963) Methemoglobin reduction. Studies of the interaction between cell populations and of the role of methylene blue. Blood 22:323–333
Braconi D, Millucci L, Bernardini G et al (2015) Oxidative stress and mechanisms of ochronosis in alkaptonuria. Free Radic Biol Med. doi:10.1016/j.freeradbiomed.2015.02.021i
Burak Cimen MY (2008) Free radical metabolism in human erthyrocytes. Clin Chim Acta 390:1–11
Cappellini MD, Fiorelli G (2008) Glucose-6-phosphate dehydrogenase deficiency. Lancet 371:64–74
Ceballos-Picot I, Witko-Sarsat V, Merad-Boudia M et al (1996) Glutathione antioxidant system as a marker of oxidative stress in chronic renal failure. Free Radic Biol Med 21:845–853
Davison AS, Milan AM, Hughes AT et al (2015) Serum concentrations and urinary excretion of tyrosine and homogentisic acid in normal subjects. Clin Chem Lab Med 53:e81–e83
De Laet C, Munoz VT, Jaeken J, FranÅois B et al (2011) Neuropsychological outcome of NTBC-treated patients with tyrosinaemia type 1. Develop Med Child Neurol 53:962–964
Faria B, Vidinha J, Pêgo C et al (2012) Impact of chronic kidney disease on the natural history of alkaptonuria. Clin Kidney J 5:352–355
Hegedus ZL, Nayak U (1994) Homogentesic acid and structurally related compounds as intermediates in plasma soluble melanin formation and soft tissue toxicities. Arch Int Physiol Biochim Biophys 102:175–181
Heng AE, Courbebaisse M, Kemeny JL et al (2010) Hemolysis in a patient with alkaptonuria and chronic kidney failure. Am J Kidney Dis 56:e1–e4
Himmelfarb J, McMonagle E, Freedman S et al The PICARD Group (2004) Oxidative stress is increased in critically ill patients with acute renal failure. J Am Soc Nephrol 15:2449–2456
Inagi R, Miyata T (1999) Oxidative protein damage with carbohydrates and lipids in uremia: ‘carbonyl stress’. Blood Purif 17:95–98
Introne WJ, Phornphutkul C, Bernardini I et al (2002) Exacerbation of the ochronosis of alkaptonuria due to renal insufficiency and improvement after renal transplantation. Mol Genet Metab 77:136–142
Introne WJ, Perry MB, Troendle J et al (2011) A 3-year randomized therapeutic trial of nitisinone in alkaptonuria. Mol Genet Metab 103:307–314
Karkouti K (2012) Transfusion and risk of acute kidney injury in cardiac surgery. Br J Anaesth 109:i29–i38
Kazancioglu R, Taylan I, Aksak F et al (2004) Alkaptonuria and renal failure: a case report. J Nephrol 17:441–445
Liu W, Prayson RA (2001) Dura mater involvement in ochronosis (alkaptonuria). Arch Pathol Lab Med 125:961–963
Masella R, Benedetto R, Vary R et al (2005) Novel mechanisms of natural antioxidant compounds in biological systems: involvement of glutathione and glutathione-related enzymes. J Nutr Biochem 16:577–586
Mayorandan S, Meyer U, Gokcay G et al (2014) Cross-sectional study of 168 patients with hepatorenal tyrosinaemia and implications for clinical practice. Orphanet J Rare Dis 9:107
McKiernan PJ (2013) Nitisinone for the treatment of hereditary tyrosinemia type I. Exp Opin Orphan Drug 1:491–497
Milch RA (1960) Studies of alcaptonuria: inheritance of 47 cases in eight highly inter-related Dominican kindreds. Am J Hum Genet 12:76–85
Millucci L, Spreafico A, Tinti L, Braconi D et al (2012) Alkaptonuria is a novel human secondary amyloidogenic disease. Biochim Biophys Acta 1822:1682–1691
Millucci L, Braconi D, Bernardini G, Lupetti P et al (2015) Amyloidosis in alkaptonuria. J Inherit Metab Dis 38:797–805
Miyasaka C, Ohe C, Takahashi H et al (2013) An autopsy case of methemoglobinemia with ochronosis. Shindan Byori. Jpn J Diagn Pathol 30:112–117 (in Japanese)
Miyata T, Saito A, Kurokawa K, van Persele Y, de Strihou C (2001) Advance glycation and lipoxidation end products: reactive carbonyl compounds-related uraemic toxicity. Nephrol Dial Transplant 16(4):8–11
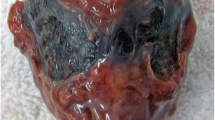
Mullan A, Cocker D, Taylor G et al (2015) Fatal oxidative haemolysis and methaemoglobinaemia in a patient with alkaptonuria and acute kidney injury. Clin Kidney J 8:109–112
