Abstract
Objective
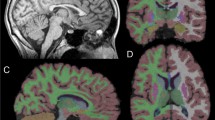
Metachromatic Leukodystrophy (MLD) is a rare disorder leading to demyelination and neurological impairment. A natural history study within the German leukodystrophy network analyzed MRI changes with respect to the clinical course.
Methods
113 MR images of 68 patients (33 late-infantile, 35 juvenile) were studied cross-sectionally and longitudinally. MRI and motor deterioration were assessed using standardized scoring systems.
Results
The temporal and spatial patterns of MR severity scores differed between the late-infantile and juvenile form. Although early (involving central white matter, corpus callosum) and late signs (involving pons, cerebellum, cerebral atrophy) were similar, high MRI scores (mean 18, SD 1.2, p < 0.001) were evident in the juvenile form already at the onset of first symptoms and even in presymptomatic patients. The progression rate of the MRI score was clearly higher and more uniform in the late-infantile (on average 8 per year, p < 0.0001) than in the juvenile patients (on average 0.4 per year, p < 0.08). In late-infantile patients, MRI changes correlated highly with motor deterioration (rho = 0.73, p < 0.001), this was less remarkable in the juvenile form (rho = 0.50, p < 0.01). Severe motor dysfunction was associated with U-fiber involvement and cerebellar changes (p < 0.05).
Conclusions
MRI showed a typical spatial pattern, which evolved gradually and uniformly during disease progression in late-infantile MLD. In juvenile MLD MRI changes were already observed at disease onset and temporal patterns were more variable. As therapeutic options for MLD are evolving, these findings are not only important for patient counseling but also for the evaluation of therapeutic interventions.



Similar content being viewed by others
References
Biffi A, Cesani M, Fumagalli F et al. (2008a) Metachromatic leukodystrophy - mutation analysis provides further evidence of genotype-phenotype correlation. Clin Genet 74:349–357
Biffi A, Lucchini G, Rovelli A, Sessa M (2008b) Metachromatic leukodystrophy: an overview of current and prospective treatments. Bone Marrow Transplant 42(Suppl 2):S2–S6
Black JW, Cumings JN (1961) Infantile metachromatic leukodystrophy. J Neurol Neurosurg Psychiatr 24:233–239
Costello DJ, Eichler AF, Eichler FS (2009) Leukodystrophies: classification, diagnosis, and treatment. Neurologist 15:319–328
Demaerel P, Faubert C, Wilms G, Casaer P, Piepgras U, Baert AL (1991) MR findings in leukodystrophy. Neuroradiology 33:368–371
Eichler F, Grodd W, Grant E et al. (2009) Metachromatic Leukodystrophy: A Scoring System for Brain MR Observations. AJNR Am J Neuroradiol 30:1893–1897
Faerber EN, Melvin J, Smergel EM (1999) MRI appearances of metachromatic leukodystrophy. Pediatr Radiol 29:669–672
Gieselmann V (2008) Metachromatic leukodystrophy: genetics, pathogenesis and therapeutic options. Acta Paediatr Suppl 97:15–21
Gieselmann V, Krägeloh-Mann I (2010) Metachromatic leukodystrophy–an update. Neuropediatrics 41:1–6
Gieselmann V, Franken S, Klein D et al. (2003) Metachromatic leukodystrophy: consequences of sulphatide accumulation. Acta Paediatr Suppl 92:74–79
Haberland C, Brunngraber E, Witting L, Daniels A (1973) Juvenile metachromatic leucodystrophy. Case report with clinical, histopathological, ultrastructural and biochemical observations. Acta Neuropathol 26:93–106
Heim P, Claussen M, Hoffmann B et al. (1997) Leukodystrophy incidence in Germany. Am J Med Genet 71:475–478
Jervis GA (1960) Infantile metachromatic leukodystrophy. (Greenfield's disease). J Neuropathol Exp Neurol 19:323–341
Kehrer C, Blumenstock G, Gieselmann V, and Krägeloh-Mann I (2011a) The natural course of gross motor deterioration in metachromatic leukodystrophy. Dev Med Child Neurol. accepted for publication.
