Abstract
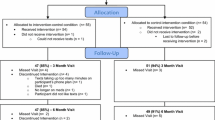
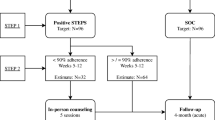
HIV+ persons with co-occurring bipolar disorder (HIV+/BD+) have elevated rates of medication nonadherence. We conducted a 30-day randomized controlled trial of a two-way, text messaging system, iTAB (n = 25), compared to an active comparison (CTRL) (n = 25) to improve antiretroviral (ARV) and psychotropic (PSY) adherence and dose timing. Both groups received medication adherence psychoeducation and daily texts assessing mood. The iTAB group additionally received personalized medication reminder texts. Participants responded to over 90 % of the mood and adherence text messages. Mean adherence, as assessed via electronic monitoring caps, was high and comparable between groups for both ARV (iTAB 86.2 % vs. CTRL 84.8 %; p = 0.95, Cliff’s d = 0.01) and PSY (iTAB 78.9 % vs. CTRL 77.3 %; p = 0.43, Cliff’s d = −0.13) medications. However, iTAB participants took ARVs significantly closer to their intended dosing time than CTRL participants (iTAB: 27.8 vs. CTRL: 77.0 min from target time; p = 0.02, Cliff’s d = 0.37). There was no group difference on PSY dose timing. Text messaging interventions may represent a low-burden approach to improving timeliness of medication-taking behaviors among difficult-to-treat populations. The benefits of improved dose timing for long-term medication adherence require additional investigation.
Resumen
Las personas infectadas con VIH y que a la vez tienen trastorno bipolar (VIH+/BD+), tienen tasas elevadas de no adherencia a medicamentos. En el presente estudio, hemos llevado a cabo un ensayo controlado aleatorio comparando un sistema de mensajes de texto, ITAB (n = 25), con un grupo control (CTRL) (n = 25). El objectivo del estudio fue mejorar la adherencia a medicamentos antirretrovirales (ARV) y psicotrópicos (PSY) y también mejorar la sincronización de las dosis. Ambos grupos recibieron psicoeducación sobre la importancia de la adherencia a los medicamentos y textos diarios evalúando el estado de ánimo. El grupo ITAB recibió adicionalmente mensajes de textos personalizados que les recordaban tomar los medicamentos. Todos los participantes respondieron a más del 90 % de los mensajes de texto sobre el estado de ánimo y la adherencia. El promedio de adherencia, evaluado a través de las tapaderas de monitoreo electrónico fue alto y comparable entre los grupos para los dos medicamentos, ARV (ITAB 86,2 % frente a 84,8 % CTRL; p = 0,95, Cliff’s d = 0,01) y PSY (ITAB 78,9 % frente a 77,3 % CTRL; p = 0,43, Cliff’s d = −0,13). Sin embargo, los participantes en el grupo ITAB tomaron medicamentos ARV significativamente más cerca del tiempo en que debían tomarlos que los participantes CTRL (ITAB : 27,8 vs. CTRL : 77,0 minutos desde el momento en que debían tomarlos; p = 0,02, Cliff’s d = 0,37). No hubo diferencia entre los grupos en la sincronización de la dosis para los medicamentos PSY. En conclusión, intervenciones utilizando mensajes de texto pueden representar una forma mas fácil de mejorar la puntualidad en la que individuos difíciles de tratar deben tomarse los medicamentos. Sin embargo, los beneficios de mejorar la sincronización en la dosis de medicamentos y la adherencia a estos a largo plazo requieren investigación adicional.



Similar content being viewed by others
References
Thompson MA, Aberg JA, Hoy JF, Telenti A, Benson C, Cahn P, et al. Antiretroviral treatment of adult HIV infection: 2012 recommendations of the International Antiviral Society-USA panel. JAMA. 2012;308(4):387–402.
Bangsberg DR. Preventing HIV antiretroviral resistance through better monitoring of treatment adherence. J Infect Dis. 2008;197(Suppl 3):S272–8.
Bangsberg DR, Deeks SG. Is average adherence to HIV antiretroviral therapy enough? J Gen Intern Med. 2002;17(10):812–3.
Mannheimer S, Friedland G, Matts J, Child C, Chesney M. The consistency of adherence to antiretroviral therapy predicts biologic outcomes for human immunodeficiency virus-infected persons in clinical trials. Clin Infect Dis. 2002;34(8):1115–21.
Mathes T, Pieper D, Antoine SL, Eikermann M. Adherence-enhancing interventions for highly active antiretroviral therapy in HIV-infected patients—a systematic review. HIV Med. 2013;14(10):583–95.
Liu H, Miller LG, Hays RD, Golin CE, Wu T, Wenger NS, et al. Repeated measures longitudinal analyses of HIV virologic response as a function of percent adherence, dose timing, genotypic sensitivity, and other factors. J Acquir Immune Defic Syndr. 2006;41(3):315–22.
