Abstract
Armed conflict is frequently assumed to be a contributor to the global HIV epidemic, but existing evidence is sparse. We examined the relationship between armed conflict between 2002 and 2008 and HIV disability life years (DALYs) in 2010 among WHO Member States. Using partial least squares analysis we also examined moderation of the armed conflict-HIV link by two susceptibility constructs (background risk, substance use) and one vulnerability mediator (numbers of refugees, people on ART, and total HIV spending). Background risk directly impacted HIV DALYs (p < 0.05), substance use moderated the conflict-HIV relationship (p < 0.01). The vulnerability construct mediated the conflict-HIV association (p < 0.01). Findings underscore the need to align HIV prevention/intervention efforts with pre-existing HIV burden and reduce the impact of natural disasters on the populace in conflict-affected states. Integration of substance prevention/harm reduction programs within national HIV responses, attention to most-at-risk populations and increased surveillance/treatment of drug resistant HIV and TB is warranted.
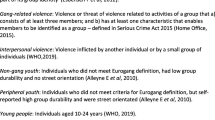
Similar content being viewed by others
Introduction
Background
Human immunodeficiency virus (HIV) remains a global public health crisis, claiming over 39 million deaths to date [1]. In 1990, HIV was ranked as 33rd among causes of morbidity and mortality combined worldwide; by 2010, it was ranked 5th, a 353 % increase [2]. At the end of 2013, approximately 35 million people were living with HIV, with 2.1 million newly infected each year [1].
Armed conflict is frequently assumed to be a contributor to the global HIV epidemic [3–5], but empirical support for that link is sparse. A study of 43 Sub-Saharan African countries from 1997 to 2005 found strong positive associations between civil war and HIV prevalence [6]. However, three other studies either found no association between conflict and HIV prevalence, controlling for economic factors [7], or that evidence was insufficient that HIV transmission increases in such settings [8, 9]. One reasonable interpretation of this literature is that conflict does not inevitably lead to increased HIV prevalence, but rather could be better understood as a risk factor whose effect might be moderated or mediated by other variables in a causal nexus.
Consistent with this view, a number of explanations have been offered to explain the link (e.g., conflict-induced migration, changes in sexual behavior) [3, 5, 8]. Nevertheless, the validity of these explanations is far from clear [10], and they do not explain why some conflict-affected populations but not others experience increased HIV morbidity and mortality. As research examining the conflict-HIV link matures, new theoretical models are needed to understand how and why conflict leads to HIV spread [11]. More importantly, the field needs to move beyond conventional multivariate risk factor analyses focusing on associations between variables to the identification of putative causal pathways through structural equation modeling.
Theoretical Model/Hypotheses
This study develops and tests a longitudinal explanatory model linking armed conflict occurring between 2002 and 2008 and its longer-term impact on HIV morbidity and mortality in 2010 among World Health Organization (WHO) Member States (Fig. 1). Conflict was defined as the number of deaths from civil war, terrorist actions and one-sided violence (e.g., genocide, summary execution of prisoners) that have increasingly characterized contemporary civil conflicts. HIV is represented by a country’s morbidity and mortality measured as disability-adjusted life years (DALYs) attributable to HIV. The model differentiates between pre-existing background or susceptibility factors from conflict-induced changes or vulnerability factors serving as indicators of processes through which conflict indirectly influences HIV spread. Susceptibility factors were conceptualized primarily as moderators, and vulnerability factors, as mediators, of the conflict-HIV relationship. Two susceptibility (moderator) constructs were created. A country’s baseline HIV prevalence, ethnic heterogeneity, and number of persons affected by natural disasters constituted the background susceptibility construct. These pre-existing factors all serve to increase a population’s susceptibility to HIV. The substance use susceptibility construct included per capita alcohol consumption and prevalences of illicit drug use and injection drug use (IDU). The one vulnerability (mediator) construct included three factors reflecting conflict-induced changes: a country’s number of refugees, asylum seekers and displaced persons, total HIV spending, and number of persons on antiretroviral treatment (ART).
Within this model, special emphasis was given to substance use as a susceptibility construct. Substance use, especially intravenous drug use (IDU), is important because an estimated 15.9 million persons worldwide inject illicit drugs. IDUs account for about 10 % of the estimated 27 million new HIV infections each year and 30 % of new infections outside Sub-Saharan Africa [1, 12]. Behaviors contributing to transmission include needle sharing and high-risk sexual behaviors. However, note that the tendency of policymakers and researchers to focus on the relationship between IDU and HIV has overshadowed the increased risk associated with alcohol use and non-IDU through high-risk sexual behaviors.
Understanding how armed conflict impacts longer-term HIV morbidity and mortality is critical in identifying conflict-affected populations at risk and in developing appropriate, evidence-based prevention and intervention approaches.
