Abstract
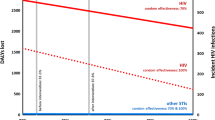
Mexico has a concentrated HIV epidemic, with male sex workers constituting a key affected population. We estimated annual HIV cumulative incidence among male sex workers’ partners, and then compared incidence under three hypothetical intervention scenarios: improving condom use; and scaling up HIV treatment as prevention, considering current viral suppression rates (CVS, 60.7 %) or full viral suppression among those treated (FVS, 100 %). Clinical and behavioral data to inform model parameterization were derived from a sample (n = 79) of male sex workers recruited from street locations and Clínica Condesa, an HIV clinic in Mexico City. We estimated annual HIV incidence among male sex workers’ partners to be 8.0 % (95 % CI: 7.3–8.7). Simulation models demonstrated that increasing condom use by 10 %, and scaling up HIV treatment initiation by 50 % (from baseline values) would decrease the male sex workers-attributable annual incidence to 5.2, 4.4 % (CVS) and 3.2 % (FVS), respectively. Scaling up the number of male sex workers on ART and implementing interventions to ensure adherence is urgently required to decrease HIV incidence among male sex workers’ partners in Mexico City.
Resumen
México enfrenta una epidemia concentrada del VIH, con hombres trabajadores sexuales que constituyen una población afectada clave. Se estimó la incidencia acumulada anual del VIH entre las parejas de hombres trabajadores sexuales. Se modeló esa incidencia bajo tres escenarios de intervención hipotéticos: mejorar el uso del condón; la ampliación del tratamiento del VIH como prevención, teniendo en cuenta las tasas de supresión viral actual (SVA, 60,7 %), o la supresión viral completa entre los tratados (SVC, 100 %). Los datos clínicos y de comportamiento para informar los parámetros del modelo se obtuvieron de una muestra (n = 79) de hombres trabajadores sexuales reclutados de lugares de la calle y la Clínica Especializada Condesa, en la Ciudad de México. Se estimó la incidencia anual del VIH entre las parejas de hombres trabajadores sexuales en 8,0 % (IC 95 %: 7,3–8,7). La simulación demostró que el aumento del uso del preservativo en un 10 %, y la ampliación de la iniciación del tratamiento del VIH en un 50 % (a partir de los valores basales) disminuiría la incidencia anual de la transmisión atribuible a hombres trabajadores sexuales al 5,2 %, al 4,4 % (SVA) y al 3,2 % (SVC), respectivamente. Se requiere urgentemente el aumento del número de hombres trabajadores sexuales en tratamiento antirretroviral e intervenciones para garantizar el apego al tratamiento para reducir la incidencia del VIH entre las parejas de hombres trabajadores sexuales en la Ciudad de México.




Similar content being viewed by others
Notes
The code/data analysis for this paper was generated using SAS software, Version 9.3 of the SAS System for Windows. Copyright © 2014 SAS Institute Inc. SAS and all other SAS Institute Inc. product or service names are registered trademarks or trademarks of SAS Institute Inc., Cary, NC, USA.
References
Censo de Población y Vivienda 2010 [Population and Housing Census 2010] [Internet]. Instituto Nacional de Estadística y Geografía (INEGI) [National Insitute of Statistics and Geography]. 2010 [cited April 29, 2014].
Bautista-Arredondo S, Colchero MA, Romero M, et al. Is the HIV epidemic stable among MSM in Mexico? HIV prevalence and risk behavior results from a nationally representative survey among men who have sex with men. PLoS One. 2013;8(9):e72616 Epub ahead of print.
CONASIDA. Informe Nacional de Avances en la Lucha contra el SIDA, México 2012 [Progress Report on the Fight Against AIDS, Mexico 2012]. Mexico City: Consejo Nacional para la Prevención y Control del SIDA, 2012.
Liguori AL, Aggleton P. Aspects of male sex work in Mexico city. In: Aggleton P, editor. Men who sell sex: international perspectives on male prostitution and HIV/AIDS. London: Routledge; 1999. p. 103–26.
Infante C, Sosa-Rubi SG, Cuadra SM. Sex work in Mexico: vulnerability of male, travesti, transgender and transsexual sex workers. Cult Health Sex. 2009;11(2):125–37.
Barrón-Limón S, Semple SJ, Strathdee SA, et al. Correlates of unprotected anal sex among men who have sex with men in Tijuana, Mexico. BMC Public Health. 2012;12(1):433.
Galárraga O, Sosa-Rubi SG, Infante C, et al. Willingness-to-accept reductions in HIV risks: conditional economic incentives in Mexico. Eur J Health Econ. 2013;15(1):41–55.
