Abstract
PHQ-9 data from persons living with HIV (PLWH, n = 4099) being screened for depression in three clinics in the southeastern USA were used to determine the prevalence of suicidal ideation (SI). SI was reported by 352 (8.6 %); associated with <3 years since HIV diagnosis (1.69; 95 %CI 1.35, 2.13), and HIV RNA >50 copies/ml (1.70, 95 %CI 1.35, 2.14). Data from PLWH enrolled in a depression treatment study were used to determine the association between moderate-to-high risk SI (severity) and SI frequency reported on PHQ-9 screening. Over forty percent of persons reporting that SI occurred on “more than half the days” (by the PHQ-9) were assessed as having a moderate-to-high risk for suicide completion during the Mini International Neuropsychiatric Interview. SI, including moderate-to-high risk SI, remains a significant comorbid problem for PLWH who are not fully stabilized in care (as indicated by detectable HIV RNA or HIV diagnosis for less than 3 years).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Suicidal ideations (SIs), both passive (thoughts that life is not worth living or that an individual wishes to be dead) and active (plans to act on such thoughts) [1, 2], are among the strongest and most proximal risk factors for suicide attempts and completions. Suicidal thoughts and behaviors are typically regarded as occurring on a continuum of severity from passive SI (the mildest form) to suicide completion. In the US general population, suicidal ideation is not uncommon, with 16 % of young adults aged 17–39 reporting SI at some point during their lives [3]. Suicide attempts are less common; in the same young adult population 5.5 % endorsed having made an attempt at some point during their lifetime. The relationship between suicide attempts and completions is complicated, but in general, suicide attempts are 10–20 times more common than completions [4].
Suicide ideation, attempts and completions are well-recognized complications among people living with HIV (PLWH). Initially, HIV-related suicide was examined in the context of terminal untreatable AIDS, similar to Huntington’s disease, and rates were found to be 7.4-fold (US) to 37-fold (in New York City) higher than in the general population [5, 6]. Subsequently, a bi-directional association was recognized, with HIV infection occurring more frequently in those individuals at risk for suicidal behavior, as well as HIV infection triggering suicidal behavior. In a meta-analysis of studies reporting suicidal behavior in both the antiretroviral therapy (ART) and pre-ART eras, completed suicide was the reported cause of death in 9.4 % of the subjects [7]. Recent studies found that the rate of suicide completion among PLWH in Switzerland and the US Armed Forces was three times that of the general population and remained unchanged from 2005 to 2009 [8, 9] and the proportion and number of deaths by suicide PLWH in San Francisco has increased in recent years [10]. Additionally, depression and SI continue to be reported by populations of PLWH in the US who experience health disparities [11, 12].
SI is also a significant comorbidity. US cohort studies conducted in the early 2000s describe prevalence of recent (<1 week) SI as being 27–40 % [13, 14]. Many factors contributed to this phenomenon, including male gender, anticipation of terminal illness with AIDS, comorbid depression, substance use disorders, social isolation, stigma, and activity-limiting physical symptoms [15–17]. The advent of effective and well-tolerated ART has led to increased life expectancy and improved quality of life, but SI rates remain similar to those of other populations living with chronic medical illnesses such as arthritis [18], chronic non-cancer pain (28 %), diabetes (25 %), epilepsy, and multiple sclerosis (15 %) [19–21] in the US and in the UK [22]. SI is a complex phenomenon. In a recent meta-analysis, SI was reported as occurring in 25–30 % of PLWH but was measured by a variety of instruments and precise comparisons across studies were not possible [7]. At the end of the first post-ART decade (2003–2007), SI was reported by 26 % of PLWH in the CHARTER study (CNS HIV Antiretroviral Effects Research), using the Composite International Diagnostic Interview (CIDI) [15]. Several prior reports [23, 24] indicate the usefulness of the PHQ-9 screen that was used in this study.