Pre-existing Background Susceptibility Factors as Independent Risk Factors for HIV or Moderators of the Conflict-HIV Association
The background susceptibility construct may directly increase HIV morbidity and mortality (i.e., as an independent risk factor), or, alternatively, interact with conflict to strengthen the conflict-HIV relationship as a moderator. Baseline prevalence of any health outcome often directly predicts future illness and death from the condition [10]. Alternatively, as a moderator of the conflict-HIV association, baseline prevalence may interact with conflict to increase longer-term HIV morbidity and mortality. That is, greater baseline prevalence may reflect a greater pool of infected persons that may strengthen the relationship between conflict and HIV morbidity and mortality [13, 14]. Similarly, within-country ethnic hetereogeneity can directly influence longer-term HIV morbidity and mortality through maldistribution of resources. That is, differences in ethnic, linguistic or religious composition can be major sources of political contention, often producing discrimination and unequal access to political power that translates into unequal access to health care [15, 16]. The greater the ethnic heterogeneity, the greater the adverse impacts on access to health care, including HIV prevention and intervention, among those discriminated against [17, 18]. Alternatively, ethnic heterogeneity, a common contributor to civil war, may moderate the conflict-HIV association through sexual violence towards women as a weapon of conflict, with associated increased risk of transmission [19–21].
Natural disasters and armed conflicts share many features and consequences and both have been classified as complex emergencies since the early 1990s [4] and more recently as “big events” [22, 23]. Natural disasters, like conflict, affect large civilian populations and are characterized by food and worker shortages, damage to healthcare facilities and other infrastructure, population displacements, violence toward women, and importantly, decreased access to contraceptive care and consequently prevention services for sexually-transmitted diseases [23]. Natural disasters have been linked directly to increased longer-term HIV morbidity and mortality. However, natural disasters can impact HIV morbidity and mortality by influencing conflict dynamics [24]. Natural disasters may moderate the armed conflict-HIV association since deadly disasters have increasingly occurred recently in countries with long-lasting conflict [25].
Taken together, the evidence and observations suggest the following alternative hypotheses:
H1A
Baseline HIV prevalence (in 2002), ethnic heterogeneity (2000), and number of people affected by natural disasters (2002–2008) directly increase longer-term HIV morbidity and mortality in 2010.
H1B
The conflict-HIV association is moderated by baseline prevalence, ethnic heterogeneity and number of people affected by natural disasters. The greater this background susceptibility, the greater the HIV-attributable morbidity and mortality.
Substance Use as a Moderator of the Conflict-HIV Association
Alcohol and illicit drug use, especially IDU, have been linked to HIV transmission through high-risk drug use and sexual behaviors [12, 26–30]. However, recent theoretical formulations [22, 23] also outline how substance use as a susceptibility factor interacts with armed conflict to influence longer-term HIV morbidity and mortality. These conditions include disruptions in economic and service provision processes and structures (including the drug trade) that influence social networks, gender and sexuality organization, norms and changes in HIV-related risk behavior. Taken together, these observations and theoretical formulations suggest that the substance use vulnerability construct may be a direct risk factor of HIV morbidity and mortality or serve as a moderator of the armed conflict-HIV association:
H2
The conflict-HIV association is moderated by alcohol and illicit drug use. The greater the level of substance use (in 2008, 2009) in the population, the greater the longer-term HIV morbidity and mortality in 2010.
Population Displacement, HIV Spending and ART Coverage as Mediators of the Conflict-HIV Association
Foremost among vulnerability factors that may mediate the conflict-HIV relationship is displacement of large populations. Numerous studies document relationships between conflict and refugees and highlight vulnerabilities among these populations to HIV reflecting family disintegration, poverty, social disruption leading to increased sexual risk behaviors, sexual violence, predatory sexual behavior and commercial sex [31–34].
The second vulnerability factor that may mediate the conflict-HIV association arises from destruction of health services and exacerbation of deficiencies in existing health infrastructures due to conflict [4, 5]. The capacity to deliver health services, including HIV prevention and intervention, is further eroded by shortages of equipment, medicine, and health care providers.
Assaults on a state’s healthcare service system resulting from conflict, and subsequent increases in HIV morbidity and mortality, attracts funding from regional and international agencies as well as non-governmental organizations. Increased spending on HIV, including ART, should reduce HIV morbidity and mortality. However, there are several reasons why an influx of resources may have led to increases in illness and death, especially during the years (2002–2010) of this study’s focus. First, HIV coordination and response in conflict-affected states remains incoherent and ad hoc, with response guidelines often vague and imprecise. Field staffs also lack the capacity and/or confidence to implement HIV guidelines. Moreover, coordination is among donors and humanitarian agencies, and integrated multiagency initiatives at the country-level, are sorely lacking [35]. Second, HIV morbidity and mortality might also increase despite increased spending and number of people on ART, especially in conflict-affected states, because of difficulty in reaching most-at-risk populations (MARPs). Many HIV epidemics in the last decade are concentrated among MARPs, specifically people who inject drugs, sex workers and men who have sex with men [36–38]. The preponderance of HIV spending in most countries with concentrated epidemics remain targeted to the general population [39], despite evidence of the effectiveness and low cost of prevention and treatment programs targeting MARPs.
