Abstract
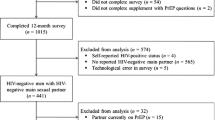
Pre-exposure prophylaxis (PrEP) affords an opportunity to significantly reduce the risk of HIV infection among male couples. We used cross-sectional dyadic data from 382 concordant-negative male couples to examine demographic and relationship characteristics associated with current PrEP use, willingness to use PrEP in the future, and perceived ability to adhere to PrEP using Actor–Partner Independence Models. Few partnered men reported currently using PrEP (16.4%) and 57.7% of non-users reported being unlikely to use PrEP in the future. Actor and partner perceptions of PrEP stigma significantly reduced PrEP use and perceptions of willingness to use PrEP or the ability to adhere to PrEP, while perceiving a higher prevalence of HIV among men was associated with significant increases in PrEP use, willingness and perceived ability to adhere. Perceptions that more friends would support PrEP use were also significantly associated with increases in willingness and perceived ability to adhere to PrEP. Dyadic interventions are needed to provide couples the skills to communicate about HIV risk and prevention, and address myths around the protective effect of relationships against HIV acquisition.
Similar content being viewed by others
References
Goodreau SM, Carnegie NB, Vittinghoff E, Lama JR, Sanchez J, Grinsztejn B, et al. What drives the US and Peruvian HIV epidemics in men who have sex with men (MSM)? PLoS One. 2012;7(11):e50522.
Sullivan PS, Salazar L, Buchbinder S, Sanchez TH. Estimating the proportion of HIV transmissions from main sex partners among men who have sex with men in five US cities. AIDS. 2009;23(9):1153–62.
Anglemyer A, Horvath T, Rutherford G. Antiretroviral therapy for prevention of HIV transmission in HIV-discordant couples. JAMA. 2013;310(15):1619–20.
Cohen MS, Chen YQ, McCauley M, Gamble T, Hosseinipour MC, Kumarasamy N, et al. Prevention of HIV-1 infection with early antiretroviral therapy. N Engl J Med. 2011;365(6):493–505.
Muessig KE, Smith MK, Powers KA, Lo Y-R, Burns DN, Grulich AE, et al. Does ART prevent HIV transmission among MSM? AIDS. 2012;26(18):2267–73.
Mitchell JW, Horvath KJ. Factors associated with regular HIV testing among a sample of US MSM with HIV-negative main partners. J Acquir Immune Defic Syndr. 2013;64(4):417–23.
Chakravarty D, Hoff CC, Neilands TB, Darbes LA. Rates of testing for HIV in the presence of serodiscordant UAI among HIV-negative gay men in committed relationships. AIDS Behav. 2012;16(7):1944–8.
Mitchell JW, Petroll AE. Patterns of HIV and sexually transmitted infection testing among men who have sex with men couples in the United States. Sex Transm Dis. 2012;39(11):871–6.
Mitchell JW, Petroll AE. HIV testing rates and factors associated with recent HIV testing among male couples. Sex Transm Dis. 2012;39(5):379–81.
Stephenson R, White D, Darbes L, Hoff C, Sullivan P. HIV testing behaviors and perceptions of risk of HIV infection among MSM with main partners. AIDS Behav. 2015;19(3):553–60.
Prevention CfDCa. NCHHSTP AtlasPlus [online data portal] 2019. Available from: https://www.cdc.gov/nchhstp/atlas/index.htm.
Starks TJ, Doyle KM, Shalhav O, John SA, Parsons JT. An examination of gay couples’ motivations to use (or forego) pre-exposure prophylaxis expressed during couples HIV testing and counseling (CHTC) sessions. Prev Sci. 2019;20(1):157–67.
Saberi P, Gamarel KE, Neilands TB, Comfort M, Sheon N, Darbes LA, et al. Ambiguity, ambivalence, and apprehensions of taking HIV-1 pre-exposure prophylaxis among male couples in San Francisco: a mixed methods study. PLoS One. 2012;7(11):e50061.
Bavinton BR, Prestage GP, Jin F, Phanuphak N, Grinsztejn B, Fairley CK, et al. Strategies used by gay male HIV serodiscordant couples to reduce the risk of HIV transmission from anal intercourse in three countries. J Int AIDS Soc. 2019;22(4):e25277.
