Abstract
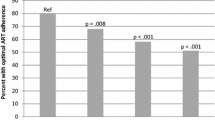
Alcohol use remains prevalent among Russian women with HIV infection. Multilevel mixed effects models were used to estimate the association of heavy drinking and HIV outcomes among women (N = 250 at baseline; N = 207 at follow-up), aged 18–35, engaged in HIV care in Saint Petersburg. Alcohol use was assessed at baseline and 3 months by self-report and by the biomarker phosphatidylethanol (PEth). Overall, 35% of women were heavy drinkers, defined as women reporting ≥ 1 past-30-day heavy drinking episode (≥ 4 standard drinks on one occasion) or with PEth blood levels ≥ 80 ng/mL. Women who engaged in heavy drinking had an average 41 CD4 cells/mm3 (95% CI = − 81, − 2; z = − 2.04; P = 0.042) fewer than those who did not. Heavy drinking was associated with higher HIV symptom burden (IRR = 1.20; 95% CI = 1.05, 1.36; z = 2.73; P = 0.006) and suboptimal antiretroviral adherence (OR = 3.04; 95% CI = 1.27, 7.28; χ2 = 2.50; P = 0.013), but not with viral load. Findings support the integration of alcohol treatment interventions as part of routine HIV care in Russia.
Resumen
El consumo de alcohol es común en las mujeres rusas con VIH. Utilizamos modelos multinivel de efectos mixtos para estimar la asociación entre el consumo de alcohol excesivo y los resultados adversos de VIH en un grupo de mujeres (N = 250 al inicio del estudio; N = 207 en el seguimiento), de 18 a 35 años de edad, que recibían atención médica para el VIH en San Petersburgo. El consumo de alcohol excesivo, definido como el consumo de ≥ 4 bebidas alcohólicas en una ocasión en base a autoinforme o a niveles de fosfatidiletanol ≥ 80 ng/mL, se evaluó al inicio del estudio y a los 3 meses. Las mujeres que bebían en exceso, el 35% de la muestra, tenían un promedio de 41 células CD4/mm3 (IC del 95% = − 81, − 2; z = − 2,04; P = 0,042) menos que las que no lo hacían. El consumo excesivo de alcohol se asoció con una mayor carga de síntomas de VIH (TIR = 1,20; IC del 95% = 1,05, 1,36; z = 2,73; P = 0,006) y una adherencia al tratamiento antirretroviral subóptima (OR = 3,04; IC del 95% = 1,27, 7,28; χ2 = 2,50; P = 0,013), pero no con carga viral. Los hallazgos respaldan la integración de la atención para el tratamiento del alcoholismo en los servicios de atención rutinaria del VIH en Rusia.
Similar content being viewed by others
Data Availability
The data used for this analysis is available upon request from the corresponding author.
References
UNAIDS. Country: Russian Federation. https://www.unaids.org/en/regionscountries/countries/russianfederation. Published 2019. Accessed 29 Sep 2019
Beyrer C, Wirtz AL, O’Hara G, Léon N, Kazatchkine M. The expanding epidemic of HIV-1 in the Russian federation. PLoS Med. 2017;14(11):e1002462–e1002462.
Federal Scientific Center for the Prevention and Control of AIDS of the Public Office of the Central Scientific Research Institute Rospotrebnadzor. HIV-infection Bulletin No. 44. Moscow: Rospotrebnadzor, 2019.
World Health Organization. Alcohol policy impact case study. The effects of alcohol control measures on mortality and life expectancy in the Russian Federation. Copenhagen: WHO Regional Office for Europe; 2019. Available on https://apps.who.int/iris/handle/10665/328167. Accessed 20 July 2020
Lan CW, Scott-Sheldon LA, Carey KB, Johnson BT, Carey MP. Prevalence of alcohol use, sexual risk behavior, and HIV among Russians in high-risk settings: a systematic review and meta-analysis. Int J Behav Med. 2017;24(2):180–90.
Abdala N, Grau LE, Zhan W, et al. Inebriation, drinking motivations and sexual risk taking among sexually transmitted disease clinic patients in St Petersburg, Russia. AIDS Behav. 2013;17(3):1144–50.
World Health Organization. Global status report on alcohol and health 2018. Geneva: World Health Organization; 2018.