Lastly, drug resistance may have slowed reductions in HIV morbidity and mortality anticipated by national HIV spending. Transmitted drug resistance occurs when previously uninfected individuals are infected with drug-resistant virus; acquired drug-resistance develops when mutations emerge among individuals receiving ART [40]. The prevalence of acquired HIV drug resistance in low-to-middle income countries increased from 3.6 to 6.6 % from 2003 to 2010, whereas in high-income countries, 80.1 % of individuals failing ART had at least one drug resistant mutation [41]. Between 2004–2006 and 2007–2010 in low-to-middle income countries, the percentage of 72 surveys reporting transmitted moderate drug resistance (5–10 %) increased from 18.2 to 32.0 %. In high-income countries, the prevalence of transmitted drug resistance was 7.7 % between 2004 and 2009. As ART coverage increases, greater drug resistance may hamper treatment effectiveness and slow reductions in HIV morbidity and mortality [40]. At the same time, tuberculosis (TB) drug resistance has increased worldwide, and this disproportionately affects people living with HIV/AIDS (PLWAs) [42]. TB is the most common presenting illness among PLWAs including those taking ART [42, 43] and also a leading health threat in conflict-affected states fueled by malnutrition, overcrowding and health service disruptions [44]. Recent increases in TB drug resistance, along with increases in HIV drug resistance may play a continuing role in increasing HIV morbidity and mortality despite increases in HIV prevention and intervention resources among PLWAs and in conflict-affected and resource limited settings.
Taken together, the aforementioned empirical evidence and observations suggest the following hypothesis:
H3
The conflict-HIV association is mediated by the number of refugees, asylum seekers and displaced persons (in 2008), total HIV spending (in 2008, 2009), and number of people on ART (in 2008).
Methods
Measures
Outcome: HIV Disability-Adjusted Life Years
The outcome variable was HIV-attributable DALYs in 2010 among WHO Member States for which data were available (n = 177). The DALY, a summary measure of health, combines information on morbidity and mortality for specific diseases including HIV. DALYs are derived as years of life lost to premature HIV-attributable mortality plus years of life lost to disability by people with HIV in a population [45]. Data on 2010 HIV DALYs were available from the Institute of Health Metrics and Evaluation’s Global Health Data Exchange [46].
Armed Conflict
The severity and scope of civil war increasingly includes terrorism and one-sided violence [47]. Between 1990 and 2004, almost all fatalities from one-sided violence have occurred in countries experiencing armed conflict and terrorism, suggesting that these three forms of intimately related violence can be combined to reflect changes in the characteristics of civil conflict [48]. Accordingly, conflict was operationalized as the sum of deaths from civil war, terrorism, and one-sided violence between 2002 and 2008.
Data for civil war deaths between 2002 and 2008 were derived from the 2014 update of the Uppsala Conflict Data Program’s Battle Deaths Database [48, 49]. Civil war is armed conflict between a state’s government and one or more internal opposition groups with or without intervention from other states. Armed conflict is contested incompatibility concerning governments and/or territory where the use of armed force between two parties, of which at least one is the state’s government, results in at least 25 battle deaths.
Data on the number of deaths among victims and perpetrators of terrorism from 2002 to 2008 were derived from the 2014 update of the Global Terrorism Database (GTD) [50]. Terrorist incidents are intentional, achieve violence and are perpetrated by sub-national, non-state actors. In addition, at least two of the following criteria must be met (1) the act must be aimed at a political, economic, religious, or social goal; (2) there is evidence of intention to coerce, intimidate, or convey another message to a larger audience than the immediate victims; and (3) the action must be outside the context of legitimate warfare activities [51].
Data on deaths resulting from one-sided violence from 2002 to 2008 were available from the Uppsala Conflict Data Program’s One-sided Violence Database [52]. One-sided violence is the use of armed force by a state’s government or a formally organized group against civilians resulting in at least 25 deaths. Only one-sided violence deaths perpetrated by government actors were included in these analyses since those perpetrated by formally organized groups were included in the GTD [53].
Using deaths from civil war, terrorism, and one-sided violence in the years 2002 to 2008 produces a 2-year lag to DALYs occurring in 2010. Thus, these are not deaths or disabilities experienced in earlier years when the civil war and related violence was active.
Pre-existing Background Susceptibility Factors
All background risk factors except number of people affected by disasters were measured as close to 2002 as available data allowed.
Baseline HIV prevalence data among 15- to-49-year-olds in 2002 were available from the UNAIDS Millennium Development Goals Database [54]. The measure of ethnic heterogeneity in this study, derived from Vanhanen [55], combines three indicators: racial, linguistic and religious division, each measured as the percentage of the largest group of a country’s population from 1994 to 1999. Data on these characteristics within countries have remained relatively stable over the years examined in this study. The inverse of these three percentages are summed to measure the degree of ethnic heterogeneity.