Kehrer C, Blumenstock G, Raabe C, Krägeloh-Mann I (2011b) Development and reliability of a classification system for gross motor function in children with metachromatic leucodystrophy. Dev Med Child Neurol 53:156–160
Kim TS, Kim IO, Kim WS et al. (1997) MR of childhood metachromatic leukodystrophy. AJNR Am J Neuroradiol 18:733–738
Loes DJ, Hite S, Moser H et al. (1994) Adrenoleukodystrophy: a scoring method for brain MR observations. AJNR Am J Neuroradiol 15:1761–1766
Mahmood A, Raymond GV, Dubey P, Peters C, Moser HW (2007) Survival analysis of haematopoietic cell transplantation for childhood cerebral X-linked adrenoleukodystrophy: a comparison study. Lancet Neurol 6:687–692
Poorthuis BJ, Wevers RA, Kleijer WJ et al. (1999) The frequency of lysosomal storage diseases in The Netherlands. Hum Genet 105:151–156
Russel Brain W, Greenfield JG (1950) Late infantile metachromatic leuko-encephalopathy, with primary degeneration of the interfascicular oligodentroglia. Brain 73:291–317
Schiffmann R, van der Knaap MS (2009) Invited article: an MRI-based approach to the diagnosis of white matter disorders. Neurology 72:750–759
Shrout PE, Fleiss JL (1979) Intraclass correlations: uses in assessing rater reliability. Psychol Bull 86:420–428
van der Knaap MS, Valk J (2005) Magnetic resonance in myelin, myelination, and myelin disorders. Springer, Berlin
van der Voorn JP, Pouwels PJ, Kamphorst W et al. (2005) Histopathologic correlates of radial stripes on MR images in lysosomal storage disorders. AJNR Am J Neuroradiol 26:442–446
von Figura K, Gieselmann V, and Jacken J (2001) Metachromatic leukodystrophy. In Scriver CR, Beaudet AL, Sly WS et al., eds. The metabolic and molecular bases of inherited disease. New York: McGraw-Hill, 3695–3724
Zafeiriou DI, Kontopoulos EE, Michelakakis HM, Anastasiou AL, Gombakis NP (1999) Neurophysiology and MRI in late-infantile metachromatic leukodystrophy. Pediatr Neurol 21:843–846
Acknowledgements
The work was supported by a grant from the German Federal Ministry of Education and Research (LEUKONET). In addition we thank Professor Martin Staudt, Dr Marko Wilke and Professor Thomas Naegele (University Hospital Tübingen, Germany) for participating in the inter-rater test, and Professor Volkmar Gieselmann (Department of Physiology, University of Bonn, Germany, coordinator of the Leukonet) for critical and helpful comments on the manuscript. And we do thank the children and their families for their participation.
Author information
Authors and Affiliations
Corresponding author
Additional information
Communicated by Ed Wraith
Conflict of interest disclosures
The work was supported by a grant from the German Federal Ministry of Education and Research (LEUKONET).
Dr. Groeschel has received institutional research support from the German Federal Ministry of Education and Research and from Shire plc.
Dr. Kehrer has received institutional research support from the German Federal Ministry of Education and Research.
Dr. Engel reports no disclosures.
Dr. í Dali serves on a scientific advisory board for Shire plc and has received institutional research support from Shire plc and Zymenex A/S.
Dr. Bley has received institutional research support from the German Federal Ministry of Education and Research.
Dr. Steinfeld reports no disclosures.
Dr. Grodd reports no disclosures.
Dr. Krägeloh-Mann was member of the scientific board of the Scandinavian biopharmaceutical company ZYMENEX for a world-wide clinical trial I-study for enzyme replacement with the ZYMENEX’s product “Metazym” in 2007. This did not imply any involvement, nor funding in the present study.
All authors confirm independence of the sponsors; the content of the article has not been influenced by the sponsors.
Electronic supplementary materials
Below is the link to the electronic supplementary material.
Supplementary material Fig. 1
MR Severity score of patients with MLD according to chronological age. Lines connect follow-up scans of patients. Empty circles indicate MR scans of patients before the onset of first symptoms. (PPT 38 kb)
Supplementary material Fig. 2
Mean of subscores for the early, middle and late phase of the disease (scaled between 0–1). The numbers indicate specific brain areas depicted by the score. (1 parieto-occipital WM – central, 2 splenium of corpus callosum, 3 frontal WM – central, 4 parieto-occipital WM – periventricular, 5 temporal WM – central, 6 genu of corpus callosum, 7 frontal WM - periventricular, 8 temporal WM – periventricular, 9 pons, 10 parieto-occipital WM – subcortical, 11 posterior limb of internal capsule, 12 frontal WM – subcortical, 13 cerebellar atrophy, 14 cerebellar WM changes, 15 temporal WM – subcortical, 16 cerebral atrophy, 17 anterior limb of internal capsule) (PPT 58 kb)
Supplementary material Table 1
MR Severity Scoring System for MLD (Eichler et al. 2009). (DOC 25 kb)
Supplementary material, Table 2
Gross Motor Function Classification system for MLD (GMFC-MLD) (Kehrer et al. 2011b). (DOC 27 kb)
Supplementary material, Table 3
Correlation coefficients (Spearman’s rank) and their correlation p-value are given for the whole MR Severity Score and its subscores with the motor function score (GMFC-MLD) for the late-infantile and juvenile form of MLD. Highlighted correlation coefficients (in bold font) are remarkably high. (DOC 48 kb)
Rights and permissions
About this article
Cite this article
Groeschel, S., Kehrer, C., Engel, C. et al. Metachromatic leukodystrophy: natural course of cerebral MRI changes in relation to clinical course. J Inherit Metab Dis 34, 1095–1102 (2011). https://doi.org/10.1007/s10545-011-9361-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10545-011-9361-1