Abstract
Late diagnosis of HIV remains a public health issue in Mexico. Most national programs target high-risk groups, not including women. More data on factors associated with late diagnosis and access to care in women are needed. In 2012–2013, Mexican women recently diagnosed with HIV were interviewed. Socio-cultural background, household-dynamics and clinical data were collected. Of 301 women, 49 % had <200 CD4 cells/mm3, 8 % were illiterate, 31 % had only primary school. Physical/sexual violence was reported by 47/30 %; 75 % acquired HIV from their stable partners. Prenatal HIV screening was not offered in 61 %; 40 % attended consultation for HIV-related symptoms without being tested for HIV. Seeking medical care ≥3 times before diagnosis was associated with baseline CD4 <200 cells/mm3 (adjusted OR 3.74, 95 % CI 1.88–7.45, p < 0.001). There were missed opportunities during prenatal screening and when symptomatic women seeked medical care. Primary care needs to be improved and new strategies implemented for early diagnosis in women.
Resumen
El diagnóstico tardío del VIH es un problema de salud pública en México. Los programas nacionales se enfocan principalmente a grupos de alto riesgo que no incluyen mujeres. Falta información sobre los factores asociados al diagnóstico de VIH y acceso a atención médica en las mujeres. En 2012–2013 se entrevistaron mujeres con VIH recién diagnosticado. De 301 mujeres, 49 % tuvo <200 CD4, 8 % eran analfabetas, 31 % solo habían cursado la primaria; 47/30 % reportaron violencia física/sexual; 75 % adquirieron VIH por su pareja estable. En 61 % no hubo escrutinio prenatal; 40 % acudieron a consulta por síntomas relacionados a VIH sin diagnosticarse. Acudir a consulta ≥3 veces antes del diagnóstico se asoció con CD4 basales <200 células/mm3 (RM ajustada 3.74, IC 95 % 1.88–7.45, p < 0.001). Hubo oportunidades perdidas de diagnóstico durante la atención prenatal y en mujeres sintomáticas. Es necesario mejorar la atención primaria e implementar nuevas estrategias para el diagnóstico temprano en mujeres.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In Mexico, HIV is a concentrated epidemic driven by men who have sex with men (MSM), who represent 70 % of the people infected. The national prevalence in the adult population is 0.3 % [1]; in MSM, it reaches 17 % [2]. As in many countries, late stage diagnosis remains an important issue in Mexico for men and women, since almost 60 % of HIV-infected individuals are detected with a CD4 count of less than 200 [3]. This highlights deficiencies in access to care and the need to implement better screening strategies [4]. Many barriers for access to care and early detection have been recognized in different countries, including low socioeconomic status, low educational level, indigenous ethnicity and lack of risk perception [5–7]. Late diagnosis is also the consequence of missed diagnostic opportunities: patients with HIV frequently attend health care centres many times prior to their diagnosis. These contacts with health facilities could have favoured an earlier detection had the HIV test been offered [8–10]. One study reported that missed diagnostic opportunities were more frequent in women than in men [11].
Women account for approximately 20 % of new cases of HIV infection in Mexico. Although this proportion has remained fairly stable in the last 5 years [12], the frequency of heterosexual transmission tends to increase, which directly affects the risk of infection in women; the ratio of infected men to women has decreased from over 1:13 at the beginning of the epidemic, to less than 1:4 in many rural areas of the country in recent years [12, 13].
Social and epidemiological data focusing on Mexican women recently diagnosed with HIV are scarce [14, 15]. Due to the nature of the epidemic, most of the research and the interventions have focused on high-risk groups such as female sex workers or drug users mainly in the Northern Mexican border region [14–17]. These high-risk populations have specific dynamics of transmission, with higher HIV prevalence (up to 15 % in sex workers) [12], multiple partners and more frequent risky behaviours, that cannot be generalized to the overall women population. The women who do not belong to high-risk groups are usually married, have fewer sexual partners [16, 18] and their major risk factor is their stable partner. Although they have a much lower prevalence of HIV (less than 0.1 %), they represent, in absolute numbers, the majority of women infected with HIV in Mexico.
National prevention programs do not generally target women who are considered to be at low risk. Pregnancy is the only context in which women are included in a public official screening program in the country. However, despite being required by a national norm since 2001 in Mexico, prenatal HIV test coverage remains low [9, 15, 19–21]. The failure to offer an HIV test during pregnancy leads to late diagnosis, which results in clinical, economic and emotional consequences [4]. In qualitative studies conducted in Mexico to investigate how women infected with HIV cope with their diagnosis, women reported fear, social isolation and stigma, as well as guilt for having infected their offspring [9, 22]. Late diagnosis and missed diagnostic opportunities are also a failure to prevent mother to child transmission that needs to be addressed.