The natural disaster measure combined the numbers of persons confirmed dead or missing, persons needing immediate shelter, and persons affected (requiring immediate assistance in basic survival needs, e.g., food, water and sanitation), in thousands, for 2002–2008. Data were available from the Emergency Events Database maintained by the Center for Research on Epidemiology and Disasters (CRED) [56]. A disaster event defined by CRED meets one or more of the following criteria: (1) at least 10 people were killed; (2) at least 100 people were affected; or (3) the disaster led to the declaration of a state of emergency or calls for international assistance.
Substance Use Susceptibility Factors
Per capita alcohol consumption was measured as total recorded consumption in liters of pure alcohol, computed as the sum of total production and imports, less exports, divided by the population aged 15 and older. Country-level data for either 2007 or 2008 were available from the WHO Global Health Observatory Database [57].
Illicit drug use was defined as non-medical use of drugs prohibited by international law. The illicit drug use measure was the sum of the annual prevalences of illicit use of cannabis, opiates and cocaine for various years between 2002 and 2009 expressed as percentages of the population aged 15 years and older [58]. Data on illicit drug use were derived from the United Nations Global Illicit Drug Trends Report [58, 59] Country-level prevalence estimates among 15- to 64-year-olds of IDU were also available from this source for various years between 2002 through 2009.
Vulnerability Factors
Number of refugees/asylum seekers/displaced persons (in thousands) residing in each host country at the end of 2008 were available from the UN High Commissioner for Refugees Statistical Database [60].
Data on total HIV spending in 2008 or 2009 and the number of persons on ART in 2008 were available from the United Nations UNAIDS Data [61]. Total spending included all domestic, public and international spending on HIV programs.
Statistical Analyses
To analyze the measurement and structural models, partial least squares structural equation modeling (PLS-SEM) utilized SmartPLS Version 2.0 [62]. This methodology is an alternative to covariance fitting approaches [63] and is component-based. PLS-SEM is more suitable for theory building, as in this study, whereas covariance-based SEM is more suitable for theory testing [64]. PLS-SEM combines the predictive approach of classical multivariate techniques to examine dependency relationships with the psychometric approach based on measurement of latent (non-observed) variables. PLS-SEM is an optimal fit to the data profile of this study, that is, small sample size (n < 200 countries) with constructs defined by multiple indicators [64].
The PLS-SEM method does not require multivariate normality to produce consistent parameters, but rather uses bootstrap resampling to test stability of estimates. The bootstrap procedure draws repeated random samples (in this case, 5000) from the data to estimate standard errors and calculate t-statistics for inferential purposes [65]. Bootstrapping is a powerful and accurate method for detecting moderating and mediating effects [66, 67].
PLS-SEM methodology adopts a two-step approach. The first step focuses on the measurement model to analyze reliability and validity of the indicator variables and constructs. In the second step, structural model assessment provides empirical evidence to suggest the theoretical model and hypotheses through examination of dependency relationships among the constructs [64].
PLS-SEM examines the direct effect of conflict on HIV DALYs and the moderating effects of the pre-existing background and substance use constructs (the former which might alternatively have a direct longer-term effect on HIV DALYs). Moderation is tested by examining the significance of the interaction between conflict and the susceptibility construct [63]. The mediation effect can be tested by observing significant path coefficients from conflict to vulnerability and from vulnerability to HIV DALYs (with no significant path from conflict to DALYs) [64]. The indicators examined herein were reflective, that is, the indicators were viewed as manifestations or expressions of their respective constructs. All indicators were standardized, centered and, except for ethnic heterogeneity, log transformed.
Results
Measurement Model: Reliability and Validity
While individual indicator reliability is optimal when standardized loadings of the indicators are at least 0.70, loadings greater than 0.50 are acceptable in initial stages of research, as is the case here [66, 68, 69]. Indicator loadings, with four exceptions (0.52–0.68), well exceeded the 0.70 benchmark.
For construct reliability, we examined composite reliability. Nunnally [70] suggests 0.70 as a reliability benchmark. All constructs showed adequate internal consistency (0.74–0.89) (Table 1).
Convergent validity was assessed with the average variance extracted (AVE), which should exceed 0.50 [68, 71, 72]. All constructs satisfy this condition (AVE 0.50–0.76) (Table 1). For discriminant validity, the AVE should exceed the variance shared between the latent construct and other model constructs (i.e., squared correlation between constructs). The square root of each constructs’ AVE (on the diagonal) is larger than its correlation with other constructs (Table 1), suggesting sufficient discriminant validity.
Sufficient convergent and discriminant validity can also be shown by higher indicator loadings on hypothesized constructs than on others [64]. All items met this condition (Table 2). In only three instances was there evidence of cross-loading: number of people on ART cross-loaded on background susceptibility and baseline HIV prevalence and number of people affected by natural disasters cross-loaded with vulnerability. However, in no instance did these cross-loadings exceed the loading of the indicator on its specified construct, further suggesting sufficient discriminant and convergent validity.