Williams EC, Hahn JA, Saitz R, Bryant K, Lira MC, Samet JH. Alcohol use and human immunodeficiency virus (HIV) infection: current knowledge, implications, and future directions. Alcohol Clin Exp Res. 2016;40(10):2056–72.
Kahler CW, Liu T, Cioe PA, et al. Direct and indirect effects of heavy alcohol use on clinical outcomes in a longitudinal study of HIV patients on ART. AIDS Behav. 2017;21(7):1825–35.
Williams EC, McGinnis KA, Edelman EJ, et al. Level of alcohol use associated with HIV care continuum targets in a national U.S. sample of persons living with HIV receiving healthcare. AIDS Behav. 2019;23(1):140–51.
Deiss RG, Mesner O, Agan BK, et al. Characterizing the association between alcohol and HIV virologic failure in a military cohort on antiretroviral therapy. Alcohol Clin Exp Res. 2016;40(3):529–35.
Hahn JA, Cheng DM, Emenyonu NI, et al. Alcohol use and HIV disease progression in an antiretroviral naive cohort. J Acquir Immune Defic Syndr. 2018;77(5):492–501.
Wandera B, Tumwesigye NM, Nankabirwa JI, et al. Hazardous alcohol consumption is not associated with CD4+ T-cell count decline among PLHIV in Kampala Uganda: a prospective cohort study. PLoS ONE. 2017;12(6):e0180015.
Cagle A, McGrath C, Richardson BA, et al. Alcohol use and immune reconstitution among HIV-infected patients on antiretroviral therapy in Nairobi, Kenya. AIDS Care. 2017;29(9):1192–7.
Carrieri MP, Protopopescu C, Raffi F, et al. Low alcohol consumption as a predictor of higher CD4+ cell count in HIV-treated patients: a French paradox or a proxy of healthy behaviors? The ANRS APROCO-COPILOTE CO-08 cohort. J Acquir Immune Defic Syndr. 2014;65(4):e148-150.
Barve SS, Kelkar SV, Gobejishvilli L, Joshi-Barve S, McClain CJ. Mechanisms of alcohol-mediated CD4+ T lymphocyte death: relevance to HIV and HCV pathogenesis. Front Biosci. 2002;7:d1689-1696.
So-Armah KA, Cheng DM, Freiberg MS, et al. Association between alcohol use and inflammatory biomarkers over time among younger adults with HIV-The Russia ARCH observational study. PLoS ONE. 2019;14(8):e0219710.
Fuster D, Sanvisens A, Bolao F, Rivas I, Tor J, Muga R. Alcohol use disorder and its impact on chronic hepatitis C virus and human immunodeficiency virus infections. World J Hepatol. 2016;8(31):1295–308.
Barve S, Kapoor R, Moghe A. Focus on the liver: alcohol use, highly active antiretroviral therapy, and liver disease in HIV-infected patients. Alcohol Res Health. 2010;33(3):229–36.
Bagby GJ, Amedee AM, Siggins RW, Molina PE, Nelson S, Veazey RS. Alcohol and HIV effects on the immune system. Alcohol Res. 2015;37(2):287–97.
Neblett RC, Hutton HE, Lau B, McCaul ME, Moore RD, Chander G. Alcohol consumption among HIV-infected women: impact on time to antiretroviral therapy and survival. J Womens Health (Larchmt). 2011;20(2):279–86.
Heimer R, Usacheva N, Barbour R, Niccolai LM, Uusküla A, Levina OS. Engagement in HIV care and its correlates among people who inject drugs in St Petersburg, Russian Federation and Kohtla-Järve, Estonia. Addiction. 2017;112(8):1421–31.
Vagenas P, Azar MM, Copenhaver MM, Springer SA, Molina PE, Altice FL. The impact of alcohol use and related disorders on the HIV continuum of care: a systematic review. Curr HIV/AIDS Rep. 2015;12(4):421–36.
Amirkhanian YA, Kelly JA, DiFranceisco WJ, et al. Predictors of HIV care engagement, antiretroviral medication adherence, and viral suppression among people living with HIV infection in St. Petersburg, Russia. AIDS Behav. 2018;22(3):791–9.
Kalichman SC, Grebler T, Amaral CM, et al. Intentional non-adherence to medications among HIV positive alcohol drinkers: prospective study of interactive toxicity beliefs. J Gen Intern Med. 2013;28(3):399–405.
Kahler C, Liu T, Cioe P, et al. Direct and indirect effects of heavy alcohol use on clinical outcomes in a longitudinal study of HIV patients on ART. AIDS Behav. 2017;21:1825–35.
