Abstract
Background
Tyrosinaemia type 1 (HT1) is a rare disorder of tyrosine metabolism leading to liver failure and hepatocellular carcinoma. Treatment previously consisted of dietary restriction and orthotopic liver transplantation (OLT) but was transformed by the introduction of nitisinone in 1992. We describe the impact of nitisinone on the outcome and need for OLT in a single centre.
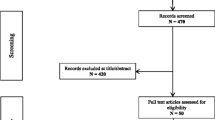
Methods
A retrospective analysis was performed of patients treated for HT1 at Birmingham Children’s Hospital from 1989–2009.
Results
Thirty eight patients were treated during the study period. Prior to 1992 6/7 (85.7 %) underwent OLT compared to 7/31 (22.6 %) after 1992 (p = 0.004) when nitisinone treatment was available. Furthermore, nitisinone-treated patients proceeding to OLT started treatment at a median age of 428 (86–821) days compared to 52 (2–990) days in those who did not (p = 0.004). Pre-OLT calculated glomerular filtration rate (cGFR) was similar in both groups but nitisinone prevented early decline after OLT (pre-nitisinone median 99.8 to 45.8 ml/min/1.73 m2, p = 0.02 versus nitisinone-treated group median 104.3 to 89.9 ml/min/1.73 m2, p = 0.5). Urinary protein:creatinine ratio (PCR) fell post-OLT to within the normal range for those treated with nitisinone but remained elevated in those not treated with nitisinone. Tubular reabsorption of phosphate (TRP) was normal or near normal in both groups pre-OLT and post-OLT. Hypertension was commoner and more severe in those not treated with nitisinone.
Conclusions
Nitisinone reduces the need for OLT particularly when started early. For those progressing to OLT the use of prior nitisinone therapy results in a preservation of their subsequent renal function.



Similar content being viewed by others
References
al-Dhalimy M, Overturf K, Finegold M, Grompe M (2002) Long-term therapy with NTBC and tyrosine-restricted diet in a murine model of hereditary tyrosinemia type I. Mol Genet Metab 75:38–45
Arnon R, Annunziato R, Miloh T et al (2011) Liver transplantation for hereditary tyrosinemia type I: analysis of the UNOS database. Pediatr Transplant 15:400–405
Arora-Gupta N, Davies P, McKiernan P, Kelly DA (2004) The effect of long-term calcineurin inhibitor therapy on renal function in children after liver transplantation. Pediatr Transplant 8:145–150
Bartlett DC, Preece MA, Holme E, Lloyd C, Newsome PN, Mckiernan PJ (2013) Plasma succinylacetone is persistently raised after liver transplantation in tyrosinaemia type 1. J Inherit Metab Dis 36:15–20
Baumann U, Duhme V, Auth MK, McKiernan PJ, Holme E (2006) Lectin-reactive alpha-Fetoprotein in patients with tyrosinemia Type I and hepatocellular carcinoma. J Pediatr Gastroenterol Nutr 43:77–82
Forget S, Patriquin HB, Dubois J et al (1999) The kidney in children with tyrosinemia: sonographic, CT and biochemical findings. Pediatr Radiol 29:104–108
Grompe M, St-Louis M, Demers SI, al-Dhalimy M, Leclerc B, Tanguay RM (1994) A single mutation of the fumarylacetoacetate hydrolase gene in French Canadians with hereditary tyrosinemia type I. N Engl J Med 331:353–357
Holme E, Lindstedt S (2000) Nontransplant treatment of tyrosinemia. Clin Liver Dis 4:805–814
Hutchesson AC, Hall SK, Preece MA, Green A (1996) Screening for tyrosinaemia type I. Arch Dis Child Fetal Neonatal Ed 74:F191–F194
Laberge C, Grenier A, Valet JP, Morissette J (1990) Fumarylacetoacetase measurement as a mass-screening procedure for hereditary tyrosinemia type I. Am J Hum Genet 47:325–328
Laine J, Salo MK, Krogerus L, Karkkainen J, Wahlroos O, Holmberg C (1995) The nephropathy of type I tyrosinemia after liver transplantation. Pediatr Res 37:640–645
Larochelle J, Alvarez F, Bussieres JF et al (2012) Effect of nitisinone (NTBC) treatment on the clinical course of hepatorenal tyrosinemia in Quebec. Mol Genet Metab 107:49–54
Lindstedt S, Holme E, Lock EA, Hjalmarson O, Strandvik B (1992) Treatment of hereditary tyrosinaemia type I by inhibition of 4-hydroxyphenylpyruvate dioxygenase. Lancet 340:813–817
Mckiernan PJ (2006) Nitisinone in the treatment of hereditary tyrosinaemia type 1. Drugs 66:743–750
Mieles LA, Esquivel CO, Van Thiel DH et al (1990) Liver transplantation for tyrosinemia. A review of 10 cases from the University of Pittsburgh. Dig Dis Sci 35:153–157
Mohan N, McKiernan P, Preece MA et al (1999) Indications and outcome of liver transplantation in tyrosinaemia type 1. Eur J Pediatr 158(Suppl 2):S49–S54
National Kidney Foundation (2002) K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Am J Kidney Dis 39:S1–S266
Paradis K, Weber A, Seidman EG et al (1990) Liver transplantation for hereditary tyrosinemia: the Quebec experience. Am J Hum Genet 47:338–342
Russo PA, Mitchell GA, Tanguay RM (2001) Tyrosinemia: a review. Pediatr Dev Pathol 4:212–221
Schwartz GJ, Brion LP, Spitzer A (1987) The use of plasma creatinine concentration for estimating glomerular filtration rate in infants, children, and adolescents. Pediatr Clin N Am 34:571–590
Shoemaker LR, Strife CF, Balistreri WF, Ryckman FC (1992) Rapid improvement in the renal tubular dysfunction associated with tyrosinemia following hepatic replacement. Pediatrics 89:251–255
Tuchman M, Freese DK, Sharp HL, Ramnaraine ML, Ascher N, Bloomer JR (1987) Contribution of extrahepatic tissues to biochemical abnormalities in hereditary tyrosinemia type I: study of three patients after liver transplantation. J Pediatr 110:399–403
van Spronsen FJ, Bijleveld CM, van Maldegem BT, Wijburg FA (2005) Hepatocellular carcinoma in hereditary tyrosinemia type I despite 2-(2 nitro-4-3 trifluoro- methylbenzoyl)-1, 3-cyclohexanedione treatment. J Pediatr Gastroenterol Nutr 40:90–93
Weinberg AG, Mize CE, Worthen HG (1976) The occurrence of hepatoma in the chronic form of hereditary tyrosinemia. J Pediatr 88:434–438
Author information
Authors and Affiliations
Corresponding author
Additional information
Communicated by: K. Michael Gibson
Competing interests
Patrick McKiernan has undertaken consultancy work for Swedish Orphan Biovitrum which has the worldwide rights to Orfadin (nitisinone).
Rights and permissions
About this article
Cite this article
Bartlett, D.C., Lloyd, C., McKiernan, P.J. et al. Early nitisinone treatment reduces the need for liver transplantation in children with tyrosinaemia type 1 and improves post-transplant renal function. J Inherit Metab Dis 37, 745–752 (2014). https://doi.org/10.1007/s10545-014-9683-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10545-014-9683-x