Abstract
A key strategy of the South African national response to HIV is the scale-up of HIV counselling and testing (HCT) in the 15–49 years age group. The integrated school health policy aims to guide the roll out of youth-friendly health services including the provision of HCT in schools. Using a discrete choice experiment to examine preferences regarding the attributes of HCT service packages, this study identifies barriers to and facilitators of HCT among high school learners. Monetary considerations were found to have the strongest effect of any attribute on choice, whilst confidentiality was found to be a primary concern for learners considering HCT. Policy makers and service providers must ensure that confidentiality is maintained, and could consider using monetary incentives as a way of increasing uptake of HCT. Programmes designed to reduce social stigma and improve education and knowledge dissemination around HCT and HIV, are vital in creating demand for HCT and changing attitudes among young people.
Similar content being viewed by others
References
Shisana O, Rehle T, Simbayi L, Zuma K, Jooste S, Zungu N, et al. South African national HIV prevalence, incidence and behaviour survey, 2012. Cape Town: Human Sciences Research Council HSRC; 2014.
Schwartländer B, Stover J, Hallett T, Atun R, Avila C, Gouws E, et al. Towards an improved investment approach for an effective response to HIV/AIDS. Lancet. 2011;377:2031–41.
National Department of Health South Africa. National Department of Health Annual performance plan 2014/15–2016/17. Pretoria: National Department of Health South Africa; 2014.
World Health Organization. HIV/AIDS statement on HIV testing and counseling: WHO, UNAIDS re-affirm opposition to mandatory HIV testing. HIV. Geneva; 2012. www.who.int/hiv/events/2012/world_aids_day/hiv_testing_counselling/en/index.html.
UNAIDS. Fast-track ending the AIDS epidemic by 2030. Geneva: Joint United Nations Programme on HIV and AIDS; 2014.
National Department of Health, National Department Of Education. Integrated school health policy. Pretoria: Government Printer; 2012.
Bearinger LH, Sieving RE, Ferguson J, Sharma V. Global perspectives on the sexual and reproductive health of adolescents: patterns, prevention, and potential. Lancet. 2007;369(9568):1220–31.
MacPhail CL, Pettifor A, Coates T, Rees H. “You must do the test to know your status”: attitudes to HIV voluntary counseling and testing for adolescents among South African youth and parents. Health Educ Behav. 2008;35(1):87–104.
Young SD, Hlavka Z, Modiba P, Gray G, Van Rooyen H, Richter L, et al. HIV-related stigma, social norms, and HIV testing in Soweto and Vulindlela, South Africa: National Institutes of Mental Health Project Accept (HPTN 043). J Acquir Immune Defic Syndr. 2010;55(5):620–4.
National Department of Health. The 2011 national antenatal sentinel HIV & syphilis prevalence survey in South Africa. Pretoria: Department of Health; 2012.
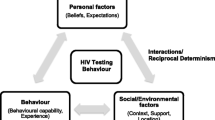
Glanz K, Rimer BK, Su SM. Theory at a glance: a guide for health promotion practice. Bethesda: United States National Cancer Institute; 2005.
Lancaster KJ. A new approach to consumer theory. J Polit Econ. 1966;74(2):132.
Louviere J, Hensher D, Swait J. Stated choice methods: analysis and applications. Cambridge: Cambridge University Press; 2000.
Njagi F, Maharaj P. Access to voluntary counselling and testing services: perspectives of young people. S Afr Rev Sociol. 2006;37(2):113–27. doi:10.1080/21528586.2006.10419150.
Mathews C, Guttmacher SJ, Flisher AJ, Mtshizana YY, Nelson T, McCarthy J, et al. The quality of HIV testing services for adolescents in Cape Town, South Africa: do adolescent-friendly services make a difference? J Adolesc Health. 2009;44(2):188–90.
Erulkar AS, Onoka CJ, Phiri A. What is youth-friendly? Adolescents’ preferences for reproductive health services in Kenya and Zimbabwe. Afr J Reprod Health. 2005;9(3):51–8.
Agot K, Onyango J. Youth-friendly services for HIV prevention, treatment, and care: the Tuungane Youth Project, Kenya. In: Marlink R, Teitelman S, editors. From the ground up: building comprehensive HIV/AIDS care programs in resource-limited settings. Washington: Elizabeth Glaser Pediatric AIDS Foundation Publication; 2004. p. 37–41.
Ikechebelu IJ, Udigwe GO, Ikechebelu N, Imoh LC. The knowledge, attitude and practice of voluntary counselling and testing (VCT) for HIV/AIDS among undergraduates in a polytechnic in southeast, Nigeria. Niger J Med. 2006;15(3):245–9.
MacPhail C, Pettifor A, Moyo W, Rees H. Factors associated with HIV testing among sexually active South African youth aged 15–24 years. AIDS Care. 2009;21(4):456–67.
Fako TT. Social and psychological factors associated with willingness to test for HIV infection among young people in Botswana. AIDS Care. 2006;18(3):201–7.