Bangsberg DR, Kroetz DL, Deeks SG. Adherence-resistance relationships to combination HIV antiretroviral therapy. Curr HIV/AIDS Rep. 2007;4(2):65–72.
Parienti JJ, Das-Douglas M, Massari V, Guzman D, Deeks SG, Verdon R, et al. Not all missed doses are the same: sustained NNRTI treatment interruptions predict HIV rebound at low-to-moderate adherence levels. PLoS ONE. 2008;3(7):e2783.
Ghidei L, Simone MJ, Salow MJ, Zimmerman KM, Paquin AM, Skarf LM, et al. Aging, antiretrovirals, and adherence: a meta analysis of adherence among older HIV-infected individuals. Drugs Aging. 2013;30(10):809–19.
Moore DJ, Blackstone K, Woods SP, Ellis RJ, Atkinson JH, Heaton RK, et al. Methamphetamine use and neuropsychiatric factors are associated with antiretroviral non-adherence. AIDS Care. 2012;24(12):1504–13.
Moore DJ, Posada C, Parikh M, Arce M, Vaida F, Riggs PK, et al. HIV-infected individuals with co-occurring bipolar disorder evidence poor antiretroviral and psychiatric medication adherence. AIDS Behav. 2012;16(8):2257–66.
Weiser SD, Wolfe WR, Bangsberg DR. The HIV epidemic among individuals with mental illness in the United States. Curr HIV/AIDS Rep. 2004;1(4):186–92.
Woodward EN, Pantalone DW. The role of social support and negative affect in medication adherence for HIV-infected men who have sex with men. AIDS Care. 2012;23(5):388–96.
Beyer JL, Taylor L, Gersing KR, Krishnan KR. Prevalence of HIV infection in a general psychiatric outpatient population. Psychosomatics. 2007;48(1):31–7.
Walkup J, Crystal S, Sambamoorthi U. Schizophrenia and major affective disorder among Medicaid recipients with HIV/AIDS in New Jersey. Am J Public Health. 1999;89(7):1101–3.
Springer SA, Dushaj A, Azar MM. The impact of DSM-IV mental disorders on adherence to combination antiretroviral therapy among adult persons living with HIV/AIDS: a systematic review. AIDS Behav. 2012;16(8):2119–43.
Mellins CA, Havens JF, McDonnell C, Lichtenstein C, Uldall K, Chesney M, et al. Adherence to antiretroviral medications and medical care in HIV-infected adults diagnosed with mental and substance abuse disorders. AIDS Care. 2009;21(2):168–77.
Scott J, Pope M. Nonadherence with mood stabilizers: prevalence and predictors. J Clin Psychiatry. 2002;63(5):384–90.
Colom F, Vieta E, Tacchi MJ, Sanchez-Moreno J, Scott J. Identifying and improving non-adherence in bipolar disorders. Bipolar Disord. 2005;7(Suppl 5):24–31.
Li J, McCombs JS, Stimmel GL. Cost of treating bipolar disorder in the California Medicaid (Medi-Cal) program. J Affect Disord. 2002;71(1–3):131–9.
Binford MC, Kahana SY, Altice FL. A systematic review of antiretroviral adherence interventions for HIV-infected people who use drugs. Curr HIV/AIDS Rep. 2012;9(4):287–312.
Centers for Disease Control and Prevention (CDC). Compendium of evidence-based HIV behavioral interventions. 2013. http://www.cdc.gov/hiv/prevention/research/compendium/ma/complete.html.
Krishna S, Boren SA, Balas EA. Healthcare via cell phones: a systematic review. Telemed J E Health. 2009;15(3):231–40.
Coomes CM, Lewis MA, Uhrig JD, Furberg RD, Harris JL, Bann CM. Beyond reminders: a conceptual framework for using short message service to promote prevention and improve healthcare quality and clinical outcomes for people living with HIV. AIDS Care. 2012;24(3):348–57.
Finitsis DJ, Pellowski JA, Johnson BT. Text message intervention designs to promote adherence to antiretroviral therapy (ART): a meta-analysis of randomized controlled trials. PLoS ONE. 2014;9(2):e88166.
Horvath T, Azman H, Kennedy GE, Rutherford GW. Mobile phone text messaging for promoting adherence to antiretroviral therapy in patients with HIV infection. Cochrane Database Syst Rev. 2014;14:CD009756.
Lester RT, Ritvo P, Mills EJ, Kariri A, Karanja S, Chung MH, et al. Effects of a mobile phone short message service on antiretroviral treatment adherence in Kenya (WelTel Kenya1): a randomised trial. Lancet. 2010;376(9755):1838–45.