Wall KM, Canary L, Workowski K, Lockard A, Jones J, Sullivan P, et al. Acceptability of couples’ voluntary HIV testing among HIV-infected patients in care and their HIV-negative partners in the United States. Open AIDS J. 2016;10(1):1–13.
Hoff CC, Chakravarty D, Bircher AE, Campbell CK, Grisham K, Neilands TB, et al. Attitudes towards PrEP and anticipated condom use among concordant HIV-negative and HIV-discordant male couples. AIDS Patient Care STDS. 2015;29(7):408–17.
Mitchell JW, Lee J-Y, Woodyatt C, Bauermeister J, Sullivan P, Stephenson R. HIV-negative male couples’ attitudes about pre-exposure prophylaxis (PrEP) and using PrEP with a sexual agreement. AIDS Care. 2016;28(8):994–9.
Brooks RA, Kaplan RL, Lieber E, Landovitz RJ, Lee S-J, Leibowitz AA. Motivators, concerns, and barriers to adoption of preexposure prophylaxis for HIV prevention among gay and bisexual men in HIV-serodiscordant male relationships. AIDS Care. 2011;23(9):1136–45.
Bosco SC, Pawson M, Parsons JT, Starks TJ. Biomedical HIV prevention among gay male couples: a qualitative study of motivations and concerns. J Homosex. 2019:1–18.
Sarno EL, Bettin E, Jozsa K, Newcomb ME. Sexual health of rural and urban young male couples in the United States: differences in HIV testing, pre-exposure prophylaxis use, and condom use. AIDS Behav. 2020;25:191–202.
John SA, Robles G, Starks TJ, Jonathon RH. Differences between groups of pre-exposure prophylaxis (PrEP) using couples in HIV-negative/unknown relationships. JAIDS J Acquir Immune Defic Syndr. 2019;81(4):419–28.
Mimiaga MJ, Closson EF, Kothary V, Mitty JA. Sexual partnerships and considerations for HIV antiretroviral pre-exposure prophylaxis utilization among high-risk substance using men who have sex with men. Arch Sex Behav. 2014;43(1):99–106.
Körner H, Hendry O, Kippax S. Negotiating risk and social relations in the context of post-exposure prophylaxis for HIV: narratives of gay men. Health Risk Soc. 2005;7(4):349–60.
Mitchell JW, Stephenson R. HIV-negative partnered men’s willingness to use pre-exposure prophylaxis and associated factors among an internet sample of U.S. HIV-negative and HIV-discordant male couples. LGBT Health. 2015;2(1):35–40.
Kahle EM, Sharma A, Sullivan S, Stephenson R. The influence of relationship dynamics and sexual agreements on perceived partner support and benefit of PrEP use among same-sex male couples in the U.S. AIDS Behav. 2020;24(7):2169–77.
Stephenson R, Chavanduka TMD, Sullivan S, Mitchell JW. Correlates of successful enrollment of same-sex male couples into a web-based HIV prevention research study: cross-sectional study. JMIR Public Health Surveill. 2020;6(1):e15078.
Mitchell JW, Chavanduka TMD, Sullivan S, Stephenson R. Recommendations from a descriptive evaluation to improve screening procedures for web-based studies with couples: cross-sectional study. JMIR Public Health Surveill. 2020;6(2):e15079.
Cuervo M, Whyte J. The effect of relationship characteristics on HIV risk behaviors and prevention strategies in young gay and bisexual men. J Assoc Nurses Aids Care. 2015;26(4):399–410.
Larzelere RE, Huston TL. The dyadic trust scale: toward understanding interpersonal trust in close relationships. J Marriage Fam. 1980;42:595–604.
Christensen A. Detection of conflict patterns in couples. In: Hahlweg K, Goldstein MJ, editors. Understanding major mental disorder: The contribution of family interaction research. Family Process Press; 1987. p. 250–265.
Christensen A. Dysfunctional interaction patterns in couples. In: Noller P, Fitzpatrick MA, editors. Perspectives on marital interaction. Multilingual Matters; 1988. p. 31–52.
Christensen A, Sullaway M. Communication patterns questionnaire. Unpublished manuscript, University of California, Los Angeles. 1984.
Salazar LF, Stephenson RB, Sullivan PS, Tarver R. Development and validation of HIV-related dyadic measures for men who have sex with men. J Sex Res. 2013;50(2):164–77.