This urges a re-evaluation of prevention and detection strategies for women and stresses the relevance of gathering more recent information on their sociological and demographic background. The national institution for HIV care and prevention (CENSIDA), as well as the National agency for women (INMUJERES) [16], are trying to understand the factors that could contribute to the vulnerability of women to acquiring HIV and that favour the spread of the epidemic among Mexican women, such as gender-based inequalities, intimate partner violence and economic dependency, which are recognized factors associated with the HIV epidemic in women and with late diagnosis [6, 13, 15, 18]. There is a need to increase the attention given to HIV among women [23], but further investigation on the context is required. The data available on the role of medical services in HIV testing is also insufficient. Knowing the circumstances in which women are diagnosed and the factors associated with late diagnosis would allow us to identify possible targets for intervention to improve early detection in this group.
The aim of this study was to describe, in a sample of Mexican women recently diagnosed with HIV, the clinical stage and circumstances of diagnosis, the factors potentially associated with increased vulnerability to HIV infection, and the role of the health-care system in promoting HIV diagnosis and screening in this population.
Methods
Study Participants
Between August 2012 and August 2013, a quantitative questionnaire was applied through face-to-face structured interviews to Mexican-born women older than 18 years of age who had been diagnosed with HIV infection between 2009 and 2013 at four HIV clinics in different states of the country. Women infected at birth were not included. All women attending the centres for regular clinic visits or for drug pick up who fulfilled the inclusion criteria were invited to participate.
Characteristics of HIV Centres
All the HIV clinics included in this study are part of the public sector. Two of the centres are located in Mexico City, one in Puebla and one in Oaxaca. Mexico City has the highest proportion of HIV cases (20 %) in the country. In Mexico City, the “Clínica Especializada Condesa (CEC)” is an ambulatory HIV referral centre intended for people without social security that provides service, at no cost, to 9000 active patients, mostly MSM. Women represent 11 % of all active patients of this clinic. The other centre in Mexico City is part of the Instituto Nacional de Ciencias Médicas y Nutrición Salvador Zubirán (INCMNSZ), a tertiary care facility that provides care for 1500 HIV positive patients, 12 % of whom are women. In Puebla and Oaxaca, participants were recruited in the ambulatory care centres for HIV called CAPASITS (Centros Ambulatorios de Prevención y Atención en SIDA e ITS), which are also free of charge. Oaxaca is considered one of the poorest states in the country (Growth domestic product is 50 % of the national average) [24], with a high proportion of rural population scattered in small villages and a high proportion of indigenous groups. It was the fifth state with the highest number of HIV cases in 2014. The CAPASITS of Oaxaca follows 1932 active patients, 26 % of whom are women. The centre in Puebla has 2232 active patients, 24.4 % of them women. Puebla is also a state with a high proportion of rural population and a high burden of HIV (the 6th state with the higher proportion of prevalent cases).
Procedures and Measurement
All women attending the centres for regular clinic visits or for drug pick-up who fulfilled the inclusion criteria were invited to participate. Written informed consent was obtained from all of them. A questionnaire containing five main topics was applied: cultural and socio-demographic characteristics (including domestic violence and sexual abuse), medical history (including sexual risk behaviour), circumstances of diagnosis, access to medical care and HIV knowledge (including condom use). Domestic violence was defined as present if the women reported having experienced any physical violence at home at any time, regardless of the aggressor. As for sexual abuse, the women were asked if they had ever suffered from any kind of sexual abuse, at any age and regardless of the aggressor.
The questionnaire consisted of 88 items, replicating a detailed medical history. It was elaborated specially for the study and was previously reviewed by a committee of five physicians, experts in HIV. The questionnaire was piloted by applying it to 15 women (not included in the study and diagnosed before 2009) in order to ensure its understandability and to evaluate its acceptability by women. Corrections were made and questions were adjusted according to the feedback provided by the women in the pilot study. Clinical and demographic data were obtained from the medical files of the women, including clinical stage at diagnosis, CD4 count, AIDS-defining illnesses, comorbidities, co-infections and sexually transmitted diseases (STD).