Structural Model
Structural model results are shown in Fig. 2. Individual path coefficients can be interpreted as standardized coefficients of ordinary least squares regression [64]. The pre-existing background construct did not moderate the conflict-HIV relationship (β = 0.065, t = 0.734, p > 0.05) but positively and directly affected DALYs (β = 0.410, t = 6.51, p < 0.01). Conversely, substance use moderated the conflict-HIV association (β = 0.114, t = 1.74, p < 0.05). The vulnerability construct mediated the conflict-HIV association demonstrating positive, significant relationships between conflict and vulnerability (β = 0.427, t = 6.62, p < 0.01) and between vulnerability and HIV DALYs (β = 0.476, t = 8.650, p < 0.01), while the conflict-HIV DALY relationship was not significant. Further, the full mediation model explains more variance in the outcome variables (R2 included 0.771) than the model without vulnerability (R2 excluded 0.765). The magnitude of the mediation effect f2 = (R2 included—R2 excluded/1-R2 included) was moderate (0.0262) [67].
The proportion of variance in 2010 HIV DALYs explained by the model was 0.771. Overall model quality, assessed with Goodness of Fit (GoF [73], the geometric mean of the average communality and average R2, was 0.585, indicating good fit.
Discussion
This study found that armed conflict did not have a direct effect on HIV morbidity and mortality, but rather exerted its effect on HIV DALYs through mediation and moderation by other HIV risk factors. This study also found that pre-existing background susceptibility factors did directly affect longer-term HIV morbidity and mortality. Baseline (2002) HIV prevalence increased HIV DALYs in 2010. That baseline prevalence does not intensify the adversities of conflict to increase morbidity and mortality (i.e., serve as a moderator of the conflict-HIV association) does not diminish its importance as an independent HIV risk factor. This finding suggests that HIV resources be directed to higher HIV burden countries to preempt increased longer-term morbidity and mortality. This investment should be directed toward all such countries, but is particularly important in conflict-prone, fragile states.
As hypothesized, ethnic heterogeneity also directly influenced morbidity and mortality [15, 16]. This finding suggests that discrimination and unequal access to political power among minorities may translate into unequal access to health care, including HIV prevention and treatment. The absence of moderation of the conflict-HIV association by ethnic-heterogeneity does not support the hypothesis that the conflict-HIV association is exacerbated by ethnic-heterogeneity through sexual violence. This finding highlights the need for increased political will to address ethnic grievances, no matter how deeply entrenched.
The number of people adversely affected by natural disasters also directly increased HIV DALYs. This finding is consistent with prior literature [22, 23] linking natural disasters to increased HIV morbidity and mortality through food and water shortages, damage to health and other infrastructures, population displacement, and decreased access to health care, including sexual health services. Natural disasters did not moderate the conflict-HIV association, suggesting that they do not affect the dynamics of conflict in ways that increase susceptibility to HIV. However, relationships between natural disasters and conflict may be more complex than reflected here. For example, factors found to influence states’ conflict propensities, such as poverty, weak political institutions, and high populations may also influence disaster resilience suggesting that each phenomenon increases propensity for the other. Further study on the relationship of natural disasters and conflict in relationship to HIV morbidity and mortality is warranted as deadly disasters have increasingly occurred in countries with longstanding conflicts.
As hypothesized, alcohol consumption, illicit drug use, and IDU moderated the conflict-HIV relationship: the greater the rate of substance use, the stronger the conflict-HIV association. It appears that conditions of conflict, arising from displacement, grief and fear, social isolation, changes in sexuality and HIV-related risk behaviors in the presence of high substance use increases the susceptibility of a population to HIV [22, 23].
Substance use is a potentially modifiable risk factor that interacts with conflict to increase longer-term HIV morbidity and mortality. Thus, approaches including brief interventions targeting high-risk substance users, provisions for injection equipment, condom distribution, and education, screening, diagnosis and treatment of other sexually transmitted disease, viral hepatitis and TB, are warranted in conflict-affected states [74]. Among these and other resource-limited settings, establishing 12-step support groups may be a cost-effective first step for the long-term stability of substance using populations [75].
Recent recommendations have focused on scaling up integration of substance use interventions within programs and allocations associated with HIV response [74]. This study’s findings further support greater investment in substance prevention and harm reduction among users in conflict-affected countries where current investment is disproportionate to disease burden.
The combined manifest vulnerability factors of number of refugees, total HIV spending, and number of people on ART mediated the conflict-HIV association. The magnitude of displaced persons in a population, rarely studied as a mediator of the conflict-HIV relationship, may explain the ambiguity in studies examining direct conflict-HIV associations among displaced populations. The mediating effect of number of refugees, asylum seekers, and displaced persons on the conflict-HIV association underscores the need of HIV prevention and intervention in these populations to reduce longer-term morbidity and mortality.
Total HIV spending, and number of people on ART were also identified as vulnerability indicators that mediated the conflict-HIV relationship. Several potentially explanatory underlying processes, including lack of coordination [34] and imprecise guidelines [35] for HIV response, and difficulties in reaching MARPs [36–38], importantly suggest interventions for decreasing morbidity and mortality. Foremost, a concentrated effort is needed to strengthen HIV response guidelines and coordinate and integrate response among multi-agency initiatives, especially among conflict-affected states. Within this context, the HIV response must address the special needs of MARPs, despite difficulties in reaching and treating these populations.