Among PLWH active and passive SI indicate the continued presence of distress [7, 25, 26]. Depression screening conducted at two US HIV clinics revealed SI in 14 % of screened individuals who were predominantly white and male and completed screening prior to 2009 [23]. HIV therapy has continued to evolve since 2009 with multiple single tablet regimens becoming available. In the present study of a majority non-white cohort in the post-ART era we propose an algorithm for assisting non-psychiatrists in the management of suicidal ideation and determine: (1) the prevalence of self-reported active and passive SI; (2) the severity of depression associated with SI; (3) the association between frequency and severity of SI; and (4) the clinical and demographic factors associated with SI. The prevalence of SI was examined using PHQ-9 screening data from PLWH attending HIV care appointments. The association between the frequency of SI as reported by PHQ-9 screening and the severity of SI as reported on the Mini International Neuropsychiatric Interview was examined using data from a depression treatment study for PLWH. The aim of these analyses is to further the understanding of SI in PLWH, in order to prevent suicide completion, treat comorbid psychiatric illness and improve quality of life.
Methods
Sites and Patient Populations
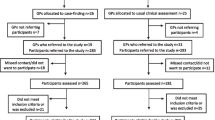
Sites 1, 2, and 4 are large clinics housed in academic medical centers that provide HIV care to 1800–2050 patients annually. These sites participated in routine screening for depression using the PHQ-9. Site 3 is a small rural clinic that did not participate in screening. To describe the suicide risk in the general HIV clinic populations at the three sites with screening, demographics, clinical characteristics and depression screening results of all patients (first screen if multiple were collected) were collected over a 12-month period: January–December 2011 (site 4, n = 1308 screened of approximately1800 clinic patients), February 2011 to January 2012 (site 1, n = 1371/1850), and January–December 2012 (site 2, 1420/2050) for a total of 4099/5700 (Supplementary material). PLWH who declined screening were not tracked. Patients at all clinics were predominantly African-American and male, consistent with the epidemiology of HIV in the southeastern United States.
Depression Treatment Study
Patients were enrolled in the treatment study (n = 304) between April 2010 and October 2013, if they had major depressive disorder diagnosed by Mini International Neuropsychiatric Interview (MINI) and were receiving or initiating antiretroviral therapy. The MINI data for one subject was not entered into the data collection tool, bringing the total number of subjects for this analysis to 303. Patients who were enrolled in the treatment study also completed a PHQ-9. The clinic screening and depression treatment study PHQ-9 data and patient characteristics (demographics, clinical parameters) were collected independently and are reported separately. Patients were excluded who met MINI criteria for bipolar disorders or psychotic symptoms, had failed two or more antidepressant trials of six or more weeks at a moderate/high dose during the current depressive episode, were mentally incompetent, or required immediate psychiatric hospitalization. Demographic and depression information for the screened populations were obtained from clinical records which only included male/female as gender choices. The data were not linked between the screened and enrolled populations.
Measures
Depression screening by PHQ-9 was integrated into clinical care practices at two clinics (site 1 and site 4) during the depression treatment study enrollment period [27]. At site 2, PHQ-9 screening was already established [28]. Each site had a plan for an immediate clinical response to reports of SI: immediate page to a clinical psychologist (one site), or HIV provider notification and subsequent social worker evaluation and emergency room transfer as needed (two sites). SI was assessed with question 9 on the PHQ-9: “In the past 2 weeks, how often have you been bothered by thoughts that you would be better off dead or of hurting yourself in some way?” with response options of “not at all”, “several days”, “more than half the days”, or “nearly every day”. PHQ-9 scores of 10 or greater, in the presence of anhedonia or depressed mood (Questions 1, 2), were considered consistent with moderate to severe depressive symptoms (depression) based on a reported sensitivity and specificity of 88 % for major depressive disorder [29]. Subscales of affective and somatic depressive symptoms were created as these have been found to be useful when examining depression in the context of medical illness [30–32]. An affective subscale consisting of questions regarding anhedonia, depressed mood, and failure/guilt, and a somatic subscale consisting of questions about changes in sleep, appetite, fatigue, concentration and psychomotor activity were constructed. In other reports, the cognitive question regarding concentration and the SI question were included in a cognitive/affective subscale [32–34]. A purely affective subscale was created by removing the SI question to avoid redundancy with the outcome measure and placing the cognitive item in the somatic subscale due the high prevalence of cognitive difficulties in PLWH. The subscales allowed us to examine the associations with somatic and affective symptoms separately.