Pop-Eleches C, Thirumurthy H, Habyarimana JP, Zivin JG, Goldstein MP, de Walque D, et al. Mobile phone technologies improve adherence to antiretroviral treatment in a resource-limited setting: a randomized controlled trial of text message reminders. AIDS. 2011;25(6):825–34.
Dowshen N, Kuhns LM, Johnson A, Holoyda BJ, Garofalo R. Improving adherence to antiretroviral therapy for youth living with HIV/AIDS: a pilot study using personalized, interactive, daily text message reminders. J Med Internet Res. 2012;14(2):e51.
Bauer M, Grof P, Gyulai L, Rasgon N, Glenn T, Whybrow PC. Using technology to improve longitudinal studies: self-reporting with ChronoRecord in bipolar disorder. Bipolar Disord. 2004;6(1):67–74.
Bopp JM, Miklowitz DJ, Goodwin GM, Stevens W, Rendell JM, Geddes JR. The longitudinal course of bipolar disorder as revealed through weekly text messaging: a feasibility study. Bipolar Disord. 2010;12(3):327–34.
Wenze SJ, Armey MF, Miller IW. Feasibility and acceptability of a mobile intervention to improve treatment adherence in bipolar disorder: a pilot study. Behavior Modif. 2014.
Depp CA, Mausbach B, Granholm E, Cardenas V, Ben-Zeev D, Patterson TL, et al. Mobile interventions for severe mental illness: design and preliminary data from three approaches. J Nerv Mental Dis. 2010;198(10):715–21.
Schulz KF, Altman DG, Moher D, Group C. CONSORT 2010 Statement: updated guidelines for reporting parallel group randomised trials. BMC Med. 2010;8:18.
Balfour L, Kowal J, Silverman A, Tasca GA, Angel JB, Macpherson PA, et al. A randomized controlled psycho-education intervention trial: improving psychological readiness for successful HIV medication adherence and reducing depression before initiating HAART. AIDS Care. 2006;18(7):830–8.
Colom F, Vieta E, Reinares M, Martinez-Aran A, Torrent C, Goikolea JM, et al. Psychoeducation efficacy in bipolar disorders: beyond compliance enhancement. J Clin Psychiatry. 2003;64(9):1101–5.
Glanz K, Rimer BK. Theory at a glance: a guide for health promotion practice. US Department of Health and Human Services, Public Health Service, National Institutes of Health, National Cancer Institute; 1997.
Young RC, Biggs JT, Ziegler VE, Meyer DA. A rating scale for mania: reliability, validity and sensitivity. Br J Psychiatry. 1978;133:429–35.
Beck AT, Steer RA, Brown GK. BDI: Beck Depression Inventory: Manual. San Antonio: Psychological Corporation; 1996.
Badiee J, Riggs PK, Rooney AS, Vaida F, Grant I, Atkinson JH, et al. Approaches to identifying appropriate medication adherence assessments for HIV infected individuals with comorbid bipolar disorder. AIDS Patient Care STDs. 2012;26(7):388–94.
Heaton RK, Franklin DR, Ellis RJ, McCutchan JA, Letendre SL, Leblanc S, et al. HIV-associated neurocognitive disorders before and during the era of combination antiretroviral therapy: differences in rates, nature, and predictors. J Neurovirol. 2011;17(1):3–16.
Cliff N. Dominance statistics: ordinal analyses to answer ordinal questions. Psychol Bull. 1993;114(3):494.
Hoogenhout EM, de Groot RH, van der Elst W, Jolles J. Effects of a comprehensive educational group intervention in older women with cognitive complaints: a randomized controlled trial. Aging Mental Health. 2012;16(2):135–44.
Romano J, Kromrey JD, Coraggio J, Skowronek J, Devine L. Exploring methods for evaluating group differences on the NSSE and other surveys: Are the t-test and Cohen’s d indices the most appropriate choices? Paper presented at the annual meeting of the Southern Association for Institutional Research; October 14–17, 2006; Arlington, Virginia.
Gill CJ, Sabin LL, Hamer DH, Keyi X, Jianbo Z, Li T, et al. Importance of dose timing to achieving undetectable viral loads. AIDS Behav. 2010;14(4):785–93.
Pompili M, Venturini P, Palermo M, Stefani H, Seretti ME, Lamis DA, et al. Mood disorders medications: predictors of nonadherence—review of the current literature. Expert Rev Neurother. 2013;13(7):809–25.
Garfein R, Collins K, Muñoz F, Moser K, Cerecer-Callu P, Sullivan M, et al., editors. Use of mobile phones for video directly observed therapy among tuberculosis patients in high and low income countries. Wireless Health; 2013 Nov 1–3; Baltimore.