Olszewska M (2004) The effect of hemodialysis on some parameters of the antioxidant system in the blood of patients with chronic renal failure. Ann Acad Med Stetin 50:41–52
Phomphutkul C, Introne WJ, Perry MB et al (2002) Natural history of alkaptonuria. N Eng J Med 347:2111–2121
Preston AJ, Keenan CM, Sutherland H et al (2014) Ochronotic osteoarthropathy in a mouse model of alkaptonuria, and its inhibition by nitisinone. Ann Rheum Dis 73:284–289
Ranganath LR, Jarvis JC, Gallagher JA (2013) Recent advances in management of alkaptonuria. J Clin Pathol 66:367–373
Ranganath LR, Milan AM, Hughes AT et al (2014) Suitability of nitisinone in Alkaptonuria 1 (SONIA 1): an international, multicentre, randomised, open-label, no-treatment controlled, parallel-group, dose–response study to investigate the effect of once daily nitisinone on 24-h urinary homogentisic acid excretion in patients with alkaptonuria after 4 weeks of treatment. Ann Rheum Dis [Epub ahead of print]. doi:10.1136/annrheumdis-2014-206033
Simons JP, Al-Shawi R, Ellmerich S et al (2013) Pathogenetic mechanisms of amyloid A amyloidosis. P Natl Acad Sci USA 110:16115–16120
Skold A, Cosco DL, Klein R (2011) Methemoglobinemia: pathogenesis, diagnosis, and management. South Med J 104:757–761
Stepniewska J, Ciechanowski K (2005) Oxidative stress as a reason of treatment difficulties in chronic renal failure. Pol Merkur Lekarski 19:697–700
Stepniewska J, Dolegowska B, Ciechanowski K et al (2006) Erythrocyte antioxidant defense system in patients with chronic renal failure according to the hemodialysis conditions. Arch Med Res 37:353–359
Stewart RMK, Briggs MC, Jarvis JC et al (2014) Reversible keratopathy due to hypertyrosinaemia following intermittent low-dose nitisinone in alkaptonuria: a case report. JIMD Rep 17:1–6
Suehiro K, Rinka H, Matsuura K et al (2007) A case of alkaptonuria with severe methemoglobinemia. Nihon Rinsho Kyukyu Igakukai Zasshi. J Jpn Soc Emer Med 10:71–75 (in Japanese)
Suwannarat P, O’Brien K, Perry MB et al (2005) Use of nitisinone in patients with alkaptonuria. Metab Clin Exp 54:719–728
Thimm E, Herebian D, Assmann B, Klee D, Mayatepek E, Spiekerkoetter U (2011) Increase of CSF tyrosine and impaired serotonin turnover in tyrosinemia type I. Mol Genet Metab 102:122–125
Uchiyama C, Kondoh H, Shintani H (2010) Acute methemoglobinemia associated with ochronotic valvular heart disease: report of a case. Thorac Cardiov Surg 58:113–119
Urieli-Shoval S, Linke RP, Matzner Y (2000) Expression and function of serum amyloid A, a major acute-phase protein, in normal and disease states. Curr Opin Hematol 7:64–69
Venkataseshan VS, Chandra B, Graziano V et al (1992) Alkaptonuria and renal failure: a case report and review of the literature. Mod Pathol 5:464–471
Zannoni VG, Lomtevas N, Goldfiner S (1969) Oxidation of homogentisic acid to ochronotic pigment in connective tissue. Biochim Biophys Acta 177:94
Zatkova A (2011) An update on molecular genetics of alkaptonuria (AKU). J Inherit Metab Dis 34:1127–1136
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical Standards
All procedures reported in this review were in accordance with the ethical standards of the local Hospital ethics committee and with the Helsinki Declaration of 1975, as revised in 2000.
Informed Consent
Informed consent was obtained from patient(s) wherever included in this review.
Ethical Approval
This article does not contain any studies with human or animal subjects performed by the any of the authors.
Conflict of interest
None.
Additional information
Communicated by: Daniela Karall
Rights and permissions
About this article
Cite this article
Davison, A.S., Milan, A.M., Gallagher, J.A. et al. Acute fatal metabolic complications in alkaptonuria. J Inherit Metab Dis 39, 203–210 (2016). https://doi.org/10.1007/s10545-015-9902-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10545-015-9902-0