Statistical Analysis
Descriptive frequencies are reported as percentages, and as measures of central tendency and variation. We used the median and range, since the data were skewed to the right and not normally distributed. Statistical analysis was done with STATA 12.0. For hypothesis testing, a Mann–Whitney U test was used for quantitative variables as a non-parametric test in cases of non-normal distribution. The χ2 test was used for categorical variables. The Kruskal–Wallis test was used for comparison between more than two groups. Late diagnosis was defined as a baseline CD4 count of less than 200 cells/mm3. To evaluate variables associated with late diagnosis in the multivariate analysis, a logistic regression was performed, including in the model all variables for which the crude analysis had shown evidence of an association (defined by p < 0.05), plus any other variable that was considered important enough to be included.
Institutional Review Board
The institutional review board of the four clinics reviewed and approved the study. Before starting the interview, the interviewer reviewed the informed consent with each woman to ensure they understood the confidentiality and anonymity of their statements and their freedom to withdraw from the study at any time. Due to the sensitive nature of some of the topics included in the questionnaires (e.g. violence and sexual abuse), every woman was offered the possibility of being referred to legal counselling and psychological support. Psychologists as well as legal and human rights organisms were identified in each centre to refer the participants if necessary.
Results
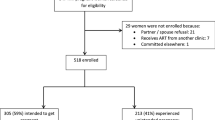
Three hundred and thirty one women were invited to participate; 61 refused to be interviewed and 301 were included in the analysis: 94 (31 %) from CEC, 58 (19.5 %) from INCMNSZ, 100 (33 %) from Oaxaca and 49 (16.5 %) from Puebla. Some women (31) accepted only that their medical file be reviewed but not the interview, most of them stating that they had no time to participate. In total, 270 women were interviewed. Thus, some results include data only from the medical file review, and the entire sample is included only when information could be obtained both from the medical files (clinical and demographic information) and the interviews. Most women (95 %) were born in seven states with the highest rates of HIV infection in the country (Hidalgo, Guerrero, Veracruz, Estado de México, and the three states in which the study was conducted: Mexico City, Puebla and Oaxaca).
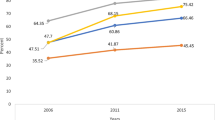
Differences Between States
Women were diagnosed at younger age in Puebla and Oaxaca, compared to Mexico City. There were no differences in the number of pregnancies, age at first pregnancy, or level of education. Indigenous-speaking women represented 25 % of the sample in Oaxaca, 9.5 % in Mexico City, and 4 % in Puebla. Only two of these women did not speak Spanish, and thus the interview was done with a translator, which in both cases was the women’s offspring. Translators are sometimes available in reference centres in rural areas, but no translator was assigned for the study. In Mexico City, there was a larger proportion of women with history of substance abuse, paid sex and sexual abuse (Table 1). The CD4 count at diagnosis was higher in Oaxaca (294 cells/mm3) than in other states (111 in INSCMNSZ and 194 in Puebla, Kwallis test, χ2 = 26.3, p < 0.001). Women had more frequently been diagnosed through pregnancy in Oaxaca. Moreover, women from Oaxaca and Puebla tended to have been diagnosed more frequently in recent years (72 % of the women interviewed in Oaxaca and 83 % of women from Puebla were diagnosed after 2011, compared to 36.5 % of the women from INCMNSZ, and 53 % of the women from CEC). There were no differences between centres regarding medical care prior to HIV diagnosis.
Circumstances of Diagnosis and Clinical Stage
Seventy five percent of the women stated that they had acquired HIV through their stable partners. The reason for taking the HIV test was because a partner or an offspring had been diagnosed with HIV in 38 % of the cases (33 % the partner and 5 % the offspring). In 35 % of the women, HIV testing and diagnosis were prompted by the presence of HIV-related symptoms. Only 10 % of the cases were diagnosed through the pregnancy screening program. The median age at HIV detection was 32 years. The median CD4 count at diagnosis was 203 cells/mm3; 49 % had less than 200 CD4 cells/mm3, 27.5 % had an AIDS-defining event at the time of HIV diagnosis, and 33 % an STD infection, mainly with human papilloma virus (HPV). Hepatitis B or C co-infections were observed in 6 women (2 %). At least one comorbidity was reported in 21 % of the cases, more frequently dyslipidemia (14 %), systemic arterial hypertension (4 %) and diabetes mellitus (5 %).
Socioeconomic Factors
In general, participants had a low level of education: 8 % of the women were illiterate, 31 % had primary school as the highest level, and only 30 % had studied beyond secondary school; 14 % of the women (most of them from Oaxaca) spoke an indigenous language.
