Abstract
Adherence to antiretroviral medications is usually expressed in terms of the proportion of doses taken. However, the timing of doses taken may also be an important dimension to overall adherence. Little is known about whether patients who mistime doses are also more likely to skip doses. Using data from the completed Adherence for Life randomized controlled trial, we created visual and statistical models to capture and analyze dose timing data collected longitudinally with electronic drug monitors (EDM). From scatter plots depicting dose time versus calendar date, we identified dominant patterns of dose taking and calculated key features [slope of line over calendar date; residual mean standard error (RMSE)]. Each was assessed for its ability to categorize subjects with ‘sub-optimal’ (<95 % of doses taken) using area under the receiver operating characteristic (AROC) curve analysis. Sixty eight subjects contributed EDM data, with ~300 to 400 observations/subject. While regression line slopes did not predict ‘sub-optimal’ adherence (AROC 0.51, 95 % CI 0.26–0.75), the variability in dose timing (RMSE) was strongly predictive (AROC 0.79, 95 % CI 0.62–0.97). Compared with the lowest quartile of RMSE (minimal dose time variability), each successive quartile roughly doubled the odds of ‘sub-optimal’ adherence (OR 2.1, 95 % CI 1.3–3.4). Patterns of dose timing and mistiming are strongly related to overall adherence behavior. Notably, individuals who skip doses are more likely to mistime doses, with the degree of risk positively correlated with the extent of dose timing variability.





Similar content being viewed by others
References
Liu H, Golin CE, Miller LG, Hays RD, Beck CK, Sanandaji S, et al. A comparison study of multiple measures of adherence to HIV protease inhibitors. Ann Intern Med. 2001;134(10):968–77.
Gross R, Bilker WB, Friedman HM, Strom BL. Effect of adherence to newly initiated antiretroviral therapy on plasma viral load. Aids. 2001;15(16):2109–17.
Wagner GJ. Predictors of antiretroviral adherence as measured by self-report, electronic monitoring, and medication diaries. AIDS Patient Care STDS. 2002;16(12):599–608.
Wilson IB, Tchetgen E, Spiegelman D. Patterns of adherence with antiretroviral medications: an examination of between-medication differences. J Acquir Immune Defic Syndr. 2001;28(3):259–63.
Knafl GJ, Bova CA, Fennie KP, O’Malley JP, Dieckhaus KD, Williams AB. An analysis of electronically monitored adherence to antiretroviral medications. AIDS Behav. 2010;14(4):755–68.
Knafl GJ, Fennie KP, Bova C, Dieckhaus K, Williams AB. Electronic monitoring device event modelling on an individual-subject basis using adaptive Poisson regression. Stat Med. 2004;23(5):783–801.
Ferguson NM, Donnelly CA, Hooper J, Ghani AC, Fraser C, Bartley LM, et al. Adherence to antiretroviral therapy and its impact on clinical outcome in HIV-infected patients. J R Soc Interface. 2005;2(4):349–63.
Wilson JQ, Kelling GL. Broken Windows: the police and neighborhood safety. Atlantic 1982.
Bachman Desilva M, Gifford AL, Keyi X, Li Z, Feng C, Brooks M, et al. Feasibility and acceptability of a real-time adherence device among HIV-positive IDU patients in China. AIDS Res Treat 2013;2013:957862.
Haberer JE, Robbins GK, Ybarra M, Monk A, Ragland K, Weiser SD, et al. Real-time electronic adherence monitoring is feasible, comparable to unannounced pill counts, and acceptable. AIDS Behav. 2012;16(2):375–82.
Haberer JE, Kiwanuka J, Nansera D, Muzoora C, Hunt PW, So J, et al. Realtime adherence monitoring of antiretroviral therapy among hiv-infected adults and children in rural uganda. Aids. 2013;27(13):2166–8.
Haberer JE, Kahane J, Kigozi I, Emenyonu N, Hunt P, Martin J, et al. Real-time adherence monitoring for HIV antiretroviral therapy. AIDS Behav. 2010;14(6):1340–6.
Sabin LL, Desilva MB, Hamer DH, Keyi X, Yue Y, Wen F, et al. Barriers to adherence to antiretroviral medications among patients living with HIV in southern China: a qualitative study. AIDS Care. 2008;20(10):1242–50.