Patients who received a PHQ-9 score ≥10, were recommended by their medical provider to the treatment study and expressed an interest in enrolling in the study, completed a structured clinical assessment with the Mini International Neuropsychiatric Interview (MINI) to confirm the presence of major depressive disorder and assess current suicidality. The selection process has been previously described [35]. The SI assessment on the MINI asks the respondent: “In the past month, did you: Think that you would be better off dead or wish you were dead; Want to hurt yourself; Think about suicide; Have a suicide plan; or Attempt suicide? And in your lifetime, did you ever make a suicide attempt?”
Characterization of and Clinical Response to SI
When clinical screening with the PHQ-9 was initiated routinely, HIV physicians and staff, who did not routinely assess suicide risk, were confronted with reports of SI more frequently than anticipated and providers raised many questions. Key questions focused on how to combine clinical information obtained about the context and thoughts of suicide into a formal risk assessment; how to manage patients with passive suicidality; the safety of starting medications in the presence of SI; and how to determine who needed psychiatric evaluation or immediate inpatient admission. Training on assessing SI was requested at one of the two sites that were new to routine depression screening. The key points of the training were: the low risk of suicide completion if only passive suicidality is present; identifying patients with high risk, active SI requires immediate psychiatric consultation and/or inpatient admission; and the appropriate follow-up for patients not being referred to psychiatry. Using published suicide risk assessment tools [36] and the clinical experience of the study psychiatrist, an algorithm was created with specific questions to use in the assessment of suicidal thoughts. A simplified version is presented here (Table 1). SI was categorized into thoughts that were passive (thoughts of being better off dead without thoughts of self-harm) or active (thoughts of self-harm). Active SI was further categorized into thoughts of self-harm without either plan or intent for self-harm (active low risk), SI with a plan or prior attempt without intent (active moderate risk), and SI with intent for self-harm (active high risk).
Study Analysis and Statistics
Frequency distributions and means were used to describe characteristics of the study population (demographics, clinical characteristics, depression screening results) and to examine reported suicidal ideation and depressive severity. Bivariable log-linear regression was used to model the prevalence of suicidality by each predictor variable. Predictor variables included age, sex, race, time in care (<3 vs. ≥3 years), HIV RNA viral load (≥50 vs. <50 copies/ml), CD4 count (<200 vs. ≥200 cells/mm3), total PHQ-9 score, affective symptoms score, somatic symptoms score, any hazardous alcohol or current drug use other than marijuana, and history of mood disorder. Time in care was categorized as less than or greater than 3 years to separate people who were still adjusting to being HIV infected and in care vs. those who could be expected to have completed this adjustment. A 3-year breakpoint was made selected based on qualitative data reporting that the first year (at a minimum) is a difficult adjustment time [37, 38]. The intent of this category was include those individuals in the initial adjustment period including those for whom this adjustment period was prolonged. Therefore, based on the clinical experience of the medical providers, a 3-year breakpoint was selected a priori for this analysis. Once the patient characteristic frequencies were calculated, the category population size was determined to be an approximation of the lowest tertile of care duration. This group was of sufficient size to allow meaningful statistical analyses and the category was kept in the analyses. All analyses were conducted using Stata 11 (StataCorp LP, College Station, TX).
Results
The demographics of the clinical and study populations reflected the HIV epidemic in the southeastern US (Table 2). The three clinics had an average 12-month combined population of approximately 5700 patients at the time of routine PHQ-9 depression screening. Information on patients without PHQ-9 screening information (missed, declined, ineligible) was not tracked. Over 12 months, 4099 unique patients (72 %, 4099/5700) completed the screening. The clinical populations were mostly male (74 %), over 40 years of age (71 %), non-white (61 %), established in HIV care (>3 years, 70 %), with suppressed HIV RNA (HIV RNA <50 copies/ml, 72 %), and normal CD4 counts (>500 cells/mm3, 56 %). Demographics of the enrollees were similar to the screened group except more were non-whites (70 %), and in care for longer than three years (83 %), and fewer had complete viral suppression (68 %). A lifetime history of suicide attempts was very high (35 %) and half of these patients (155/303) reported SI on the MINI. Some described intent (n = 40), a plan [21], and/or a recent attempt (n = 6).