The social context of the women is shown in Table 2. Domestic violence was reported by 47 % of the women, and sexual abuse by 30 %. In both cases, the first aggressor was a stable partner (current or past). History of imprisonment, illicit substance abuse, or alcohol-related problems were reported by 4, 11 and 11 % of the women respectively. Twenty-five women (9 %) reported having sex for money more than once.
The median age at sexual initiation was 17 years, and almost a third of the women had their first pregnancy during their teens (Table 2). Regarding condom use, 66 % had never or almost never used a condom prior to their diagnosis. Fifty three percent of the women did not have a regular job. The monthly average income was less than 500 USD for 94 % of the women.
Medical and Prenatal Care
Forty percent of the women had sought medical care prior to diagnosis for symptoms such as fever, diarrhoea, weight loss, oral candidiasis, or herpes; 66 % of them had contact with the medical system for these symptoms more than three times before being tested for HIV. Furthermore, almost 70 % of the women diagnosed through symptoms had sought medical care prior to their diagnosis. As for prenatal care, 90.5 % of women had been pregnant, and 71 % had received prenatal care during all their pregnancies. Still, 61 % stated they were not offered an HIV test during any of their pregnancies.
Variables Associated with Low CD4 Count at Diagnosis
Univariate Analysis
The crude analysis showed strong evidence of an association between the circumstances of diagnosis and a higher baseline CD4 count (Kwallis test, χ2 = 41.16, p < 0.001): women diagnosed with HIV-related symptoms had a lower CD4 count than women diagnosed during pregnancy (108 vs. 322 cells/mm3) (Fig. 1). Younger age at diagnosis (<30 years) was associated with a higher baseline CD4 count (64 % had ≥200 cells/mm3 compared to 44 % in women >30 years (OR 2.32, CI 95 % 1.38–3.89, χ2 = 10.9, p = 0.001). Women who sought medical care for HIV-related symptoms 3 or more times without being offered an HIV test had a lower CD4 count at diagnosis compared to women who attended less than three visits. The more health care visits they had attended without being tested, the lower the CD4 count at diagnosis, (Kwallis test, χ2 = 41.3, p < 0.001) (Fig. 2). We also found, as mentioned previously, an association between the centre of inclusion and the level of baseline CD4. The year of diagnosis was not associated with a low CD4 count.
Having experienced physical or sexual violence, speaking an indigenous language, having low education or being younger at first pregnancy were not associated with a lower baseline CD4 count. However, women who experienced physical violence were more frequently diagnosed through symptoms and when they were older than 40 years of age (OR 1.88, CI 95 % 1.12–3.15, χ2 = 6, p = 0.014 and OR 2.42 CI 95 % 1.33–4.43, χ2 = 8.9, p = 0.003, respectively). There was no association between the year of diagnosis and late stage diagnosis.
Multivariate Analysis
All the variables that were associated with late diagnosis in the crude analysis were included in the multivariate model: age at diagnosis, diagnosis through pregnancy, medical contact prior to diagnosis and site of inclusion. The year of diagnosis was also included, since there was an increase in diagnosis through pregnancy in recent years (5 % before 2011 and 14 % afterwards, χ2 = 4.7, p = 0.031), and to account for other potential confounders associated with time that had not been measured. After adjusting for those variables in the logistic regression, there remained strong evidence of an association between seeking medical care prior to diagnosis and having a low baseline CD4 count. The women who sought medical care for HIV-related symptoms 3 or more times were almost 4 times more likely to be diagnosed with a CD4 count of less than 200 compared to women who sought medical care less than 3 times (adjusted OR 3.75, CI 95 % 1.88–7.45, Wald test, Z = 3.77, p < 0.001). There was also weak evidence of an association between age at diagnosis and late diagnosis after controlling for the other variables (adjusted OR 1.79, CI 95 % 0.98–3.27, Wald test, Z = 1.9, p = 0.057) (Table 3).
Discussion
Almost half of the women in this sample were diagnosed with a CD4 count of less than 200, which is the usual cut-off value for late stage diagnosis, since it is associated with an increased frequency of opportunistic infections and mortality, a poorer response to treatment and worse prognosis [4]. This is not exclusive of women, as recent reports describe late diagnosis in almost 60 % of the Mexican population infected with HIV, including men [25]. Many studies, even in developed countries, show a significant proportion of late diagnosis, usually related to variables such as age, gender, foreign origin and education level, amongst others. Late diagnosis has been associated with increased morbidity and mortality, and remains a preventable cause of HIV-related morbidity in the era of universal HAART access [4].
