Abstract
Pompe disease is a lysosomal storage disorder caused by acid α-glucosidase deficiency and characterized by progressive muscle weakness. Enzyme replacement therapy (ERT) has ameliorated patients’ perspectives, but reversal of skeletal muscle pathology remains a challenge. We studied pretreatment biopsies of 22 patients with different phenotypes to investigate to what extent fiber-type distribution and fiber-type-specific damage contribute to clinical diversity. Pompe patients have the same fiber-type distribution as healthy persons, but among nonclassic patients with the same GAA mutation (c.-32-13T>G), those with early onset of symptoms tend to have more type 2 muscle fibers than those with late-onset disease. Further, it seemed that the older, more severely affected classic infantile patients and the wheelchair-bound and ventilated nonclassic patients had a greater proportion of type 2x muscle fibers. However, as in other diseases, this may be caused by physical inactivity of those patients.





Similar content being viewed by others
References
Bell RD, MacDougall JD, Billeter R, Howald H (1980) Muscle fiber types and morphometric analysis of skeletal msucle in six-year-old children. Med Sci Sports Exerc 12:28–31
Drost MR, Schaart G, van Dijk P et al (2008) Both type 1 and type 2a muscle fibers can respond to enzyme therapy in Pompe disease. Muscle Nerve 37:251–255
Fukuda T, Roberts A, Ahearn M, Zaal K, Ralston E, Plotz PH, Raben N (2006) Autophagy and lysosomes in Pompe disease. Autophagy 2:318–320
Giesker D, Bowers GN Jr (1979) The comparative utility of serum creatine kinase versus serum aldolase in the evaluation of muscle disorders. Conn Med 43:699–704
Gojo K, Abe S, Ide Y (2002) Characteristics of myofibres in the masseter muscle of mice during postnatal growth period. Anat Histol Embryol 31:105–112
Griffin JL (1984) Infantile acid maltase deficiency. I. Muscle fiber destruction after lysosomal rupture. Virchows Arch B Cell Pathol Incl Mol Pathol 45:23–36
Grimby G, Aniansson A, Zetterberg C, Saltin B (1984) Is there a change in relative muscle fibre composition with age? Clin Physiol 4:189–194
Hesselink RP, Wagenmakers AJ, Drost MR, Van der Vusse GJ (2003) Lysosomal dysfunction in muscle with special reference to glycogen storage disease type II. Biochim Biophys Acta 1637:164–170
Hirschorn R, Reuser A (2001) Glycogen storage disease type II: acid alpha-glucosidase (Acid Maltase) deficiency. In: Scriver CR, Beaudet AL, Sly WS, Valle MD (eds) The metabolic and molecular bases of inherited disease. Mc Graw-Hill, pp 3389–3420
Kishnani PS, Corzo D, Leslie ND et al (2009) Early treatment with alglucosidase alpha prolongs long-term survival of infants with Pompe disease. Pediatr Res 66:329–335
Kishnani PS, Corzo D, Nicolino M et al (2007) Recombinant human acid [alpha]-glucosidase: major clinical benefits in infantile-onset Pompe disease. Neurology 68:99–109
Kishnani PS, Hwu WL, Mandel H, Nicolino M, Yong F, Corzo D, Infantile-Onset Pompe Disease Natural History Study Group (2006) A retrospective, multinational, multicenter study on the natural history of infantile-onset Pompe disease. J Pediatr 148:671–676
Kriketos AD, Baur LA, O’Connor J, Carey D, King S, Caterson ID, Storlien LH (1997) Muscle fibre type composition in infant and adult populations and relationships with obesity. Int J Obes Relat Metab Disord 21:796–801
Krupp LB, LaRocca NG, Muir-Nash J, Steinberg AD (1989) The fatigue severity scale. Application to patients with multiple sclerosis and systemic lupus erythematosus. Arch Neurol 46:1121–1123
Lexell J (1995) Human aging, muscle mass, and fiber type composition. J Gerontol A Biol Sci Med Sci 50 Spec No: 11–16
Lexell J, Taylor CC, Sjostrom M (1988) What is the cause of the ageing atrophy? Total number, size and proportion of different fiber types studied in whole vastus lateralis muscle from 15- to 83-year-old men. J Neurol Sci 84:275–294
Muller-Felber W, Horvath R, Gempel K et al (2007) Late onset Pompe disease: clinical and neurophysiological spectrum of 38 patients including long-term follow-up in 18 patients. Neuromuscul Disord 17:698–706
Raben N, Danon M, Gilbert AL et al (2003) Enzyme replacement therapy in the mouse model of Pompe disease. Mol Genet Metab 80:159–169
Raben N, Fukuda T, Gilbert AL et al (2005) Replacing acid alpha-glucosidase in Pompe disease: recombinant and transgenic enzymes are equipotent, but neither completely clears glycogen from type II muscle fibers. Mol Ther 11:48–56
Raben N, Ralston E, Chien YH et al (2010) Differences in the predominance of lysosomal and autophagic pathologies between infants and adults with Pompe disease: implications for therapy. Mol Genet Metab 101:324–331
Scelsi R, Marchetti C, Poggi P (1980) Histochemical and ultrastructural aspects of m. vastus lateralis in sedentary old people (age 65–89 years). Acta Neuropathol 51:99–105