Kabiru CW, Beguy D, Crichton J, Zulu EM. HIV/AIDS among youth in urban informal (slum) settlements in Kenya: what are the correlates of and motivations for HIV testing? BMC Public Health. 2011;11:685.
Lancsar E, Louviere J. Conducting discrete choice experiments to inform healthcare decision making. Pharmacoeconomics. 2008;26(8):661–77.
Viney R, Lancsar E, Louviere J. Discrete choice experiments to measure consumer preferences for health and healthcare. Expert Rev Pharmacoecon Outcomes Res. 2002;2(4):319–26. doi:10.1586/14737167.2.4.319.
de Bekker-Grob EW, Ryan M, Gerard K. Discrete choice experiments in health economics: a review of the literature. Health Econ. 2012;21(2):145–72.
Hoeffler S, Ariely D. Constructing stable preferences: a look into dimensions of experience and their impact on preference stability. J Consum Psychol. 1999;8(2):113–39.
Strauss M, Rhodes B, George G. A qualitative analysis of the barriers and facilitators of HIV counselling and testing perceived by adolescents in South Africa. BMC Health Serv Res. 2015;15(1):250.
South African Reserve Bank. Selected historical rates. 2016. http://www.resbank.co.za/Research/Rates/Pages/SelectedHistoricalExchangeAndInterestRates.aspx.
Zwerina K, Huber J, Kuhfeld W. A general method for constructing efficient choice designs. Durham: Duke University; 1996. p. 39–59.
Street DJ, Burgess L, Louviere JJ. Quick and easy choice sets: constructing optimal and nearly optimal stated choice experiments. Int J Res Mark. 2005;22(4):459–70.
Montague C, Ngcobo N, Mahlase G, Frohlich J, Pillay C, Yende-Zuma N, et al. Implementation of adolescent-friendly voluntary medical male circumcision using a school based recruitment program in rural KwaZulu-Natal, South Africa. PLoS ONE. 2014;9(5):e96468.
Hensher D, Rose J, Greene W. Applied choice analysis: a primer. Cambridge: Cambridge University Press; 2005.
Ryan M, Gerard K. Using discrete choice experiments to value health care programmes: current practice and future research reflections. Appl Health Econ Health Policy. 2003;2(1):55–64.
Haan P. Discrete choice labor supply: conditional logit vs. random coefficient models. Berlin: German Institute for Economic Research; 2004.
Clark MD, Determann D, Petrou S, Moro D, de Bekker-Grob EW. Discrete choice experiments in health economics: a review of the literature. Pharmacoeconomics. 2014;32(9):883–902.
Ramirez-Avila L, Nixon K, Noubary F, Giddy J, Losina E, Walensky RP, et al. Routine HIV testing in adolescents and young adults presenting to an outpatient clinic in Durban, South Africa. PLoS ONE. 2012;7(9):e45507.
South African National AIDS Council. Global AIDS response progress report 2012: Republic of South Africa. 2012.http://www.unaids.org/en/dataanalysis/knowyourresponse/countryprogressreports/2012countries/ce_ZA_Narrative_Report.pdf.
Walensky RP, Wood R, Fofana MO, Martinson NA, Losina E, April MD, et al. The clinical impact and cost-effectiveness of routine, voluntary HIV screening in South Africa. J Acquir Immune Defic Syndr. 2011;56(1):26–35.
Rosenberg NE, Westreich D, Bärnighausen T, Miller WC, Behets F, Maman S, et al. Assessing the effect of HIV counselling and testing on HIV acquisition among South African youth. AIDS. 2013;27(17):2765–73.
Padian NS, Buvé A, Balkus J, Serwadda D, Cates W. Biomedical interventions to prevent HIV infection: evidence, challenges, and way forward. Lancet. 2008;372(9638):585–99.
Kharsany ABM, Mlotshwa M, Frohlich JA, Yende Zuma N, Samsunder N, Abdool Karim SS, et al. HIV prevalence among high school learners—opportunities for schools-based HIV testing programmes and sexual reproductive health services. BMC Public Health. 2012;12(231):231.
South African National AIDS Council. National strategic plan on HIV, STIs and TB 2012–2016. Pretoria: South African National AIDS Council; 2012.
UNESCO. Young people today. Time to act now. Why adolescents and young people need comprehensive sexuality education and sexual and reproductive health services in Eastern and Southern Africa. Paris: UNESCP Publications; 2013.
Peltzer K, Matseke G, Mzolo T, Majaja M. Determinants of knowledge of HIV status in South Africa: results from a population-based HIV survey. BMC Public Health. 2009;9:174.
Napierala Mavedzenge SM, Doyle AM, Ross DA. HIV prevention in young people in sub-Saharan Africa: a systematic review. J Adolesc Heal. 2011;49(6):568–86. doi:10.1016/j.jadohealth.2011.02.007.
Mall S, Middelkoop K, Mark D, Wood R, Bekker L. Changing patterns in HIV/AIDS stigma and uptake of voluntary counselling and testing services: the results of two consecutive community surveys conducted in the Western Cape, South Africa. AIDS Care. 2013;25(2):194–201.