In our sample, late diagnosis was the result of missed diagnostic opportunities due to two main scenarios: the first scenario is the failure to offer an HIV test to women attending prenatal care. The second scenario is the failure to offer an HIV test even to women who were using medical services due to symptoms that should have prompted a test. The fact that the small group of women diagnosed during pregnancy had higher CD4 counts at diagnosis reflects the consequences of missing diagnostic opportunities and evidences the benefits of screening.
With respect to the first scenario, offering an HIV test is mandatory during pregnancy in Mexico [21], and yet, two decades after the first study demonstrated that prenatal testing is the most efficient measure to prevent HIV transmission to children, the proportion of pregnant women tested for HIV is still low [9, 15, 19, 20]. In our sample, 61 % of the women reported they had never been offered an HIV test during any of their pregnancies. In fact, in 12 women, HIV testing was prompted by a diagnosis of HIV in their children, which confirms the failure to detect the disease during prenatal care. The results of national reports about prenatal coverage tend to vary. The results of this study are similar to what was reported by CENSIDA (National Centre for Prevention and control of AIDS) in 2011, when coverage was 34 % [26], but are a little higher than what was reported by a national health survey carried out in 2012, when 54 % of registered pregnant women were offered an HIV test [19]. It is also estimated that in 2014, 121 cases of HIV infection due to perinatal transmission were detected [27]. The absence of prenatal testing keeps occurring despite the fact that many reports have shown a high rate of acceptance of HIV testing among Mexican women [28–30]. The low coverage of HIV testing seems to be more related to the failure of offering the tests than to women declining to take them, evidencing deficiencies in the programs designed to prevent mother to child transmission in the country, an important public health issue that needs to be addressed. The national institutions for HIV care and prevention (CENSIDA) have tried to emphasize this issue in recent years, and improving coverage of prenatal HIV testing is an important target at a national level.
Since there are limited opportunities for HIV testing in women, determining other opportunities to offer an HIV test to women could be another useful strategy. In a retrospective study in South Carolina, Duffus et al. [10] analysed all medical contacts recorded in databases of women diagnosed with HIV and found that 73 % had previously visited a health-care facility, during a period when it was assumed that they were already HIV-positive, without being offered an HIV test. Half of these women were late testers and most of them were older women beyond reproductive age who could not take advantage of the only established routine screening programs for women (during prenatal care). The authors concluded that other testing strategies should be implemented in order to include women not belonging to the groups traditionally perceived as being at risk; these alternative strategies could be based on STD family planning and cervical cancer screening clinics. This recommendation was also highlighted in another retrospective study in North Carolina that found that men were three times more likely to be diagnosed in their first contact with health care than women. One of the possible explanations suggested by the author is that women tend to have more regular medical contacts through gynaecological services, which are not used for testing. In our study, we found that an STD was detected in 40 % of the women at diagnosis, mainly HPV (72.6 %). This seems a good opportunity to offer an HIV test, since cervical cancer screening clinics are major points of contact with the medical system for women.
Another possible explanation of the increase in missed diagnostic opportunities for women attending health care centres compared to men, is that it might be easier for men to be offered an HIV test when attending a health centre due to stereotyped definitions of risk [11]. Although marriage has been reported as one of the main risk factors for HIV infection in women [16, 18], they do not fit into the high-risk profiles defined for a concentrated epidemic. The majority of women in our sample had few partners and 75 % were infected by their stable partners; hence, most of the women in this sample would be considered as a low-risk group. This lack of risk perception among health care providers results in women attending health care centres several times for symptoms that should prompt an HIV test, delaying the diagnosis at the primary care level, with important clinical and prognostic implications. This leads to the second scenario considered in this study, in which 40 % of the women attended health care centre for HIV-related symptoms without being offered an HIV test, and in which an increasing number of medical contacts is associated with an increased risk of late diagnosis. Expanding HIV screening to avoid depending on pre-established risk profiles for decision-making could be a way to address this issue.
Regarding the association of socio-economic determinants with HIV, there were some factors in the study that could contribute to increase the vulnerability of women to HIV. The women in our sample had a low socioeconomic level (including low education levels and low monthly income), high prevalence of physical and sexual abuse, young age at first pregnancy and low condom use. If we make a comparison with national data from a demographic survey (INEGI) [31], some of these factors seem to reflect the general conditions of the population: the prevalence of illiteracy found by us (8 %) is similar to the one reported for women at national level (7 %) in 2010 [31]. Moreover, in that year, 35 % of the population had primary school as the highest level of studies (compared to 30 % in this study). We also found a lower monthly average income compared to the national data: in 2012, 58 % of the population included in the national survey earned less than 500 USD a month, compared to 94 % in this sample [24]. Early pregnancies were also more frequent in our sample than at the national level: in 2013, INEGI reported 19.4 % of mothers with less than 20 years of age, compared to 41 % in our sample.