Carey MP, Schroder KE. Development and psychometric evaluation of the brief HIV Knowledge Questionnaire. AIDS Educ Prev. 2002;14(2):172–82.
Napper LE, Fisher DG, Reynolds GL. Development of the perceived risk of HIV scale. AIDS Behav. 2012;16(4):1075–83.
Szymanski DM. Does internalized heterosexism moderate the link between heterosexist events and lesbians’ psychological distress? Sex Roles. 2006;54(3–4):227–34.
Smolenski DJ, Diamond PM, Ross MW, Simon Rosser BR. Revision, criterion validity, and multigroup assessment of the reactions to homosexuality scale. J Pers Assess. 2010;92(6):568–76.
Fortenberry JD, McFarlane M, Bleakley A, Bull S, Fishbein M, Grimley DM, et al. Relationships of stigma and shame to gonorrhea and HIV screening. Am J Public Health. 2002;92(3):378–81.
Bush K, Kivlahan DR, McDonell MB, Fihn SD, Bradley KA. The AUDIT alcohol consumption questions (AUDIT-C): an effective brief screening test for problem drinking. Ambulatory Care Quality Improvement Project (ACQUIP). Alcohol Use Disorders Identification Test. Arch Intern Med. 1998;158(16):1789–95.
Organization WH. AUDIT: the alcohol use disorders identification test: guidelines for use in primary health care. Geneva: World Health Organization; 2001.
Saunders JB, Aasland OG, Babor TF, de la Fuente JR, Grant M. Development of the alcohol use disorders identification test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption-II. Addiction. 1993;88(6):791–804.
Carpenter J, Andrykowski M, Wilson J, Hall L, Rayens MK, Sachs B, et al. Psychometrics for two short forms of the Center for Epidemiologic Studies-Depression Scale. Issues Ment Health Nurs. 1998;19(5):481–94.
Cook WL, Kenny DA. The actor–partner interdependence model: a model of bidirectional effects in developmental studies. Int J Behav Dev. 2005;29(2):101–9.
Kenny DA, Kashy DA, Cook WL. Dyadic data analysis. New York: Guilford Press; 2006.
Serota DP, Rosenberg ES, Lockard AM, Rolle C-PM, Luisi N, Cutro S, et al. Beyond the biomedical: preexposure prophylaxis failures in a cohort of young Black men who have sex with men in Atlanta, Georgia. Clin Infect Dis. 2018;67(6):965–70.
Siegler AJ, Bratcher A, Weiss KM. Geographic access to preexposure prophylaxis clinics among men who have sex with men in the United States. Am J Public Health. 2019;109(9):1216–23.
Edelman EJ, Jennifer Edelman E, Moore BA, Calabrese SK, Berkenblit G, Cunningham C, et al. Primary care physicians’ willingness to prescribe HIV pre-exposure prophylaxis for people who inject drugs. AIDS Behav. 2017;21(4):1025–33.
Galindo GR, JnJ Walker, Hazelton P, Lane T, Steward WT, Morin SF, et al. Community member perspectives from transgender women and men who have sex with men on pre-exposure prophylaxis as an HIV prevention strategy: implications for implementation. Implement Sci. 2012;7(1):1–13.
Eaton LA, Driffin DD, Bauermeister J, Smith H, Conway-Washington C. Minimal awareness and stalled uptake of pre-exposure prophylaxis (PrEP) among at risk, HIV-negative, Black men who have sex with men. AIDS Patient Care STDS. 2015;29(8):423–9.
Cohen SE, Vittinghoff E, Bacon O, Doblecki-Lewis S, Postle BS, Feaster DJ, et al. High interest in preexposure prophylaxis among men who have sex with men at risk for HIV infection: baseline data from the US PrEP demonstration project. J Acquir Immune Defic Syndr. 2015;68(4):439–48.
Highleyman L. HIV AIDs information: PrEP use is rising fast in US but large racial disparities remain 2016. Available from: http://www.aidsmap.com/PrEP-use-is-rising-fast-in-US-but-large-racial-disparities-remain/page/3065545/.
Sullivan S, Stephenson R. Perceived HIV prevalence accuracy and sexual risk behavior among gay, bisexual, and other men who have sex with men in the United States. AIDS Behav. 2018;22(6):1849–57.