Prevalence of PHQ-9 scores greater than or equal to 10 was 17 % in the screened population (Table 3) and varied from 13 to 21 % at the three sites (data not shown). Approximately 8.6 % of screened clinic patients reported some level of SI on the PHQ-9 and 1.3 % reported that these thoughts occurred almost daily. Moderate to high severity of affective symptoms was reported as frequently as moderate to high total PHQ-9 total scores (17 %), while moderate to high severity of somatic symptoms were reported with somewhat greater frequency (21.7 %). SI was examined in the presence or absence of a PHQ-9 score for moderate or severe depression. Of the 352 individuals with SI, the majority reporting SI, 277 (277/353, 79 %) did so in the presence of moderate to severe depressive symptoms. However, one in five (75/352, 21 %) reported SI in the absence of significant symptoms of depression.
The responses to the suicide question on the PHQ-9 by study enrollees were compared with the responses to the suicide assessment questions on the MINI that was completed within 24 h of the PHQ-9 for 89 % of enrollees and within 14 days for all enrollees (Table 4). This allowed for an analysis of the association between reports of SI frequency (PHQ-9 data) and SI severity (MINI data). Among patients who reported no days with thoughts of death or self-harm on the PHQ-9, the vast majority reported no SI (132/177, 75 %) or passive SI (31/177, 18 %) on the MINI. Overall, 15.5 % of the enrolled subjects were categorized as having SI with a moderate or high risk for completion at the time of enrollment. However, 6 % reported active SI with moderate or high risk of completion. Active, moderate to high risk SI on the MINI increased to 17.8 % (n = 13/73) if SI was reported “several days” on the PHQ-9, 42 % (n = 17/41) if SI was reported on “more than half the days” and 50 % (n = 6/12) if SI was reported “nearly every day”. Increasing frequency of suicidal thoughts on the PHQ-9 was associated with an increased frequency that the suicidal thoughts were active rather than passive when assessed in more detail on the MINI.
Prevalence ratios were estimated for the association between reports of any suicidality and specific demographic and clinical characteristics (Table 5). In the screened population, a history of a mood disorder was strongly predictive of SI. This association was not assessed in the enrolled population since by definition all participants had confirmed major depressive disorder. Gender and CD4 count were not associated with reports of suicidality but age appeared protective. Time since HIV diagnosis of less than 3 years and having a baseline HIV RNA over 50 copies/ml were both associated with SI. These characteristics are consistent with individuals who are not in consistent long-term care because of a recent diagnosis or poor engagement in care. SI was associated with the total PHQ-9 score, the affective symptom score, the somatic symptom score and a history of hazardous alcohol or current substance use (excluding marijuana). Among the study participants, age continued to be protective. Only an HIV diagnosis of less than 3 years and the scores of the three measures of depression were associated with increased SI. Except for the association with recent HIV diagnosis, similar findings were seen when considering active SI rather than any SI as the endpoint.
Discussion
In the results reported here, SI was reported somewhat less frequently (8.6 %) than reported by prior studies [7, 23]. This is consistent with the expectation that improvements in HIV treatment in the post-ART era have led to reductions in depression and SI through improved quality of life. Heterosexual exposure to HIV is more likely to be reported by PLWH in the southeastern US, including the locations of our study. Lower numbers of men who have sex with men (MSM) may explain our lower prevalence of SI, as MSM may experience stigma related to sexual identity as an additional trigger for depression and SI. Additionally, other unique southeastern US or African-American cultural factors may influence the prevalence of suicidal ideation. It is most likely that each of these factors contributes to the over-all lower prevalence of SI but these factors are beyond the scope of this study and warrant further study. While prevalence has decreased, this study found SI to be prevalent in PLWH receiving care in academic medical clinics in the southeastern US.
The PHQ-9 has been validated using the MINI in a variety of settings in the US and overseas [36, 39, 40]. Reports of SI on the PHQ-9 are a known risk for suicide attempts and completion [41]. In the screening program reported here, some moderate to high risk active SI was observed even among those reporting no thoughts of death or self-harm on the PHQ-9. Discrepancies between the two assessments may be due to a number of factors. The two assessments use different time frames so some variation may have occurred as a result. Patients may also differ in the willingness to report SI more ‘anonymously’ by pencil and paper (PHQ-9) versus a clinical interview (MINI) [42]. It is also possible that patients may not reveal this information until a clinician develops rapport and probes for SI. Finally, the clinical interviews were not always conducted on the same day as the PHQ-9 screening, but 89 % were completed within 24 h and all were completed within 2 weeks.