Regarding violence, national surveys report a prevalence of physical violence ranging from 40 to 60 % in women (we report 47 % in this study) [24, 32]. However, there was a higher prevalence of sexual abuse (30 %) in our group of women compared to the national surveys (17 %). Other studies have shown the negative impact of sexual violence on the adoption of protective behaviours, such as condom negotiation, HIV disclosure to the partner and seeking health care, which, in turn, has an effect on the incidence of HIV. Previous reports have shown that intimate partner violence is associated with a higher incidence of HIV infection [6], and also that HIV disclosure generates violence, not only in the family but also in the health system: in a survey with 80 women with HIV from different regions of Mexico, the women reported frequent psychological violence and discrimination from health care workers as a consequence of disclosing their diagnosis [33]. In addition, violence and stigmatization can limit access to health care [34, 35]. In our sample, we did not find an association between these variables and a low CD4 count at diagnosis, but we did find that women who had experienced physical violence tended to be diagnosed more frequently through symptoms and at an older age. These social factors do represent potential adverse situations that could be improved through empowerment and education, which in turn could facilitate care-seeking behaviours.
With respect to the differences between the centres, some of them are related to the characteristics and location of each centre, as well as to the population serviced by them. The Oaxaca centre treats individuals coming from a more rural setting and is expected to have a higher number of indigenous language-speaking people. On the other hand, CEC is located in an urban setting with a higher number of women reporting paid sex and drug abuse. However, other differences were less expected. The fact that Oaxaca, being a rural setting, had a higher level of baseline CD4 count, as well as a higher proportion of women diagnosed at a younger age and through pregnancy was initially surprising. However, this was possibly associated with the year of diagnosis: the women interviewed in Oaxaca tended to have been diagnosed more recently compared to the other centres. This could represent a selection bias, with women from Oaxaca reflecting an improvement in recent years in terms of increasing coverage of prenatal HIV testing in women.
We also found a high prevalence of women speaking an indigenous language (14 %), (most of them from Oaxaca, 25 %) compared to national data, which showed an overall prevalence of 6.5 % in the whole country, and regional variations as high as 33.9 % for Oaxaca, and 11.9 % for Puebla [31]. It is worth noting that approximately 9 % of women in the Mexico City centres spoke an indigenous language, a much higher proportion than that reported for the general population in Mexico City (1.5 %). Most of these women had migrated many years before and had been living in the city for more than 10 years (70 %). This could suggest that women who speak an indigenous language and who migrate from rural areas have certain conditions that contribute to a higher risk of being infected with HIV; however, the limitations of the sampling make this difficult to ascertain. Although we found that this group of women had lower income and lower education, we did not find an association with late stage diagnosis. Whether a larger sample would show such an association remains to be evaluated, and further studies are needed to understand if migration to a big city increases the risk of acquiring HIV for these women.
This study has some limitations. It is an observational study that included only women infected with HIV and hence we cannot ascertain that the sociodemographic characteristics found in this study are associated with an increased vulnerability to HIV since there was no comparison group. Another limitation is that the women included in the study were not randomly selected and are also the ones that are already linked to care and willing to participate in such a study. This limits the generalizability of the results. However, the sample included women from the main referral centres in 3 states that have a high burden of HIV, with the women coming from different settings (urban and rural), which increases the representativeness of the study population.
In conclusion, we found several barriers to an early HIV diagnosis in this sample of Mexican women. The best scenario for the women to be detected with a higher CD4 count was to be pregnant, which reflects the lack of screening opportunities for non-pregnant women, and demands a reconsideration of the strategies for early detection in countries with concentrated epidemics. The study also highlights possible interventions to improve HIV detection at the primary care level, considering the low frequency of HIV test offering. One target could be the expansion of HIV testing through HPV screening clinics and other major contact points for women within the medical system, such as family planning clinics. Improving the coverage of prenatal care is also absolutely needed. There was also a high prevalence of social and cultural factors that might play a role in increasing women’s vulnerability to HIV; the role of these factors in the dynamics of HIV transmission demands further investigation.