Bobrow K, Brennan T, Springer D, Levitt NS, Rayner B, Namane M, et al. Efficacy of a text messaging (SMS) based intervention for adults with hypertension: protocol for the StAR (SMS Text-message Adherence suppoRt trial) randomised controlled trial. BMC Public Health. 2014;14:28.
Muench F, van Stolk-Cooke K, Morgenstern J, Kuerbis AN, Markle K. Understanding messaging preferences to inform development of mobile goal-directed behavioral interventions. J Med Internet Res. 2014;16(2):e14.
Wendel CS, Mohler MJ, Kroesen K, Ampel NM, Gifford AL, Coons SJ. Barriers to use of electronic adherence monitoring in an HIV clinic. Ann Pharmacother. 2001;35(9):1010–5.
Bova CA, Fennie KP, Knafl GJ, Dieckhaus KD, Watrous E, Williams AB. Use of electronic monitoring devices to measure antiretroviral adherence: practical considerations. AIDS Behav. 2005;9(1):103–10.
Levine AJ, Hinkin CH, Castellon SA, Mason KI, Lam MN, Perkins A, et al. Variations in patterns of highly active antiretroviral therapy (HAART) adherence. AIDS Behav. 2005;9(3):355–62.
Walsh JC, Mandalia S, Gazzard BG. Responses to a 1 month self-report on adherence to antiretroviral therapy are consistent with electronic data and virological treatment outcome. AIDS. 2002;16(2):269–77.
Acknowledgments
The present work was supported by California HIV/AIDS Research Program IDEA Award ID09-SD-047 (D.J. Moore, PI) as well as the HIV Neurobehavioral Research Center (HNRC) NIMH/CSPAR Award Number P30MH062512 (R.K. Heaton, PI).
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
The members of the HIV Neurobehavioral Research Program (HNRP) Group given in the "Appendix".
Appendix: HIV Neurobehavioral Research Program (HNRP) Group
Appendix: HIV Neurobehavioral Research Program (HNRP) Group
The San Diego HIV Neurobehavioral Research Center [HNRC] group is affiliated with the University of California, San Diego, the Naval Hospital, San Diego, and the Veterans Affairs San Diego Healthcare System, and includes: Director: Robert K. Heaton, Ph.D., Co-Director Igor Grant, M.D.; Associate Directors: J. Hampton Atkinson, M.D., Ronald J. Ellis, M.D., Ph.D., and Scott Letendre, M.D.; Center Manager: Thomas D. Marcotte, Ph.D.; Jennifer Marquie-Beck, M.P.H.; Melanie Sherman; Neuromedical Component Ronald J. Ellis, M.D., Ph.D. (P.I.), Scott Letendre, M.D., J. Allen McCutchan, M.D., Brookie Best, Pharm.D., Rachel Schrier, Ph.D., Debra Rosario, M.P.H.; Neurobehavioral Component Robert K. Heaton, Ph.D. (P.I.), J. Hampton Atkinson, M.D., Steven Paul Woods, Psy.D., Thomas D. Marcotte, Ph.D., Mariana Cherner, Ph.D., David J. Moore, Ph.D., Matthew Dawson; Neuroimaging Component Christine Fennema-Notestine, Ph.D. (P.I.), Monte S. Buchsbaum, M.D., John Hesselink, M.D., Sarah L. Archibald, M.A., Gregory Brown, Ph.D., Richard Buxton, Ph.D., Anders Dale, Ph.D., Thomas Liu, Ph.D.; Neurobiology Component Eliezer Masliah, M.D. (P.I.), Cristian Achim, M.D., Ph.D.; Neurovirology Component: David M. Smith, M.D. (P.I.), Douglas Richman, M.D.; International Component J. Allen McCutchan, M.D., (P.I.), Mariana Cherner, Ph.D.; Developmental Component Cristian Achim, M.D., Ph.D.; (P.I.), Stuart Lipton, M.D., Ph.D.; Participant Accrual and Retention Unit J. Hampton Atkinson, M.D. (P.I.), Jennifer Marquie-Beck, M.P.H.; Data Management and Information Systems Unit Anthony C. Gamst, Ph.D. (P.I.), Clint Cushman; Statistics Unit Ian Abramson, Ph.D. (P.I.), Florin Vaida, Ph.D. (Co-PI), Reena Deutsch, Ph.D., Anya Umlauf, M.S.
The views expressed in this article are those of the authors and do not reflect the official policy or position of the Department of the Navy, Department of Defense, nor the United States Government.
Rights and permissions
About this article
Cite this article
Moore, D.J., Poquette, A., Casaletto, K.B. et al. Individualized Texting for Adherence Building (iTAB): Improving Antiretroviral Dose Timing Among HIV-Infected Persons with Co-occurring Bipolar Disorder. AIDS Behav 19, 459–471 (2015). https://doi.org/10.1007/s10461-014-0971-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-014-0971-0