Conflict was positively associated with spending and number of people on ART, which in turn was positively associated with HIV DALYs. HIV and TB drug resistance [42–44] were hypothesized to contribute to processes underlying vulnerability to HIV that mediate the conflict-HIV association (along with the number of persons displaced by conflict). Recent WHO reports have highlighted the need for surveillance/surveys of transmitted and acquired drug resistance, especially in ART-treated populations. More resources in the global HIV response should be directed to screening, diagnosis, and treatment of HIV and TB drug resistance, monitoring early indicators of resistance and integrating HIV and TB prevention and intervention. These urgent recommendations are even more critical for conflict-affected states where weakened public health infrastructure can destabilize ART programs and lead to treatment and supply chain interruptions, healthcare personnel and civilian displacement, destruction of homes, lack of necessities, and violent environments. Demoralization in conflict-affected populations may also lead to HIV and TB treatment non-adherence.
This study moved beyond conventional multivariate risk factor models to examine putative causal pathways between conflict and longer-term HIV morbidity and mortality using PLS-SEM. This study also combined deaths from civil wars, terrorism and one-sided violence in conflict-affected states, highlighting all three forms of violence as substantial public health problems. Substance use moderated the conflict-HIV association, providing preliminary evidence for the importance of these neglected factors in HIV spread.
Limitations include the potential for omitting important indicators from the models presented herein, but the associated R2s were very high, indicating reasonably complete specification of relevant influences. Although the ecological comparative design of this study cannot fully capture within-country variation, it can play an essential role in defining the impact of major public health problems like conflict that operate at a population level to influence HIV morbidity and mortality. The measures used in this study were also associated with variable reliability across WHO Member States. However, since the mid-1990s, efforts to increase the reliability of study variables have been unprecedented, including stringent inter-rater reliability standards [48, 75], increased reliability and coverage of indicator variables and advances in completeness and reliability of morbidity and mortality data underlying DALY estimates [2, 76, 77]. These measures are the most reliable that have ever been available, thereby permitting plausible, but tempered, systematic inferences of the longer-term influence of conflict on HIV morbidity and mortality.
In summary, armed conflict influenced longer-term HIV morbidity and mortality, largely by moderation by substance use and mediation through refugees, HIV spending, and the number of people on ART. Baseline HIV prevalence, ethnic heterogeneity, and number affected by disasters also directly influenced HIV DALYs. Future studies using SEM are needed to refine the present theoretical models and to identify the role of additional risk factors for HIV morbidity and mortality. Taken together, this research will form the evidence base to inform prevention and intervention programs in conflict-affected states. Importantly, these results underscore one of the hidden health costs of armed conflict, providing an additional rationale for promoting peace.
References
World Health Organization. HIV/AIDS. Geneva, Switzerland: World Health Organization.
Murray JLM, Vos T, Lozano R, et al. Disability-adjusted life years (DALYS) for 291 diseases and injuries in 21 regions, 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2197–223.
El-Bushra J. How should we understand violence and HIV/AIDS in conflict contexts. Washington D.C: AIDS and Conflict Initiative; 2012.
Levy BS, Sidel VW. Health effects of combat: a life course perspective. Annu Rev Public Health. 2009;30:123–36.
Levy BS, Sidel VW. War and public health. New York: Oxford University Press; 2007.
Iqbal Z, Zorn C. Violence conflict and spread of HIV/AIDS in Africa. J Pol. 2010;72:149–62.
Davenport C, Loyle CE. The conflict-HIV/AIDS nexus: an empirical assessment. New York: AIDS Security and Conflict Initiative; 2009.
Spiegel PB. HIV/AIDS among conflict-affected and displaced populations: dispelling myths and taking action. Disasters. 2007;28(3):322–39.
Spiegel PB, Bennedsen AR, Claas J, et al. Prevalence of HIV infection in conflict-affected and displaced persons in seven Sub-Saharan African countries: a systematic review. Lancet. 2007;369(9580):2187–95.
McInnes C. Conflict, HIV and AIDS: a new dynamic in warfare. Glob Change Peace Secur. 2009;21(1):99–114.
Mock NB, Duale S, Brown LF, Mathys E. Conflict and HIV: a framework for risk assessment to prevent HIV in conflict-affected settings in Africa. Emerg Themes Epidemiol. 2004;1(6):1–16.
World Bank. The global epidemics among people who use drugs. Washington, D.C.: World Bank; 2013.
McInnes C, Rushton S. HIV, AIDS and security: where are we now. Int Aff. 2010;86(1):225–45.
Hankins CA, Friedman SE, Zafar T, et al. Transmission and prevention of HIV and sexually transmitted infections in war settings: implications for current and future armed conflict. AIDS. 2002;16(17):2245–52.
Buhaug H, Cederman LE, Gleditsch KS. Square pegs in round holes: inequalities, grievances, and civil war. Int Stud Quart. 2014;58(2):418–31.