It is not known what SI screening score should be used for triggering a structured intervention. Previous recommendations for urgent intervention were limited to those who report SI almost every day [23]. The need for a clinical intervention for patients reporting SI must be balanced against the cost of the resources needed for the intervention and any disruption to the original purpose of the medical visit. The frequency of low-risk SI does not allow for a full psychiatric interview for every report of SI in medical clinics. This challenge has been described in the oncology literature where depression is a complication of a cancer diagnoses [42, 43]. The SI response plan at the site with the highest rate of SI during screening required the HIV provider to make an assessment of SI completion risk and involve the clinic social worker in arranging further care if needed. The threshold for this response was any report of SI, including “several days”, and the providers and staff were initially overwhelmed by the number of patients needing an intervention. The duration of SI is associated with increased risk of completion but even when experienced inconsistently, SI may be a clinically meaningful symptom. When SI was only reported “several days” in the last 2 weeks, more than one in six patients reported moderate to high risk SI. The prevalence of SI with moderate to high risk of completion increased with the frequency with which the thoughts occurred. Active, high risk SI was reported by nearly half of the participants who reported SI on more than half the days on the PHQ-9. Importantly, reporting SI “more than half the days” and “nearly every day” had similar frequencies of active moderate-high risk SI when interviewed. An immediate intervention is recommended based on moderate and high levels of risk for suicide completion. Since similar frequencies of moderate and high risk SI are present in the “more than half the days” and “almost every day” PHQ-9 categories, a similar level of healthcare response is indicated. Our findings suggest that both groups should be the target of urgent interventions and all reports require further evaluation.
In addressing SI in the clinic, patient characteristics that might increase the risk for SI are important to understand. The characteristics that were most associated with SI other than depressive symptoms were having a diagnosis of HIV for less than 3 years and having a detectable viral load. It is important to note that these are characteristics of individuals who are not in long-term consistent care. Individuals who are in long-term consistent care have almost always achieved viral load suppression. Thus, PLWH with detectable viral loads are not receiving effective care (or not long enough). It is also possible that patients with depression, have received some depression treatment if they are in HIV care. The opposite is true if a person is not in care. While screening for mental illness is becoming more common at the time of HIV diagnosis, including a formal assessment of depression may also be helpful when addressing PLWH who have high viral loads or who are returning to clinic after a lapse in care.
Implementation of depression screening as a component of HIV care requires some level of comfort with suicide assessments by medical providers, even when clinical behavioral health staff are available. Routine screening forced HIV providers to confront the prevalence of SI and precipitated many questions regarding further assessment. These questions were addressed using a structured SI triage algorithm and additional training. Baseline training included the use of the antidepressant medication algorithm and the availability of immediate psychiatry backup for questions regarding management of medications, side effects, and SI were outlined. Providers at the site with the highest rate of SI (>20 %) requested a second training and a response algorithm was developed. The study psychiatrist reviewed suicide symptomatology, identification of risks, and appropriate responses. Afterwards, providers were able to identify passive and low risk SI with sufficient comfort to allow screening to be included in routine care. The burden on medical clinics when implementing routine depression screening must be included in any implementation strategy. Addressing this with several trainings by a collaborating psychiatrist and a standardized SI triage algorithm may make implementation of screening possible in locations where immediate psychiatric care is not present.
These findings have several limitations. While the PHQ-9 is a versatile and widely used instrument, it has been demonstrated to behave differently with black and white Americans and other populations [44, 45]. The results of the MINI and the PHQ-9 are from clinics located in the southeastern US, and the populations in these clinics are predominantly African-American. The findings may not be applicable to PLWH in other parts of the US or the world. Second, screening was performed as a routine part of clinical care, so PLWH who are not engaged in medical care are not represented in this study. A third limitation to consider is the complexity of suicidal thoughts and ideation. A meta-analysis by Catalan et al. makes it clear that this is a multi-dimensional symptom and identifies the use of thoughts, ideation, and plans to describe concepts of SI. The articles cited in this meta-analysis describe the concepts of suicidal thoughts, ideation and plans using 20 or more methods [7]. While we acknowledge the importance of understanding the multiple dimensions of SI, the conceptual and measurement complexities prevented this issue from being addressed by the screening program. Despite those limitations, these data were collected at multiple sites and represent PLWH in the southeastern US where the burden of HIV is the greatest. In addition, it documents a successful strategy for addressing an important comorbid condition in PLWH.
