Abstract
Background
Metabolic treatment in glutaric aciduria type I (GA-I) including a low lysine diet with lysine-free, tryptophan-reduced amino acid supplements (AAS), carnitine supplementation and early start of emergency treatment during putatively threatening episodes of intermittent febrile illness dramatically improves the outcome and thus has been recommended by an international guideline group (Kölker et al, J Inherit Metab Dis 30:5–22, 2007). However, possible affection of linear growth, weight gain and biochemical follow-up monitoring has not been studied systematically.
Methods
Thirty-three patients (n = 29 asymptomatic, n = 4 dystonic) with GA-I who have been identified by newborn screening in Germany from 1999 to 2009 were followed prospectively during the first six years of life. Dietary treatment protocols, anthropometrical and biochemical parameters were longitudinally evaluated.
Results
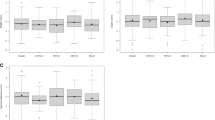
Mean daily intake as percentage of guideline recommendations was excellent for lysine (asymptomatic patients: 101 %; dystonic patients: 103 %), lysine-free, tryptophan-reduced AAS (108 %; 104 %), energy (106 %; 110 %), and carnitine (92 %; 102 %). Low lysine diet did not affect weight gain (mean SDS 0.05) but mildly impaired linear growth in asymptomatic patients (mean SDS −0.38), while dystonic patients showed significantly reduced weight gain (mean SDS −1.32) and a tendency towards linear growth retardation (mean SDS −1.03). Patients treated in accordance with recent recommendations did not show relevant abnormalities of routine biochemical follow-up parameters.
Interpretation
Low lysine diet promotes sufficient intake of essential nutrients and anthropometric development in asymptomatic children up to age 6 year, whereas individualized nutritional concepts are required for dystonic patients. Revised recommendations for biochemical monitoring might be required for asymptomatic patients.




Similar content being viewed by others
Abbreviations
- 3-OH-GA:
-
3-hydroxyglutaric acid
- AAS:
-
Amino acid supplements (lysine-free tryptophan-reduced, fortified with minerals, trace elements, and vitamins)
- ALAT:
-
Alanine aminotransferase
- ANOVA:
-
Analysis of variance
- ASAT:
-
Aspartate aminotransferase
- C5DC:
-
Glutarylcarnitine
- FAD:
-
Flavin adenine dinucleotide
- GA:
-
Glutaric acid
- GA-I:
-
Glutaric aciduria type I
- GCDH:
-
Glutaryl-CoA dehydrogenase
- GC/MS:
-
Gas chromatography/mass spectrometry
- MCV:
-
Mean corpuscular volume
- NBS:
-
Newborn screening
- SD(S):
-
Standard deviation (score)
- TCA:
-
Tricarboxylic acid cycle
- TSCSREG:
-
Times series cross sectional regression analysis
References
Abdi H (2007) Bonferroni and Sidak corrections for multiple comparisons. In: Salkind NJ (ed) Encyclopedia of measurement and statistics. Sage, Thousand Oaks, pp 103–107
Baric I, Wagner L, Feyh P, Liesert M, Buckel W, Hoffmann GF (1999) Sensitivity and specificity of free and total glutaric acid and 3-hydroxyglutaric measurements by stable-isotope dilution assays for the diagnosis of glutaric aciduria type I. J Inherit Metab Dis 22:867–881
Basinger AA, Booker JK, Frazier DM, Koeberl DD, Sullivan JA, Muenzer J (2006) Glutaric acidemia type 1 in patients of Lumbee heritage from North Carolina. Mol Genet Metab 88:90–92
Bjugstad KB, Goodman SI, Freed CR (2000) Age at symptom onset predicts severity of motor impairment and clinical outcome of glutaricacidemia type 1. J Pediatr 137:681–686
Boy Nikolas SP, Opp S, Heringer J, Okun JG, Sauer SW, Kölker S (2011) Glutaric aciduria type I: a translational approach to an enigmatic disease. J Pediatr Sci 3:e67
Christensen E (1983) Improved assay of glutaryl-CoA dehydrogenase in cultured cells and liver: application to glutaric aciduria type I. Clin Chim Acta 129:91–97