Denny EK, Walter BF. Ethnicity and civil war. J Peace Res. 2014;15(2):199–212.
Esteban J, Mayoral L, Ray D. Ethnicity and conflict. Science. 2012;336(6083):858–65.
Ghobarah HA, Huth P, Russett B. The post-war public health effects of civil conflict. Soc Sci Med. 2004;59(4):869–84.
Khaw AJ, Salama P, Burkholder B, Dondero TJ. HIV risk prevention in emergency-affected populations: a review. Disasters. 2000;24(3):181–97.
Mills EJ, Singh S, Nelson BD, et al. The impact of conflict on HIV/AIDS in Sub-Saharan Africa. Int J STD AIDS. 2006;17(11):713–7.
Shanks L, Schull MJ. Rape in war: the humanitarian response. Can Med Assoc J. 2000;163(9):1152–6.
Friedman S, Rossi D, Flom PL. “Big events” and networks. Connect. 2006;27(1):9–14.
Friedman SR, Rossi D, Braine N. Theorizing, “big events” as a potential risk environment for drug use, drug-related harm and HIV epidemic outbreaks. Int J Drug Policy. 2009;20(3):283–91.
Leaning J, Guha-Sapir D. Natural disasters, armed conflit and public health. New Engl J Med. 2013;369(19):1836–42.
United Nations Office for Coordination of Humanitarian Affairs. Natural and conflict related hazards in Asia-Pacific. Thailand: United Nationals Office for Coordination of Humanitarian Affairs; 2009.
Ezard N, Oppenheimer E, Burton A, et al. Six rapid assessments of alcohol and other substance use in populations displaced by conflict. Confl Health. 2011;5(1):1–15.
Kalichman SC, Simbaya C, Kaufman M, et al. Alcohol use and sexual risks for HIV/AIDS in sub-Saharan Africa: a systematic review of empirical findings. Prev Sci. 2007;8(2):141–51.
Strathdee SA, Stachowiak JA, Toss CS, et al. Complex emergencies, HIB, and substance use: no “big easy” solution. Subst Use Misuse. 2006;41:1637–51.
Weaver H, Roberts B. Drinking and displacement, a systematic review of the influence of forced displacement on harmful substance use. Subst Use Misuse. 2010;45(10–12):2340–55.
Woolf-King SE, Maisto SA. Alcohol use and high-risk sexual behavior in Sub-Saharan Africa: a narrative review. Arch Sex Behav. 2011;40(1):17–42.
Toole MJ. The public health aspects of complex emergencies and refugee situations. Annu Rev Public Health. 1997;18:283–312.
Toole MJ, Waldman RJ. 1993. Refugees and displaced persons. JAMA. 1993;270(5):600–5.
United Nations for Commissioner for Refugees. The state of the world’s refugees. England: Oxford, United Nations High Commissioner for Refugees; 2013.
Hanson BW, Wodak A, Fiamma A, et al. Refocusing and prioritizing HIV programmes in conflict and post conflict settings: funding recommendations. AIDS. 2008;22:S95–103.
Avdeeva O, Lazarus JV, Aziz MA, Atun R. The Global Fund’s resource allocation decisions for HIV programmes: addressing those in need. J Int AIDS Soc. 2011;2011(14):1–10.
Beyer C, Sullivan P, Sanchez J, et al. The increase in global HIV epidemics in MSM. AIDS. 2013;27(17):2665–78.
Mathers BM, Degenhardt L, Ali H, et al. HIV prevention treatment and care services for people who inject drugs: a systematic review of global, regional and national coverage. Lancet. 2010;375(9719):1014–29.
Strandee SA, Stockman JK. Epidemiology of HIV among injecting and non-injecting drug users: current trends and implications for intervention. Curr HIV AIDS Rep. 2010;7(2):99–106.
Craig AP, Thein HH, Zhang L, et al. Spending HIV resources in Asia and Eastern Europe: systematic review reveals need to shift funding allocations toward priority populations. J Int AIDS Soc. 2014;17:1–13.
World Health Organization. Surveillance of HIV drug resistance in adults initiating antiretroviral therapy (pretreatment HIV drug resistance). Geneva: World Health Organization; 2014.
World Health Organization. HIV drug resistance report. Geneva: World Health Organization; 2012.
World Health Organization. Global tuberculosis report, 2014. Geneva: World Health Organization; 2014.
World Health Organization. Priority research questions for TB/HIV in HIV-prevalent and resource-limited settings. Geneva: World Health Organization; 2010.
Kimbrough W, Saliba V, Dahab M, et al. The burden of tuberculosis in crisis-affected populations: a systematic review. Lancet. 2010;12(12):950–65.
Murray CJL, Lopez AD. The global burden of disease. Geneva: World Health Organization; 1996.
Institute of Health Metrics and Evaluation. Global Burden of Disease 2010 Global Health Data Exchange. Seattle: Institute of Health Metrics and Evaluation; 2013.