Deiss RG, Brouwer KC, Loza O, et al. High-risk sexual and drug using behaviors among male injection drug users who have sex with men in 2 Mexico-US border cities. Sex Transm Dis. 2008;35(3):243–9.
Bautista-Arredondo S, Colchero MA, Sosa Rubí SG, et al. Results of a sero-revalence survey in gathering points among men who have sex with men. Instituto Nacional de Salud Pública Centro de Investigación en Evaluación y Encuestas Executive summary. 2012;3(3).
Crabtree-Ramírez B, Caro-Vega Y, Shepherd BE, et al. Cross-sectional analysis of late HAART initiation in Latin America and the Caribbean: late testers and late presenters. PLoS One. 2011;6(5):e20272.
Crabtree-Ramírez B, Caro-Vega Y, Belaurarán-Zamudio F, et al. High prevalence of late diagnosis of HIV in Mexico during the HAART era. Salud Publica Mex. 2012;54(5):506–14.
Bautista-Arredondo S, Dmytraczenko T, Kombe G, et al. Costing of scaling up HIV/AIDS treatment in Mexico. Salud Publica Mex. 2008;4:S437–44.
Gertler P, Shah M, Bertozzi S. Risky business: the market for unprotected commercial sex. J Polit Econ. 2005;113:518–50.
Rao V. Sex workers and the cost of safe sex: the compensating differential for condom use among calcutta prostitutes. J Dev Econ. 2003;71:585–603.
Shah M. Do sex workers respond to disease? Evidence from the male market for sex. Am Econ Rev. 2013;1003(3):445–50.
Cai WD, Zhao J, Zhao JK, et al. HIV prevalence and related risk factors among male sex workers in Shenzhen, China: results from a time-location sampling survey. Sex Transm Infect. 2010;86(1):15–20.
Baral S, Kizub D, Masenior NF, et al. Male sex workers in Moscow, Russia: a pilot study of demographics, substance use patterns, and prevalence of HIV-1 and sexually transmitted infections. AIDS Care. 2010;22(1):112–8.
Vuylsteke B, Semde G, Sika L, et al. High prevalence of HIV and sexually transmitted infections among male sex workers in Abidjan, Cote d’Ivoire: need for services tailored to their needs. Sex Transm Infect. 2012;88(4):288–93.
Dos Ramos Farias MS, Garcia MN, Reynaga E, et al. First report on sexually transmitted infections among trans (male to female transvestites, transsexuals, or transgender) and male sex workers in Argentina: high HIV, HPV, HBV, and syphilis prevalence. Int J Infect Dis. 2011;15(9):e635–40.
Guadamuz TE, Kunawararak P, Beyrer C, et al. HIV prevalence, sexual and behavioral correlates among Shan, Hill tribe, and Thai male sex workers in Northern Thailand. AIDS Care. 2010;22(5):597–605.
Toledo CA, Varangrat A, Wimolsate W, et al. Examining HIV infection among male sex workers in Bangkok, Thailand: a comparison of participants recruited at entertainment and street venues. AIDS Educ Prev. 2010;22(4):299–311.
Sethi G, Holden BM, Gaffney J, et al. HIV, sexually transmitted infections, and risk behaviours in male sex workers in London over a 10 year period. Sex Transm Infect. 2006;82(5):359–63.
Leuridan E, Wouters K, Stalpaert M, et al. Male sex workers in Antwerp, Belgium: a descriptive study. Int J STD AIDS. 2005;16(11):744–8.
Marino R, Minichiello V, Disogra C. Male sex workers in Cordoba, Argentina: sociodemographic characteristics and sex work experiences. Revista panamericana de salud publica [Pan American journal of public health]. 2003;13(5):311–9.
Robertson AM, Syvertsen JL, Ulibarri MD, et al. Prevalence and correlates of HIV and sexually transmitted infections among female sex workers and their non-commercial male partners in two Mexico-USA border cities. J Urban Health. 2014;91(4):752–67 Epub ahead of print.
Baggaley RF, White RG, Boily MC. HIV transmission risk through anal intercourse: systematic review, meta-analysis and implications for HIV prevention. Int J Epidemiol. 2010;39(4):1048–63.
SAS. 9.3 ed. Cary: SAS Institute Inc; 2013.
Fan X, Sivo SA, Keenan SC, et al. SAS® for Monte Carlo studies: a guide for quantitative researchers. Cary: SAS Publishing; 2002. p. 272.
Balaji AB, Bowles KE, Le BC, et al. High HIV incidence and prevalence and associated factors among young MSM. AIDS. 2008;27(2):269–78.
Antiretroviral therapy for HIV infection in adults and adolescents. Geneva: WHO; 2010.