In conclusion, despite the availability of effective ART and the possibility of a normal life span, SI remains a problem of importance in PLWH. As such, there is a continued need for screening and integrated interventions. Suicide assessment training should be built into the training and implementation practices for the expansion of depression management into primary care (including HIV primary care). Unlike prior recommendations, these findings suggest that immediate actions should be taken for patients reporting SI on more than half of the days in a 2-week time span. The association of SI with high viral loads suggests the importance of screening for depression when patients are entering care, re-engaging in care or failing to achieve viral load suppression. Unanswered questions remain regarding the character of SI and its impact on self-care and management of HIV among PLWH. Despite the fact that HIV has improved morbidity and mortality, the findings suggest that SI remains a significant comorbid problem for PLWH, especially for those who have recently begun to engage or re-engage in care.
References
Kessler RC, Borges G, Walters EE. Prevalence of and risk factors for lifetime suicide attempts in the National Comorbidity Survey. Arch Gen Psychiatry. 1999;56(7):617–26.
Szanto K, Reynolds CF, Frank E, Stack J, Fasiczka AL, Miller M, et al. Suicide in elderly depressed patients: is active vs. passive suicidal ideation a clinically valid distinction? Am J Geriatr Psychiatry. 1996;4:197–207.
Druss B, Pincus HA. Suicidal ideation and suicide attempts in general medical illnesses. Arch Intern Med. 2000;160:1522–6.
Hirschfeld RMA, Russell JM. Assessment and treatment of suicidal patients. N Engl J Med. 1997;337:910–5.
Marzuk PM, Tierney T, Tardiff K, Gross EM, Morgan EB, Hsu M-A, et al. Increased risk of suicide in persons with AIDS. JAMA. 1988;259:1333–7.
Cote TR, Biggar RJ, Dannenberg AL. Risk of suicide among persons with AIDS. JAMA. 1992;268(15):2066–8.
Catalan J, Harding R, Sibley E, Clucas C, Croome N, Sherr L. HIV infection and mental health: suicidal behaviour—systematic review. Psychol Health Med. 2011;16(5):588–611.
Carrico AW. Elevated suicide rate among HIV-positive persons despite benefits of antiretroviral therapy: implications for a stress and coping model of suicide. Am J Psychiatry. 2010;167(2):117–9.
Keiser O, Spoerri A, Brinkhof MW, Hasse B, Gayet-Ageron A, Tissot F, et al. Suicide in HIV-infected individuals and the general population in Switzerland, 1988-2008. Am J Psychiatry. 2010;167(2):143–50.
Schwarcz SK, Vu A, Hsu LC, Hessol NA. Changes in causes of death among persons with AIDS: San Francisco, California, 1996-2011. AIDS Patient Care STDs. 2014;28(10):517–23.
Hanson KE, Mansergh G, Koblin BA, Flores SA, Hudson SM, Myers L, et al. Depressive symptoms by HIV serostatus are differentially associated with unprotected receptive and insertive anal sex among substance-using men who have sex with men in the United States. J Acquir Immune Defic Syndr. 2014;68:e13–5.
McFall AM, Dowdy DW, Zelaya CE, Murphy K, Wilson TE, Young MA, et al. Understanding the disparity: predictors of virologic failure in women using highly active antiretroviral therapy vary by race and/or ethnicity. J Acquir Immune Defic Syndr. 2013;64(3):289–98.
Heckman TG, Miller J, Kochman A, Kalichman SC, Carlson B, Silverthorn M. Thoughts of suicide among HIV-infected rural persons enrolled in a telephone-delivered mental health intervention. Ann Behav Med. 2002;24(2):141–8.
Kalichman SC, Heckman T, Kochman A, Sikkema K, Bergholte J. Depression and thoughts of suicide among middle-aged and older persons living with HIV-AIDS. Psychiatr Serv. 2000;51(7):903–7.