Littlefield AK, Brown JL, DiClemente RJ, et al. Phosphatidylethanol (PEth) as a biomarker of alcohol consumption in HIV-infected young Russian women: comparison to self-report assessments of alcohol use. AIDS Behav. 2017;21(7):1938–49.
Hahn JA, Dobkin LM, Mayanja B, et al. Phosphatidylethanol (PEth) as a biomarker of alcohol consumption in HIV-positive patients in sub-Saharan Africa. Alcohol Clin Exp Res. 2012;36(5):854–62.
Matson TE, McGinnis KA, Rubinsky AD, et al. Gender and alcohol use: influences on HIV care continuum in a national cohort of patients with HIV. AIDS. 2018;32(15):2247–53.
Ohashi K, Pimienta M, Seki E. Alcoholic liver disease: a current molecular and clinical perspective. Liver Res. 2018;2(4):161–72.
Brown JL, DiClemente RJ, Sales JM, et al. Substance use patterns of HIV-infected Russian women with and without hepatitis C virus Co-infection. AIDS Behav. 2016;20(10):2398–407.
Jones J, Jones M, Plate C, Lewis D. The detection of 1-palmitoyl-2-oleoyl-sn-glycero-3-phosphoethanol in human dried blood spots. Anal Methods. 2011;3:1101–6.
Hahn JA, Anton RF, Javors MA. The formation, elimination, interpretation, and future research needs of phosphatidylethanol for research studies and clinical practice. Alcohol Clin Exp Res. 2016;40(11):2292–5.
Carey KB. Understanding binge drinking: introduction to the special issue. Psychol Addict Behav. 2001;15(4):283–6.
Stewart SH, Koch DG, Willner IR, Anton RF, Reuben A. Validation of blood phosphatidylethanol as an alcohol consumption biomarker in patients with chronic liver disease. Alcohol Clin Exp Res. 2014;38(6):1706–11.
Molina PE, Nelson S. Binge drinking’s effects on the body. Alcohol Res Curr Rev. 2018;39(1):99–109.
Yu T, Wu L. Robust modelling of the relationship between CD4 and viral load for complex AIDS data. J Appl Stat. 2017;45(2):367–83.
Elul B, Basinga P, Nuwagaba-Biribonwoha H, et al. High levels of adherence and viral suppression in a nationally representative sample of HIV-infected adults on antiretroviral therapy for 6, 12 and 18 months in Rwanda. PLoS ONE. 2013;8(1):e53586.
Justice AC, Holmes W, Gifford AL, et al. Development and validation of a self-completed HIV symptom index. J Clin Epidemiol. 2001;54(12):S77–90.
Ickovics JR, Meade CS. Adherence to HAART among patients with HIV: breakthroughs and barriers. AIDS Care. 2002;14(3):309–18.
Simoni JM, Kurth AE, Pearson CR, Pantalone DW, Merrill JO, Frick PA. Self-report measures of antiretroviral therapy adherence: a review with recommendations for HIV research and clinical management. AIDS Behav. 2006;10(3):227–45.
Turner BJ. Adherence to antiretroviral therapy by human immunodeficiency virus—infected patients. J Infect Dis. 2002;185(Supplement_2):S143–51.
Bartlett JA. Addressing the challenges of adherence. JAIDS. 2002;29:S2–10.
Viswanathan S, Detels R, Mehta SH, Macatangay BJC, Kirk GD, Jacobson LP. Level of adherence and HIV RNA suppression in the current era of highly active antiretroviral therapy (HAART). AIDS Behav. 2015;19(4):601–11.
Bezabhe WM, Chalmers L, Bereznicki LR, Peterson GM. Adherence to antiretroviral therapy and virologic failure: a meta-analysis. Medicine. 2016;95(15):e3361–e3361.
MacKinnon DP. Introduction to statistical mediation analysis. New York: Erlbaum; 2008.
Preacher KJ. Advances in mediation analysis: a survey and synthesis of new developments. Annu Rev Psychol. 2015;66:825–52.
Amirkhanian YA, Kelly JA, Kuznetsova AV, DiFranceisco WJ, Musatov VB, Pirogov DG. People with HIV in HAART-Era Russia: transmission risk behavior prevalence, antiretroviral medication-taking, and psychosocial distress. AIDS Behav. 2011;15(4):767–77.