Eck K, Hultman L. One-sided violence against civilians in war: insights from new fatality data. J Peace Res. 2007;44(2):233–46.
Lacina B. Battle Deaths Dataset, Version 5.0. Oslo: Center for the Study of Civil War, International Peace Research; 2014.
Lacina B, Gleditsch NP. Monitoring trends in global combat: a new dataset of battle deaths. Eur J Popul. 2005;2005(21):145–66.
National Consortium for the Study of Terrorism and Response to Terrorism. Global Terrorism Database, 1970-2013. College Park: National Consortium for the Study of Terrorism and Response to Terrorism; 2014.
National Consortium for the Study of Terrorism and Response to Terrorism. Global Terrorism Database codebook, 1970-2013. College Park: National Consortium for the Study of Terrorism and Response to Terrorism; 2014.
Kreutz J, Eck K. One-sided violence dataset, 1984-2012. Uppsala: Uppsala Conflict Data Program; 2013.
Kreutz J, Eck K. One-sided violence codebook, version 1.4. Uppsala: Uppsala Conflict Data Program; 2013.
United Nations. UNAIDS Millennium Development Goals Database. New York: United Nations; 2014.
Vanhanen T. Domestic ethnic conflict and ethnic nepotism: a comparative analysis. J Peace Res. 1999;36(1):55–73.
Center for Research on Epidemiology and Disasters. Emergency Event Database. Geneva: Center for Research on Epidemiology and Disasters; 2014.
World Health Organization. Global Health Observatory Database. Geneva: World Health Organization; 2014.
United Nations Office on Drugs and Crime World Drug Report. Vienna. Austria: United Nations Office on Drugs and Crime; 2013. p. 2013.
United Nations Office on Drugs and Crime. Drug trends statistical database. Vienna: United Nations Office on Drugs and Crime; 2014.
United Nations High Commissioner for Refugees. Statistical database on refugees. Geneva: United Nationals High Commissioner for Refugees; 2013.
United Nations. UNAID database. New York: United Nations; 2014.
Ringle CM, Wende S, Will A. Smart PLS 2.0 [Computer Software]. www.smartpls.de; 2005.
Jöreskog, KG, Sörbom, D. LISREL 9.4 for Windows. Skokie: Scientific Software International, Inc.; 2014.
Vinzi VE, Chin WW, Henseler J, et al. Handbook of partial least squares. New York: Springer; 2010.
Hair JF, Hult GTM, Ringle CM, et al. A primer on partial least squares structural equation modeling (PLS-SEM). Washington D.C.: Sage; 2014.
Jose PE. Doing statistical mediation and moderation. New York: Guilford Press; 2013.
Chin WW. The partial least squares approach to structural equation modeling. In: Marcoulides GA, editor. Modern methods for business research. Mahwah: Lawrence Erlbaum Associates; 1998. p. 295–358.
Barclay D, Higgins C, Thompson R. The partial least squares approach (PLS) to causal modeling: personal computer adaptation and use as an illustration. Tech Stud. 1995;2(2):285–309.
Carmines EG, Zeller RA (eds.). Reliability and validity assessment. Sage university paper series on quantitative applications in the social sciences. Sage Publications, Beverly Hills, California; 1979.
Nunnally J. Psychometric theory. New York: McGraw Hill; 1978.
Werts CE, Linn RL, Joreskog KG. Interclass reliability estimates: testing structural assumptions. Educ Psychol Meas. 1974;34(1):25–33.
Fornell C, Larcker DF. Evaluating structural equation models with unobservable variables and measurement error. J Marketing Res. 1981;18(1):39–50.
Tenenhaus M, Vinzi VE, Chatelin YM, et al. PLS path modeling. Comp Stat Data Anal. 2005;48(1):159–205.
United Nations High Commissioner for Human Rights/World Health Organization. Rapid assessment of alcohol and other substance use in conflict-affected and displaced populations: a field guide. Geneva: United Nations High Commissioner for Human Rights/World Health Organization; 2008.
World Health Organization. Global status report on alcohol and health. Geneva: World Health Organization; 2011.
Kreutz K, Eck K. One-Sided Violence Deaths Database. Oslo: Department of Peace and Conflict Research; 2014.
Murray CJL, Ezzati M, Flaxman AD, et al. GBD 2010: design, definitions and metrics. Lancet. 2012;380(9859):2063–6.
Acknowledgments
This research was supported by the National Institute on Drug Abuse, National Institutes of Health (5F32DA0364431: Dr. Kerridge), the National Institute on Alcohol Abuse and Alcoholism (K05AA014223: Dr. Hasin), and the New York State Psychiatric Institute (Dr. Hasin).
Disclaimer
The views and opinions expressed in this report are those of the authors and should not be construed to represent the views of any of the sponsoring agencies of the government.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kerridge, B.T., Saha, T.D. & Hasin, D.S. Armed Conflict, Substance Use and HIV: A Global Analysis. AIDS Behav 20, 473–483 (2016). https://doi.org/10.1007/s10461-015-1161-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-015-1161-4