Eaton LA, Kalichman SC, Price D, Finneran S, Allen A, Maksut J. Stigma and conspiracy beliefs related to pre-exposure prophylaxis (PrEP) and interest in using PrEP among Black and White men and transgender women who have sex with men. AIDS Behav. 2017;21(5):1236–46.
Mustanski B, Ryan DT, Hayford C, Phillips G, Newcomb ME, Smith JD. Geographic and individual associations with PrEP stigma: results from the RADAR cohort of diverse young men who have sex with men and transgender women. AIDS Behav. 2018;22(9):3044–56.
Corrigan PW, Druss BG, Perlick DA. The impact of mental illness stigma on seeking and participating in mental health care. Psychol Sci Public Interest. 2014;15(2):37–70.
Whitehead J, Shaver J, Stephenson R. Outness, stigma, and primary health care utilization among rural LGBT populations. PLOS One. 2016;11(1):e0146139.
Marcus JL, Glidden DV, Mayer KH, Liu AY, Buchbinder SP, Rivet Amico K, et al. No evidence of sexual risk compensation in the iPrEx trial of daily oral HIV preexposure prophylaxis. PLoS One. 2013;8(12):e81997.
Prevention CfDCa. Preexposure prophylaxis for the prevention of HIV infection in the United States—2017 update: a clinical practice guideline. US Public Health Service; 2018.
Hoff CC, Beougher SC, Chakravarty D, Darbes LA, Neilands TB. Relationship characteristics and motivations behind agreements among gay male couples: differences by agreement type and couple serostatus. AIDS Care. 2010;22(7):827–35.
Hernandez-Romieu AC, Sullivan PS, Sanchez TH, Kelley CF, Peterson JL, Del Rio C, et al. The comparability of men who have sex with men recruited from venue-time-space sampling and facebook: a cohort study. JMIR Res Protoc. 2014;3(3):e37.
Martinez O, Wu E, Levine EC, Muñoz-Laboy M, Isabel Fernandez M, Bass SB, et al. Integration of social, cultural, and biomedical strategies into an existing couple-based behavioral HIV/STI prevention intervention: voices of Latino male couples. PLOS One. 2016;11(3):e0152361.
Burton J, Darbes LA, Operario D. Couples-focused behavioral interventions for prevention of HIV: systematic review of the state of evidence. AIDS Behav. 2010;14(1):1–10.
Martinez O, Wu E, Frasca T, Shultz AZ, Fernandez MI, López Rios J, et al. Adaptation of a couple-based HIV/STI prevention intervention for Latino men who have sex with men in New York City. Am J Mens Health. 2017;11(2):181–95.
Stephenson R, Freeland R, Sullivan SP, Riley E, Johnson BA, Mitchell J, et al. Home-based HIV testing and counseling for male couples (Project Nexus): a protocol for a randomized controlled trial. JMIR Res Protoc. 2017;6(5):e101.
Bazzi AR, Fergus KB, Stephenson R, Finneran CA, Coffey-Esquivel J, Hidalgo MA, et al. A dyadic behavioral intervention to optimize same sex male couples’ engagement across the HIV care continuum: development of and protocol for an innovative couples-based approach (partner steps). JMIR Res Protoc. 2016;5(3):e168.
Newcomb ME, Macapagal KR, Feinstein BA, Bettin E, Swann G, Whitton SW. Integrating HIV prevention and relationship education for young same-sex male couples: a pilot trial of the 2GETHER intervention. AIDS Behav. 2017;21(8):2464–78.
Mitchell JW, Lee J, Wu Y, Sullivan PS, Stephenson R. Feasibility and acceptability of an electronic health HIV prevention toolkit intervention with concordant HIV-negative, same-sex male couples on sexual agreement outcomes: pilot, randomized controlled trial. JMIR Form Res. 2020;4(2):e16807.
Funding
Funding was provided by National Institute for Mental Health (Grant No. R21MH111445).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
All procedures involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The study protocol was approved by the University of Michigan Institutional Review Board (HUM00125711).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Stephenson, R., Chavanduka, T.M.D., Sullivan, S.P. et al. Dyadic Influences on Pre-exposure Prophylaxis (PrEP) Use and Attitudes Among Male Couples. AIDS Behav 26, 361–374 (2022). https://doi.org/10.1007/s10461-021-03389-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-021-03389-4