Sabin LL, DeSilva MB, Hamer DH, Xu K, Zhang J, Li T, et al. Using electronic drug monitor feedback to improve adherence to antiretroviral therapy among HIV-positive patients in China. AIDS Behav. 2010;14(3):580–9.
Wools-Kaloustian K, Kimaiyo S, Diero L, Siika A, Sidle J, Yiannoutsos CT, et al. Viability and effectiveness of large-scale HIV treatment initiatives in sub-Saharan Africa: experience from western Kenya. Aids. 2006;20(1):41–8.
Nachega JB, Hislop M, Dowdy DW, Chaisson RE, Regensberg L, Maartens G. Adherence to nonnucleoside reverse transcriptase inhibitor-based HIV therapy and virologic outcomes. Ann Intern Med. 2007;146(8):564–73.
Bangsberg DR. Less than 95% adherence to nonnucleoside reverse-transcriptase inhibitor therapy can lead to viral suppression. Clin Infect Dis. 2006;43(7):939–41.
Mocroft A, Horban A, Clumeck N, Stellbrink HJ, Monforte ADA, Zilmer K, et al. Comparison of single and boosted protease inhibitor versus nonnucleoside reverse transcriptase inhibitor-containing cART regimens in antiretroviral-naive patients starting cART after January 1, 2000. HIV Clin Trials. 2006;7(6):271–84.
Weiser SD, Guzman D, Riley ED, Clark R, Bangsberg DR. Higher rates of viral suppression with nonnucleoside reverse transcriptase inhibitors compared to single protease inhibitors are not explained by better adherence. HIV Clin Trials. 2004;5(5):278–87.
Price MA, Wallis CL, Lakhi S, Karita E, Kamali A, Anzala O, et al. Transmitted HIV type 1 drug resistance among individuals with recent HIV infection in East and Southern Africa. AIDS Res Hum Retrovir. 2011;27(1):5–12.
Phanuphak P, Sirivichayakul S, Jiamsakul A, Sungkanuparph S, Kumarasamy N, Lee MP, et al. Transmitted drug resistance and antiretroviral treatment outcomes in non-subtype B HIV-1-infected patients in South East Asia. J Acquir Immune Defic Syndr. 2014;66(1):74–9.
Mantovani NP, Azevedo RG, Rabelato JT, Sanabani S, Diaz RS, Komninakis SV. Analysis of transmitted resistance to raltegravir and selective pressure among HIV-1-infected patients on a failing HAART in Sao Paulo, Brazil. J Clin Microbiol. 2012;50(6):2122–5.
Sherr L, Lampe F, Norwood S, Leake Date H, Harding R, Johnson M, et al. Adherence to antiretroviral treatment in patients with HIV in the UK: a study of complexity. AIDS Care. 2008;20(4):442–8.
Acknowledgments
We wish to thank Ka Lai Poon for her assistance in generating the library of subject-by-subject scatter plots for this analysis. The AFL study was supported by a cooperative agreement (GHS-A-00-03-00030-00) between Boston University and the Office of Health and Nutrition of the United States Agency for International Development (USAID), with additional support from the World Health Organization (WHO) and CDC-GAP/China. Dr. Gill’s work was supported by NIH/NIAID K23 AI 62208. This study was supported by a cooperative agreement (GHS-A-00-03-00030-00) between Boston University and the Office of Health and Nutrition of the United States Agency for International Development (USAID), with additional support from the World Health Organization (WHO) and the United States Centers for Disease Control and Prevention.
Conflict of interest
All authors declare no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
10461_2015_1065_MOESM1_ESM.docx
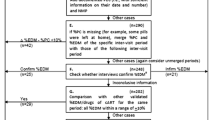
Supplementary material 1 (DOCX 2193 kb). A. SAS codes used to generate the uni- and bi-modal scatter plots. B. Individual subject uni-modal scatter plots. C. Individual subject bi-modal scatter plots
Rights and permissions
About this article
Cite this article
Gill, C.J., DeSilva, M.B., Hamer, D.H. et al. Novel Approaches for Visualizing and Analyzing Dose-Timing Data from Electronic Drug Monitors, or “How the ‘Broken Window’ Theory Pertains to ART Adherence”. AIDS Behav 19, 2057–2068 (2015). https://doi.org/10.1007/s10461-015-1065-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-015-1065-3