Badiee J, Moore DJ, Atkinson JH, Vaida F, Gerard M, Duarte NA, et al. Lifetime suicidal ideation and attempt are common among HIV+ individuals. J Affect Disord. 2012;136(3):993–9.
Jia CX, Mehlum L, Qin P. AIDS/HIV infection, comorbid psychiatric illness, and risk for subsequent suicide: a nationwide register linkage study. J Clin Psychiatry. 2012;73(10):1315–21.
Rice BD, Smith RD, Delpech VC. HIV infection and suicide in the era of HAART in England, Wales and Northern Ireland. AIDS. 2010;24(11):1795–7.
Tektonidou MG, Dasgupta A, Ward MM. Suicidal ideation among adults with arthritis: prevalence and subgroups at highest risk. Data from the 2007-2008 National Health and Nutrition Examination Survey. Arthritis Care Res (Hoboken). 2011;63(9):1322–33.
Cheatle MD, Wasser T, Foster C, Olugbodi A, Bryan J. Prevalence of suicidal ideation in patients with chronic non-cancer pain referred to a behaviorally based pain program. Pain Physician. 2014;17(3):E359–67.
Dickstein LP, Viguera AC, Nowacki AS, Thompson NR, Griffith SD, Baldessarini RJ, et al. Thoughts of death and self-harm in patients with epilepsy or multiple sclerosis in a tertiary care center. Psychosomatics. 2015;56(1):44–51.
Pompili M, Forte A, Lester D, Erbuto D, Rovedi F, Innamorati M, et al. Suicide risk in type 1 diabetes mellitus: a systematic review. J Psychosom Res. 2014;76(5):352–60.
Sherr L, Lampe F, Fisher M, Arthur G, Anderson J, Zetlerd S, et al. Suicidal ideation in UK HIV clinic attenders. AIDS. 2008;22:1651–8.
Lawrence ST, Willig JH, Crane HM, Ye J, Aban I, Lober W, et al. Routine, self-administered, touch-screen, computer-based suicidal ideation assessment linked to automated response team notification in an HIV primary care setting. Clin Infect Dis. 2010;50(8):1165–73.
Schumacher JE, McCullumsmith C, Mugavero MJ, Ingle-Pang PE, Raper JL, Willig JH, et al. Routine depression screening in an HIV clinic cohort identifies patients with complex psychiatric co-morbidities who show significant response to treatment. AIDS Behav. 2013;17(8):2781–91.
Mirza RA, Eick-Cost A, Otto JL. The risk of mental health disorders among US military personnel infected with human immunodeficiency virus, active component, US Armed Forces 2000-2011. MSMR. 2012;19(5):10–3.
Govender RD, Schlebusch L. Suicidal ideation in seropositive patients seen at a South African HIV voluntary counselling and testing clinic. Afr J Psychiatry (Johannesbg). 2012;15(2):94–8.
Edwards M, Quinlivan EB, Bess K, Gaynes BN, Heine A, Zinski A, et al. Implementation of PHQ-9 depression screening for HIV-infected patients in a real-world setting. J Assoc Nurses AIDS Care. 2014;25(3):243–52.
Kozak MS, Mugavero MJ, Ye J, Aban I, Lawrence ST, Nevin CR, et al. Patient reported outcomes in routine care: advancing data capture for HIV cohort research. Clin Infect Dis. 2012;54(1):141–7.
Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–13.
Krause JS, Reed KS, McArdle JJ. Factor structure and predictive validity of somatic and nonsomatic symptoms from the patient health questionnaire-9: a longitudinal study after spinal cord injury. Arch Phys Med Rehabil. 2010;91(8):1218–24.
Yoon JC, Crane PK, Ciechanowski PS, Harrington RD, Kitahata MM, Crane HM. Somatic symptoms and the association between hepatitis C infection and depression in HIV-infected patients. AIDS Care. 2011;23(10):1208–18.
Rathore JS, Jehi LE, Fan Y, Patel SI, Foldvary-Schaefer N, Ramirez MJ, et al. Validation of the Patient Health Questionnaire-9 (PHQ-9) for depression screening in adults with epilepsy. Epilepsy Behav. 2014;37:215–20.
de Jonge P, Mangano D, Whooley MA. Differential association of cognitive and somatic depressive symptoms with heart rate variability in patients with stable coronary heart disease: findings from the Heart and Soul Study. Psychosom Med. 2007;69(8):735–9.