Siegfried N, Uthman OA, Rutherford GW. Review optimal time for initiation of antiretroviral therapy in asymptomatic, HIV-infected, treatment-naive adults. Cochrane Database Syst Rev. 2010;3:CD008272.
Kitahata MM, Gange SJ, Abraham AG, et al. Effect of early versus deferred antiretroviral therapy for HIV on survival. N Engl J Med. 2009;360(18):1815–26.
Sax PE, Baden LR. When to start antiretroviral therapy-ready when you are? N Engl J Med. 2009;360(18):1897–9.
Stanecki K, Daher J, Stover J, et al. Antiretroviral therapy needs: the effect of changing global guidelines. Sex Transm Infect. 2010;86(Suppl_2):i62–ii6.
Muessiga KE, Smith MK, Powersa KA, et al. Does ART prevent HIV transmission among MSM? AIDS. 2012;26(18):2267–73.
Kalichman SC, Rompa D. Treatment adherence and unprotected sex practices among persons receiving antiretroviral therapy. Sex Transm Infect. 2003;79:59–61.
Remien RH, Dolezal C, Wagner GJ, et al. The association between poor antiretroviral adherence and unsafe sex: differences by gender and sexual orientation and implications for scale-up of treatment as prevention. AIDS Behav. 2013;18(8):1541–7.
Cohen MS, Chen YQ, McCauley M, et al. Prevention of HIV-1 infection with early antiretroviral treatment. N Engl J Med. 2011;365:493–505.
Cohen MS, Smith MK, Muessig KE, Hallett TB, Powers KA, Kashuba AD. Antiretroviral treatment of HIV-1 prevents transmission of HIV-1: where do we go from here? Lancet. 2013;382(9903):1515–24.
Weller SC, Davis-Beaty K. Condom effectiveness in reducing heterosexual HIV transmission. Cochrane Database Syst Rev. 2002;1:CD003255.
Wade Taylor S, Mayer KH, Elsesser SM, et al. Optimizing content for pre-exposure prophylaxis (PrEP) counseling for men who have sex with men: perspectives of PrEP users and high-risk PrEP naïve men. AIDS Behav. 2013;18(5):871–9.
Robertson AM, Syvertsen JL, Martinez G, et al. Acceptability of vaginal microbicides among female sex workers and their intimate male partners in two Mexico-US border cities: a mixed methods analysis. Glob Public Health. 2013;8(5):619–33.
McMahon JH, Elliott JH, Bertagnolio S. Viral suppression after 12 months of antiretroviral therapy in low- and middle-income countries: a systematic review. Bull World Health Organ. 2013;91:377–85.
Li X, Buechner JM, Tarwater PM, et al. A diamond-shaped equiponderant graphical display of the effects of two categorical predictors on continuous outcomes. Am Stat. 2003;57(3):193–9.
Acknowledgments
We gratefully acknowledge the Punto Seguro staff members: Nathalie Gras, Octavio Parra, Jehovani Tena. Biani Saavedra, Fernando Ruiz and Cecilia Hipólito provided research assistance; Dr. Carlos Conde’s INSP laboratory with María Olamendi and Santa García conducted the PCR diagnosis of chlamydia and gonococcus in urine samples. Dr. Florentino Badial-Hernández and Luis Juárez-Figueroa contributed to participants recruitment, care, and HIV testing. Questionnaires were programmed into A-CASI by CEO (Edgar Díaz). Project management and administration: CISIDAT (Research Consortium on HIV/AIDS and TB). We especially thank the participants for agreeing to become part of Punto Seguro. Supported by: US National Institutes of Health (R21HD065525; “Conditional economic incentives to reduce HIV risk: A pilot in Mexico”; PI: Galárraga); and the Mexican National Center for HIV/AIDS Control and Prevention (CENSIDA). Dr. Filipe Monteiro is supported by a postdoctoral fellowship, T32 Training Program in HIV and other Consequences of Substance Abuse (Grant Number T32-DA013911). Dr. Brandon Marshall is supported by a Richard B. Salomon Faculty Research Award from Brown University. This publication was made possible with help from the Lifespan/Tufts/Brown Center for AIDS Research. The described project was supported by Grant Number P30AI042853 from the National Institute of Allergy and Infectious Diseases. The content is solely of responsibility of the authors and does not necessarily represent the official views of the any of the National Institutes of Health.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Monteiro, J.F.G., Marshall, B.D.L., Escudero, D. et al. Preventing HIV Transmission Among Partners of HIV-Positive Male Sex Workers in Mexico City: A Modeling Study. AIDS Behav 19, 1579–1588 (2015). https://doi.org/10.1007/s10461-014-0915-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-014-0915-8