Cole TJ (1990) The LMS method for constructing normalized growth standards. Eur J Clin Nutr 44:45–60
D-A-CH (Deutsche Gesellschaft für Ernährung, Österreichische Gesellschaft für Ernährung, Schweizerische Gesellschaft für Ernährungsforschung, Schweizerische Vereinigung für Ernährung) (2000) Referenzwerte für die Nährstoffzufuhr. 1. Auflage, Umschau/Braus, Frankfurt/Main
Forstner R, Hoffmann GF, Gassner I et al (1999) Glutaric aciduria type I: ultrasonographic demonstration of early signs. Pediatr Radiol 29:138–143
Gauci C, Moranne O, Fouqueray B et al (2008) Pitfalls of measuring total blood calcium in patients with CKD. J Am Soc Nephrol 19:1592–1598
Goodman SI, Markey SP, Moe PG, Miles BS, Teng CC (1975) Glutaric aciduria: a “new” disorder of amino acid metabolism. Biochem Med 12:12–21
Goodman SI, Stein DE, Schlesinger S et al (1998) Glutaryl-CoA dehydrogenase mutations in glutaric acidemia (type I): review and report of thirty novel mutations. Hum Mut 12:141–144
Greenberg CR, Prasad AN, Dilling LA et al (2002) Outcome of the first 3-years of a DNA-based neonatal screening program for glutaric acidemia type 1 in Manitoba and nortwestern Ontario, Canada. Mol Genet Metab 75:70–78
Harting I, Neumaier-Probst E, Seitz A et al (2009) Dynamic changes of striatal and extrastriatal abnormalities in glutaric aciduria type I. Brain 132:1764–1782
Heringer J, Boy NPS, Ensenauer R et al (2010) Use of guidelines improves the neurological outcome in glutaric aciduria type I. Ann Neurol 68:743–752
Hoffmann GF, Athanassopoulos S, Burlina AB et al (1996) Clinical course, early diagnosis, treatment, and prevention of disease in glutaryl-CoA dehydrogenase deficiency. Neuropediatrics 27:115–123
Jafari P, Braissant O, Bonafé L, Ballhausen D (2011) The unsolved puzzle of neuropathogenesis in glutaric aciduria type I. Mol Genet Metab 104:425–437
Kölker S, Koeller DM, Okun JG, Hoffmann GF (2004) Pathomechanisms of neurodegeneration in glutaryl-CoA dehydrogenase deficiency. Ann Neurol 55:7–12
Kölker S, Garbade SF, Greenberg CR et al (2006) Natural history, outcome and therapeutic efficacy in children and adults with glutaryl-CoA dehydrogenase deficiency. Pediatr Res 59:840–847
Kölker S, Christensen E, Leonard JV et al (2007) Guideline for the diagnosis and management of glutaryl-CoA dehydrogenase deficiency (glutaric aciduria type I). J Inherit Metab Dis 30:5–22
Kölker S, Christensen E, Leonard JV et al (2011) Diagnosis and management of glutaric aciduria type I - revised recommendations. Inherit Metab Dis 34:677–694
Kromeyer-Hauschild K, Wabitsch M, Kunze D et al (2001) Perzentile für den Body-mass-Index für das Kinder- und Jugendalter unter Heranziehung verschiedener deutscher Stichproben. Monatsschr Kinderheilkd 149:807–818
Kyllerman M, Skjeldal O, Christensen E et al (2004) Long-term follow-up, neurological outcome and survival rate in 28 Nordic patients with glutaric aciduria type 1. Eur J Paediatr Neurol 8:121–129
Lamp J, Keyser B, Koeller DM, Ullrich K, Braulke T, Mühlhausen C (2011) Glutaric aciduria type 1 metabolites impair the succinate transport from astrocytic to neuronal cells. J Biol Chem 285:17777–17784
Lin SK, Hsu SG, Ho ES et al (2002) Novel mutations and prenatal sonographic findings of glutaric aciduria (type I) in two Taiwanese families. Prenat Diagn 22:725–729
Mellerio C, Marignier S, Roth P et al (2008) Prenatal ultrasound and MRI findings in glutaric aciduria type 1: a de novo case. Ultrasound Obstet Gynecol 31:712–714
Monavari AA, Naughten ER (2000) Prevention of cerebral palsy in glutaric aciduria type 1 by dietary management. Arch Dis Child 82:67–70