McCauley AP. Equitable access to HIV counseling and testing for youth in developing countries: a review of current practice. Horizons Report. Washington: Population Council; 2004.
Biddlecom AE, Munthali A, Singh S, Woog V. Adolescents’ views of and preferences for sexual and reproductive health services in Burkina Faso, Ghana, Malawi and Uganda. Afr J Reprod Health. 2007;11(3):99.
MIET Africa. Literature Review: Youth friendly health services. Grassroots Health News. 2011. http://www.miet.co.za/site/search/downloadencode/nLaaaqWMqp2zp4Sx.
Heise L, Lutz B, Ranganathan M, Watts C. Cash transfers for HIV prevention: considering their potential. J Int AIDS Soc. 2013;16(18615):1–5.
de Walque D, Dow WH, Nathan R, Abdul R, Abilahi F, Gong E, et al. Incentivising safe sex: a randomised trial of conditional cash transfers for HIV and sexually transmitted infection prevention in rural Tanzania. BMJ Open. 2012;2:e000747.
Pettifor A, MacPhail C, Nguyen N, Rosenberg M. Can money prevent the spread of HIV? A review of cash payments for HIV prevention. AIDS Behav. 2012;16(7):1729–38.
Cluver L, Boyes M, Orkin M, Pantelic M, Molwena T, Sherr L. Child-focused state cash transfers and adolescent risk of HIV infection in South Africa: a propensity-score-matched case-control study. Lancet Glob Heal. 2013;1(6):e362–70.
Cluver LD, Orkin FM, Boyes ME, Sherr L. Cash plus care. AIDS. 2014;28:S389–97.
National Department of Health. South African National AIDS Council. South African HIV and TB investment case: reference report phase 1. Pretoria: National Department of Health; 2016.
PEPFAR. Working Together for an AIDS-free Future for Girls and Women. The United States President’s Emergency Plan for AIDS Relief. 2016. http://www.pepfar.gov/partnerships/ppp/dreams/.
Baird SJ, Garfein RS, McIntosh CT, Özler B. Effect of a cash transfer programme for schooling on prevalence of HIV and herpes simplex type 2 in Malawi: a cluster randomised trial. Lancet. 2012;379(9823):1320–9. doi:10.1016/S0140-6736(11)61709-1.
Kakwani N, Soares F, Son H. Conditional cash transfers in African countries. Brasilia: International Poverty Centre; 2005.
MRC South Africa. Linkage to care following home-based HIV counselling and testing. 2013. http://www.hst.org.za/sites/default/files/LinkageCare.pdf.
Negin J, Wariero J, Mutuo P, Jan S, Pronyk P. Feasibility, acceptability and cost of home-based HIV testing in rural Kenya. Trop Med Int Heal. 2009;14(8):849–55.
Matovu JKB, Kigozi G, Nalugoda F, Wabwire-Mangen F, Gray RH. The Rakai Project counselling programme experience. Trop Med Int Heal. 2002;7(12):1064–7. doi:10.1046/j.1365-3156.2002.00964.x.
National Department of Health. HIV counselling and testing (HCT) policy guidelines. Pretoria: National Department of Health; 2010.
AIDS.gov. Types of HIV tests. HIV test types. 2012. p. 1–2. http://aids.gov/hiv-aids-basics/prevention/hiv-testing/hiv-test-types/.
Acknowledgements
Assistance from colleagues from the research team at CAPRISA was invaluable for conducting this study. A big thank you goes specifically to the team arranging and coordinating the school visits and liaising with school principals and teachers. The authors also acknowledge the input from colleagues at the Health Economics and HIV and AIDS Research Division whose comments have helped to shape this piece of work, specifically Kaymarlin Govender, one of the primary investigators on the overarching VMMC study. The authors thank the team of fieldworkers and data capturers and translators, without whose assistance this study would not have been possible. The authors also acknowledge the financial support of the Swedish International Development Cooperation Agency (Sida), which helped to finance this research.
Funding
Funding for this project was provided by the Heath Economics and AIDS Research Division (HEARD) at the University of KwaZulu-Natal using general funds (no Grant number) supported by the Swedish International Development Agency (SIDA).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Michael Strauss, Gavin George, and Bruce Rhodes declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institution. Permission to conduct this study was obtained from the Human and Social Sciences Ethics Committee at the institution. A waiver of parental consent was granted for participants older than 16 but younger than 18 years, given that children in South Africa can access HCT services without parental consent. All participants signed written informed consent forms before enrollment into the study. This article does not contain any studies with animals performed by any of the authors.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Strauss, M., George, G.L. & Rhodes, B.D. Determining Preferences Related to HIV Counselling and Testing Services Among High School Learners in KwaZulu-Natal: A Discrete Choice Experiment. AIDS Behav 22, 64–76 (2018). https://doi.org/10.1007/s10461-016-1602-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-016-1602-8