Puryear SB, Balzer LB, Ayieko J, et al. Associations between alcohol use and HIV care cascade outcomes among adults undergoing population-based HIV testing in East Africa. AIDS. 2020;34(3):405–13.
Kowalski S, Colantuoni E, Lau B, et al. Alcohol consumption and CD4 T-cell count response among persons initiating antiretroviral therapy. J Acquir Immune Defic Syndr. 2012;61(4):455–61.
Hahn JA, Samet JH. Alcohol and HIV disease progression: weighing the evidence. Curr HIV/AIDS Rep. 2010;7(4):226–33.
Baum MK, Rafie C, Lai S, Sales S, Page JB, Campa A. Alcohol use accelerates HIV disease progression. AIDS Res Hum Retroviruses. 2010;26(5):511–8.
Bilal U, Lau B, Lazo M, et al. Interaction between alcohol consumption patterns, antiretroviral therapy type, and liver fibrosis in persons living with HIV. AIDS Patient Care STDS. 2016;30:200–7.
Pecoraro A, Mimiaga MJ, O’Cleirigh C, et al. Lost-to-care and engaged-in-care HIV patients in Leningrad Oblast, Russian Federation: barriers and facilitators to medical visit retention. AIDS Care. 2014;26(10):1249–57.
Garey L, Bakhshaie J, Sharp C, Neighbors C, Zvolensky MJ, Gonzalez A. Anxiety, depression, and HIV symptoms among persons living with HIV/AIDS: the role of hazardous drinking. AIDS Care. 2015;27(1):80–5.
Kumar S, Jin M, Ande A, Sinha N, Silverstein PS, Kumar A. Alcohol consumption effect on antiretroviral therapy and HIV-1 pathogenesis: role of cytochrome P450 isozymes. Expert Opin Drug Metab Toxicol. 2012;8(11):1363–75.
Azar MM, Springer SA, Meyer JP, Altice FL. A systematic review of the impact of alcohol use disorders on HIV treatment outcomes, adherence to antiretroviral therapy and health care utilization. Drug Alcohol Depend. 2010;112(3):178–93.
O’Connor J, Smith C, Lampe FC, et al. Durability of viral suppression with first-line antiretroviral therapy in patients with HIV in the UK: an observational cohort study. Lancet HIV. 2017;4(7):e295–302.
Phillips AN, Staszewski S, Weber R, et al. HIV viral load response to antiretroviral therapy according to the baseline CD4 cell count and viral load. JAMA. 2001;286(20):2560–7.
Heimer R, Usacheva N, Barbour R, Niccolai LM, Uuskula A, Levina OS. Engagement in HIV care and its correlates among people who inject drugs in St Petersburg, Russian Federation and Kohtla-Jarve, Estonia. Addiction. 2017;112(8):1421–31.
Papas RK, Gakinya BN, Mwaniki MM, et al. Associations between the phosphatidylethanol alcohol biomarker and self-reported alcohol use in a sample of HIV-infected outpatient drinkers in Western Kenya. Alcohol Clin Exp Res. 2016;40(8):1779–87.
Funding
This work was supported by grants from the National Institute on Drug Abuse (JLB: R03DA0377860; RJD: 1U01DA0362233) and the National Institute on Alcohol Abuse and Alcoholism (RJD: 1R01AA018096). The funding source had no role in the study design; data collection, analysis, or interpretation; writing or decision to submit the paper for publication. No financial disclosures that pose a conflict of interest are reported by the authors of this paper.
Author information
Authors and Affiliations
Contributions
AC: Conception and design of the analysis; statistical analysis, interpretation and writing; JLB: Critical revision of the work; PS: Data collection, coordination, critical revision of the work; NB and VR: Project conception, data collection quality control, critical revision of the work; RJD: Conception of the project, data collection quality control, revision of the data, findings and writing, final approval of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to disclose.
Ethical Approval
The Institutional Review Boards of Emory University (USA) and St. Petersburg AIDS Center (Russia) approved all study procedures.
Consent to Participate
All participants provided signed informed consent prior to recruitment.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Capasso, A., Brown, J.L., Safonova, P. et al. Heavy Alcohol Use is Associated with Lower CD4 Counts among Russian Women Living with HIV: A Multilevel Analysis. AIDS Behav 25, 3734–3742 (2021). https://doi.org/10.1007/s10461-021-03270-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-021-03270-4