Müller E, Kölker S (2004) Reduction of lysine intake while avoiding malnutrition – major goals and major problems in dietary treatment of glutaryl-CoA dehydrogenase deficiency. J Inherit Metab Dis 27:903–910
Naughten ER, Mayne PD, Monavari AA, Goodman SI, Sulaiman G, Croke DT (2004) Glutaric Aciduria Type I, Outcome in the Republic of Ireland. J Inherit Metab Dis 27:917–920
Prader A, Largo RH, Molinari L, Issler C (1989) Physical growth of Swiss children from birth to 20 years of age. Helv Paediatr Acta Suppl 52:1–125
SAS Institute (2008) SAS/ETS 9.2 User’s Guide. SAS Institute, Cary
Sauer SW, Okun JG, Schwab MA et al (2005) Bioenergetics in glutaryl-coenzyme A dehydrogenase deficiency, a role for glutaryl-coenzyme A. J Biol Chem 280:21830–21836
Sauer SW, Okun JG, Fricker G et al (2006) Intracerebral accumulation of glutaric and 3-hydroxyglutaric acids secondary to limited flux across the blood–brain barrier constitute a biochemical risk factor for neurodegeneration in glutaryl-CoA dehydrogenase deficiency. J Neurochem 97:899–910
Sauer SW, Opp S, Mahringer A et al (2010) Glutaric aciduria type I and methylmalonic aciduria: stimulation of cerebral import and export of accumulating neurotoxic dicarboxylic acids in in vitro models of the blood–brain barrier and the choroid plexus. Biochem Biophys Acta 1802:551–560
Sauer SW, Opp S, Hoffmann GF, Koeller DM, Okun JG, Kölker S (2011) Therapeutic modulation of cerebral L-lysine metabolism in a mouse model for glutaric aciduria type I. Brain 134:157–170
Strauss KA, Puffenberger EG, Robinson DL, Morton DH (2003) Type I glutaric aciduria, part 1: natural history of 77 patients. Am J Med Genet 121C:38–52
Strauss KA, Lazovic J, Wintermark M, Morton DH (2007) Multimodal imaging of striatal degeneration in Amish patients with glutaryl-CoA dehydrogenase deficiency. Brain 130:1905–1920
Strauss KA, Donnelly P, Wintermark M (2010) Cerebral haemodynamics in patients with glutaryl-coenzyme A dehydrogenase deficiency. Brain 133:76–92
Thomas JA, Bernstein LE, Greene CL, Koeller DM (2000) Apparent decreased energy requirements in children with organic acidemias: preliminary observations. J Am Diet Assoc 100:1074–1076
van der Watt G, Owen EP, Berman P et al (2010) Glutaric aciduria type 1 in South Africa-high incidence of glutaryl-CoA dehydrogenase deficiency in black South Africans. Mol Genet Metab 101:178–182
Yannicelli S, Rohr F, Warman ML (1994) Nutrition support for glutaric acidemia type I. J Am Diet Assoc 94:183–188
Zinnanti WJ, Lazovic J, Housman C et al (2007) Mechanism of age-dependent susceptibility and novel treatment strategy in glutaric acidemia type I. J Clin Invest 117:3258–3270
Zschocke J, Quak E, Guldberg P, Hoffmann GF (2000) Mutation analysis in glutaric aciduria type I. J Med Genet 37:177–181
Acknowledgements & Funding
The study was supported by grants from the Kindness for Kids Foundation, Munich, Germany, and was continued with funding from the European Union for the project E-IMD (EAHC no. 2010 12 01), in the framework of the Health Programme 2008–2013 – both to S. K. and G. F. H. The authors declare no conflict of interest. We thank the patients with GA-I and their parents for participation in this study.
The authors confirm independence from the sponsors; the content of the article has not been influenced by the sponsors.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
Communicated by: Johan Lodewijk Karel Van Hove
Peter Burgard and Stefan Kölker contributed equally
Rights and permissions
About this article
Cite this article
Boy, N., Haege, G., Heringer, J. et al. Low lysine diet in glutaric aciduria type I – effect on anthropometric and biochemical follow-up parameters. J Inherit Metab Dis 36, 525–533 (2013). https://doi.org/10.1007/s10545-012-9517-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10545-012-9517-7