Smolderen KG, Spertus JA, Reid KJ, Buchanan DM, Krumholz HM, Denollet J, et al. The association of cognitive and somatic depressive symptoms with depression recognition and outcomes after myocardial infarction. Circ Cardiovasc Qual Outcomes. 2009;2(4):328–37.
Pence BW, Gaynes BN, Adams JL, Thielman NM, Heine AD, Mugavero MJ, et al. The effect of antidepressant treatment on HIV and depression outcomes: The SLAM DUNC randomized trial. AIDS. 2015;29:1975–86.
O’Connor E, Gaynes BN, Burda BU, Soh C, Whitlock EP. Screening for and treatment of suicide risk relevant to primary care: a systematic review for the US preventive services task force. Ann Intern Med. 2013;158:741–54.
Quinlivan EB, Messer LC, Adimora AA, Roytburd K, Bowditch N, Parnell H, et al. Experiences with HIV testing, entry, and engagement in care by HIV-infected women of color, and the need for autonomy, competency, and relatedness. AIDS Patient Care STDs. 2013;27(7):408–15.
Christopoulos KA, Massey AD, Lopez AM, Geng EH, Johnson MO, Pilcher CD, et al. “Taking a half day at a time:” patient perspectives and the HIV engagement in care continuum. AIDS Patient Care STDs. 2013;27(4):223–30.
Cholera R, Gaynes BN, Pence BW, Bassett J, Qangule N, Macphail C, et al. Validity of the Patient Health Questionnaire-9 to screen for depression in a high-HIV burden primary healthcare clinic in Johannesburg, South Africa. J Affect Disord. 2014;167:160–6.
Pence BW, Gaynes BN, Atashili J, O’Donnell JK, Kats D, Whetten K, et al. Feasibility, safety, acceptability, and preliminary efficacy of measurement-based care depression treatment for HIV patients in Bamenda, Cameroon. AIDS Behav. 2014;18(6):1142–51.
Simon GE, Rutter CM, Peterson D, Oliver M, Whiteside U, Operskalski B, et al. Does response on the PHQ-9 depression questionnaire predict subsequent suicide attempt or suicide death? Psychiatr Serv. 2013;64(12):1195–202.
Walker J, Hansen CH, Hodges L, Thekkumpurath P, O’Connor M, Sharma N, et al. Screening for suicidality in cancer patients using Item 9 of the nine-item patient health questionnaire; does the item score predict who requires further assessment? Gen Hosp Psychiatry. 2010;32(2):218–20.
Walker J, Waters RA, Murray G, Swanson H, Hibberd CJ, Rush RW, et al. Better off dead: suicidal thoughts in cancer patients. J Clin Oncol. 2008;26(29):4725–30.
Crane PK, Gibbons LE, Willig JH, Mugavero MJ, Lawrence ST, Schumacher JE, et al. Measuring depression levels in HIV-infected patients as part of routine clinical care using the nine-item Patient Health Questionnaire (PHQ-9). AIDS Care. 2010;22(7):874–85.
Huang FY, Chung H, Kroenke K, Delucchi KL, Spitzer RL. Using the Patient Health Questionnaire-9 to measure depression among racially and ethnically diverse primary care patients. J Gen Intern Med. 2006;21(6):547–52.
Acknowledgments
The authors acknowledge the clinic staff, providers, and patients for their invaluable contributions to this research.
Funding
This research was supported by funds from NIMH, NINR (R01MH086362); the Centers for AIDS Research at the University of North Carolina at Chapel Hill (P30-AI50410), Duke University (P30-AI064518) and the University of Alabama at Birmingham (P30-AI027767); and the National Center for Advancing Translational Sciences (NCATS), National Institutes of Health, through Grant Award Number 1UL1TR001111. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
None of the authors have conflict of interest to report.
Ethical Approval for Human Subjects
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Ethical Approval for Animal Research
This article does not contain any studies with animals performed by any of the authors.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Quinlivan, E.B., Gaynes, B.N., Lee, J.S. et al. Suicidal Ideation is Associated with Limited Engagement in HIV Care. AIDS Behav 21, 1699–1708 (2017). https://doi.org/10.1007/s10461-016-1469-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-016-1469-8