References
Secretaria de Salud CENSIDA. El VIH/SIDA en México 2012. www.censida.salud.gob.mx/descargas/biblioteca/VIHSIDA_MEX2012.pdf. 2012.
Bautista-Arredondo S, Colchero MA, Romero M, Conde-Glez CJ, Sosa-Rubi SG. Is the HIV epidemic stable among MSM in Mexico? HIV prevalence and risk behavior results from a nationally representative survey among men who have sex with men. PLoS One. 2013;8(9):e72616.
Crabtree-Ramirez B, Caro-Vega Y, Belaunzaran-Zamudio F, Sierra-Madero J. High prevalence of late diagnosis of HIV in Mexico during the HAART era. Salud Publica Mex. 2012;54(5):506–14.
Fisher M. Late diagnosis of HIV infection: major consequences and missed opportunities. Curr Opin Infect Dis. 2008;21(1):1–3.
Zambrana RE, Cornelius LJ, Boykin SS, Lopez DS. Latinas and HIV/AIDS risk factors: implications for harm reduction strategies. Am J Public Health. 2004;94(7):1152–8.
Jewkes RK, Dunkle K, Nduna M, Shai N. Intimate partner violence, relationship power inequity, and incidence of HIV infection in young women in South Africa: a cohort study. Lancet. 2010;376(9734):41–8.
Tariq S, Elford J, Cortina-Borja M, Tookey PA. National Study of HIViP, Childhood. The association between ethnicity and late presentation to antenatal care among pregnant women living with HIV in the UK and Ireland. AIDS Care. 2012;24(8):978–85.
Nakao JH, Wiener DE, Newman DH, Sharp VL, Egan DJ. Falling through the cracks? Missed opportunities for earlier HIV diagnosis in a New York City Hospital. Int J STD AIDS. 2014;25(12):887–93.
Kendall T. Consequences of missed opportunities for HIV testing during pregnancy and delayed diagnosis for Mexican women, children and male partners. PLoS One. 2014;9(11):e109912.
Duffus WA, Davis HT, Byrd MD, Heidari K, Stephens TG, Gibson JJ. HIV testing in women: missed opportunities. J Womens Health (Larchmt). 2012;21(2):170–8.
Chin T, Hicks C, Samsa G, McKellar M. Diagnosing HIV infection in primary care settings: missed opportunities. AIDS Patient Care STDS. 2013;27(7):392–7.
Secretaria de Salud CENSIDA. Informe Nacional de Avances en la respuesta al VIH y el SIDA. www.censida.salud.gob.mx/descargas/ungass/garp2014.pdf. 2014.
Allen Leigh B., P. TP. Género, poder y VIH/SIDA en la vida de las mujeres. In: Pública INdS, editor. 25 años de VIH en México: logros, desaciertos y retos 2009.
De Boni R, Veloso VG, Grinsztejn B. Epidemiology of HIV in Latin America and the Caribbean. Curr Opin HIV AIDS. 2014;9(2):192–8.
Garcia PJ, Bayer A, Carcamo CP. The changing face of HIV in Latin America and the Caribbean. Curr HIV/AIDS Rep. 2014;11(2):146–57.
INMUJERES C, INSP. Mujeres, adolescentes y niñas mexicanas: una mirada comprensiva en torno al VIH y el SIDA. Epidemiología, prevención, atención y mejores prácticas en México. SIDA Ad, editor 2010.
Ramos RL, Ferreira-Pinto JB, Rusch ML, Ramos ME. Pasa la voz (spread the word): using women’s social networks for HIV education and testing. Public Health Rep. 2010;125(4):528–33.
Hirsch JS, Meneses S, Thompson B, Negroni M, Pelcastre B, del Rio C. The inevitability of infidelity: sexual reputation, social geographies, and marital HIV risk in rural Mexico. Am J Public Health. 2007;97(6):986–96.
Torres JV. Prevención de la transmisión perinatal del VIH/SIDA en México por medio de la aplicación de la prueba en mujeres embarazadas. Mexico: Facultad Latinoamericana de Ciencias Sociales; 2014.
Uribe Zuñiga P., Ortiz Ibarra F.J., G. HT. La prevención de la transmisión perinatal. In: Instituto Nacional de Salud Pública, editor. 25 años de VIH en México: logros, desaciertos y retos. Second ed 2009. pp. 73–92.
Secretaria de Salud. Norma Oficial Mexicana para la prevención y control de la infección por virus de la inmunodeficiencia humana, NOM-010-SSA2-2010,. www.salud.gob.mx/unidades/cdi/nom/010ssa23. 2010.