Schoser B, Hill V, Raben N (2008) Therapeutic approaches in glycogen storage disease type II/Pompe Disease. Neurotherapeutics 5:569–578
Schoser BG, Muller-Hocker J, Horvath R, Gempel K, Pongratz D, Lochmuller H, Muller-Felber W (2007) Adult-onset glycogen storage disease type 2: clinico-pathological phenotype revisited. Neuropathol Appl Neurobiol 33:544–559
Shea L, Raben N (2009) Autophagy in skeletal muscle: implications for Pompe disease. Int J Clin Pharmacol Ther 47(Suppl 1):S42–S47
Straub V (2008) Diagnosis. In: Baethmann M, Straub V, Reuser AJJ (eds) Pompe disease. Bremen, UNI-MED, pp 51–54
Strothotte S, Strigl-Pill N, Grunert B et al (2010) Enzyme replacement therapy with alglucosidase alfa in 44 patients with late-onset glycogen storage disease type 2: 12-month results of an observational clinical trial. J Neurol 257:91–97
Thurberg BL, Lynch Maloney C, Vaccaro C et al (2006) Characterization of pre- and post-treatment pathology after enzyme replacement therapy for Pompe disease. Lab Invest 86:1208–1220
Turner DC, Eppenberger HM (1973) Developmental changes in creatine kinase and aldolase isoenzymes and their possible function in association with contractile elements. Enzyme 15:224–238
van Capelle CI, Winkel LP, Hagemans ML et al (2008) Eight years experience with enzyme replacement therapy in two children and one adult with Pompe disease. Neuromuscul Disord 18:447–452
van den Berg LE, de Vries JM, Verdijk RM, van der Ploeg AT, Reuser AJ, van Doorn PA (2011) A case of adult Pompe disease presenting with severe fatigue and selective involvement of type 1 muscle fibers. Neuromuscul Disord 21:232–234
van den Hout HM, Hop W, van Diggelen OP et al (2003) The natural course of infantile Pompe’s disease: 20 original cases compared with 133 cases from the literature. Pediatrics 112:332–340
Van den Hout JM, Kamphoven JH, Winkel LP et al (2004) Long-term intravenous treatment of Pompe disease with recombinant human alpha-glucosidase from milk. Pediatrics 113:e448–e457
van der Ploeg AT, Clemens PR, Corzo D et al (2010) A randomized study of alglucosidase alfa in late-onset Pompe’s disease. N Engl J Med 362:1396–1406
Winkel LP, Hagemans ML, van Doorn PA, Loonen MC, Hop WJ, Reuser AJ, van der Ploeg AT (2005) The natural course of non-classic Pompe’s disease; a review of 225 published cases. J Neurol 252:875–884
Winkel LP, Kamphoven JH, van den Hout HJ, Severijnen LA, van Doorn PA, Reuser AJ, van der Ploeg AT (2003) Morphological changes in muscle tissue of patients with infantile Pompe’s disease receiving enzyme replacement therapy. Muscle Nerve 27:743–751
Wokke JH, Escolar DM, Pestronk A et al (2008) Clinical features of late-onset Pompe disease: a prospective cohort study. Muscle Nerve 38:1236–1245
Acknowledgements
We thank patients and parents for participating in the study; and J. Hardon, H. Nelisse, and T. Oskam for their contribution to the study as research nurses.
The research on Pompe disease at Erasmus MC was financially supported by the Erasmus MC Revolving Fund (NAMEvdB, project no 1054), ZonMw-Dutch organization for healthcare research and innovation of care [Grant 152001005], The ‘Prinses Beatrix Fonds’ (project number OP07-08) and the European Union, 7th Framework Program “EUCLYD-a European Consortium for Lysosomal Storage Diseases” of the European Union (health F2/2008 grant agreement 201678).
Competing interest
As of August 2004, ATvdP and AJR provide consulting services for Genzyme Corp, Cambridge, MA, USA, under an agreement between Genzyme Corp and Erasmus MC, Rotterdam, the Netherlands. This agreement also caters to financial support for Erasmus MC for research in Pompe disease. Erasmus MC and inventors for the method of treatment of Pompe’s disease by ERT receive royalty payments pursuant to Erasmus MC policy on inventions, patents and technology transfer.
Author information
Authors and Affiliations
Corresponding author
Additional information
Communicated by: Ed Wraith
Electronic supplementary material
Below is the link to the electronic supplementary material.
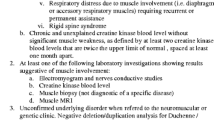
Supplementary Figure 1
The percentage of a types 1 and 2 muscle fibers, and b percentage of type 2a and type 2x muscle fibers in classic infantile patients and nonclassic patients. Significance between the different groups of patients is shown by * (P < 0.05). (JPEG 22 kb)
Supplementary Table 1
Patient characteristics (DOC 61 kb)
Supplementary Table 2
Degree of vacuolation per muscle-fiber type (percentage of fibers) (DOC 26 kb)
Rights and permissions
About this article
Cite this article
van den Berg, L.E.M., Drost, M.R., Schaart, G. et al. Muscle fiber-type distribution, fiber-type-specific damage, and the Pompe disease phenotype. J Inherit Metab Dis 36, 787–794 (2013). https://doi.org/10.1007/s10545-012-9541-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10545-012-9541-7