Holtz CS, Sowell R, Velasquez G. Oaxacan women with HIV/AIDS: resiliency in the face of poverty, stigma, and social isolation. Women Health. 2012;52(6):517–35.
Secretaria de Salud CENSIDA. Guia Nacional para la Prevencion del VIH y el Sida. www.censida.salud.gob.mx/descargas/principal/GUIA_NACIONAL_2014.pdf. Mexico 2014.
INEGI. Censo de Población y vivienda 2012. www.inegi.org.mx. 2012.
Crabtree-Ramirez B, Caro-Vega Y, Shepherd BE, Wehbe F, Cesar C, Cortes C, et al. Cross-sectional analysis of late HAART initiation in Latin America and the Caribbean: late testers and late presenters. PLoS One. 2011;6(5):e20272.
CONASIDA. La cobertura de pruebas de detección del VIH en embarazadas en México. Boletín del Grupo de Información Sectorial en VIH/SIDA. 2011.
Secretaria de Salud CENSIDA. Vigilancia Epidemiológica de casosde VIH/SIDA en México Registro Nacional de Casos de SIDA. www.censida.salud.gob.mx/descargas/epidemiologia/RN_CIERRE_2014.pdf. 2014.
Romero-Gutierrez G, Delgado-Macias AA, Mora-Escobar Y, de Leon ALPP, Amador N. Mexican women’s reasons for accepting or declining HIV antibody testing in pregnancy. Midwifery. 2007;23(1):23–7.
Viani RM, Araneta MR, Ruiz-Calderon J, Hubbard P, Lopez G, Chacon-Cruz E, et al. Perinatal HIV counseling and rapid testing in Tijuana, Baja California, Mexico: seroprevalence and correlates of HIV infection. J Acquir Immune Defic Syndr. 2006;41(1):87–92.
Vera GL, Gongora BRA, Pavia RN, Gaber OJ, Lara PD, Alonzo SL. [Acceptability of a test for antibodies against HIV in a group of pregnant women in Yucatan, Mexico]. Ginecol Obstet Mex. 2005;73(7):355–9.
INEGI. Censo de Población y Vivienda 2010: Tabulados del Cuestionario Básico. www.inegi.org.mx. 2010.
Instituto Nacional de Salud Pública, Secretaria de Salud. Encuesta Nacional sobre Violencia contra las Mujeres. 2003.
Kendall T, van Dijk M, Wilson KS, Picasso N, Lara D, Garcia S. A lifetime of violence: results from an exploratory survey of Mexican women with HIV. J Assoc Nurses AIDS Care. 2012;23(5):377–87.
Gonzalez A. Poverty and gender inequalities reduce the quality of life of women living with HIV/AIDS in Chiapas, Mexico. AIDS Conference Abstract no TUPE0696 2008.
Theilgaard ZP, Katzenstein TL, Chiduo MG, Pahl C, Bygbjerg IC, Gerstoft J, et al. Addressing the fear and consequences of stigmatization—a necessary step towards making HAART accessible to women in Tanzania: a qualitative study. AIDS Res Ther. 2011;8:28.
Acknowledgments
To all the women who participated in the study’s interviews.
Author’s Contributions
AMO, PVF and JSM contributed to the design, implementation and analysis of data. VAW contributed to implementation of the study and analysis. AGR, JCR, LRA, ITE all contributed to the study design and analysis.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
AMO has received honoraria from Abbvie for an advisory board and a symposium. PVF has received honoraria from Abbvie for advisory boards and as a speaker. VAW declares she has no conflict of interest. AGR declares she has no conflict of interest. JCR declares he had no conflict of interest at the moment of the study but is currently working as medical manager in Stendhal. LRA declares she has no conflict of interest. ITE has received financial support from BMS and speaker honoraria from Abbvie and Stendhal. JSM has received speaker honoraria from Stendhal and Gilead, is a consultant for MSD, Stendhal and Pfizer and has received research support from Pfizer, BMS and GSK.
Ethical Approval
All procedures performed in this study were in accordance with the ethical standards of the institutional research committees and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Martin-Onraët, A., Volkow-Fernández, P., Alvarez-Wyssmann, V. et al. Late Diagnosis Due to Missed Opportunities and Inadequate Screening Strategies in HIV Infected Mexican Women. AIDS Behav 21, 505–514 (2017). https://doi.org/10.1007/s10461-016-1560-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-016-1560-1