Abstract
Cancer cells produce galectin-1 as a tumor promoting protein. Thiodigalactoside (TDG) as a non-metabolised small drug, is shown to suppress tumor growth by inhibiting multiple cancer enhancing activities of galectin-1, including immune cell dysregulation, angiogenesis and protection against oxidative stress. Thus, using B16F10 melanoma and 4T1 orthotopic breast cancer models, intratumoral injection of TDG significantly raised the levels of tumor-infiltrating CD8+ lymphocytes and reduced CD31+ endothelial cell content, reducing tumor growth. TDG treatment of tumors in Balb/c nude mice (defective in T cell immunity) reduced angiogenesis and slowed tumor growth by a third less than in immunocompetent mice. Knocking down galectin-1 expression (G1KD) in both cancer cell types significantly impeded tumor growth and the sensitivity of the G1KD tumors to TDG was severely reduced, highlighting a specific role for galectin-1. Endothelial cells were protected by galectin-1 from oxidative stress-induced apoptosis induced by H2O2, but TDG inhibited this antioxidant protective effect of galectin-1 and reduced tube forming activity in angiogenic assays. We show for the first time that the single agent, TDG, concurrently prevents many tumor promoting effects of galectin-1 on angiogenesis, immune dysregulation and protection against oxidative stress, providing a potent and novel small molecule as an anti-cancer drug.
Similar content being viewed by others
Introduction
Galectin-1 is a β-galactoside binding protein with a highly conserved carbohydrate-recognition domain (CRD) [1, 2]. A wide range of tumor cells over-express galectin-1, which has been shown in separate studies to play important roles in tumor progression, including tumor cell proliferation and adhesion as well as immune cell inhibition by inducing apoptosis of activated T cells [3–6]. The outcome of the immune inhibitory influences is a reduced immune response by the host, thereby facilitating tumor growth. Recent reports document that galectin-1 is also important for tumor angiogenesis [3, 7]. In addition, hypoxia inducible factor-1 (HIF-1), activated during the cellular response to hypoxia commonly associated with tumor growth induces galectin-1 expression. Ironically, hypoxia is associated with increased levels of oxidative stress, activating signaling pathways leading to HIF family protein stabilization and activation (reviewed in [8]).
Tumor angiogenesis refers to formation of new blood vessels induced by tumor-secreted factors and is involved in tumor progression [9]. Growth of solid tumors strictly depends on the formation of new blood vessels and this tumorigenic neovascularization requires several steps including stimulation of vascular endothelial cells (ECs) and destabilization of the basal membrane and extracellular matrix [10]. Hypoxia, due to poor blood supply, is associated with oxidative stress and increased tumor angiogenesis [11] and is also recognized as a major obstacle to successful immunotherapeutic outcomes, jeopardizing cancer therapy. More specifically, the aberrant new blood vessel formation hampers infiltration and recruitment of immune effector cells into tumors because of the chaotic vascular morphology and reduced expression of adhesion molecules [12]. In fact, it has been shown that normalization of the tumor vasculature improved immunotherapeutic outcomes in a mouse tumor model [13].
High levels of galectin-1 expression have been observed in growth stimulated ECs as well as in tumor cells, thereby promoting the proliferation and migration of ECs into the tumor [5, 7, 14]. In addition, galectin-1 has been linked with reduction in the migration of lymphocytes, their trafficking to ECs and transendothelial infiltration into tumors [15, 16]. Previous studies have shown that by reducing galectin-1 expression or using a peptide such as anginex to inhibit CRD binding could inhibit endothelial function, as well as tumor growth and metastasis [4, 17, 18]. TDG has been more closely examined here as a small drug inhibitor of galectin-1 that increases the number of CD8+ lymphocytes infiltrating into tumors as well as suppressing tumor angiogenesis, most likely by preventing EC survival under conditions of oxidative stress.
Materials and methods
Cell lines and culture conditions
The murine melanoma B16F10 cell line, murine mammary carcinoma 4T1 cell line and human umbilical vein ECs (HUVECs) were maintained in DMEM supplemented with 10% heat-inactivated FBS, 50 IU/ml penicillin and streptomycin, 20 mM Hepes buffer, and 1.6 mM l-glutamate (Sigma). Human EAhy926 ECs were grown in DMEM containing HAT (hypoxanthine/aminopterin/thymidine) as previously described [19].
ELISA for detecting galectin-1 binding
96-well plates were pre-coated with mouse laminin (Invitrogen) in 0.2 M NaHCO3 at 1 μg/well. EAhy926 cells or HUVECs were fixed onto the wells by overnight incubation in 4% p-formaldehyde/PBS. After washing with PBS containing 0.05% Tween-20, plates were blocked with 3% BSA/PBS at 37°C for 1 h. Recombinant galectin-1 protein (see [20] and Supplemental data for method of preparation and Supplementary Fig. 1 for purity analysis) was pre-incubated with serial dilutions of TDG or sucrose (as a control disaccharide not binding the galectin-1 CRD) at 37°C for 1 h before testing for protein binding to the plates of laminin or cells. Samples were incubated at RT for 2 h, then washed before adding biotinylated anti-galectin-1 IgG. After incubating the plates at RT for 1 h, the unbound antibody was removed by washing. HRP streptavidin was added at RT for 1 h before final washing and addition of Lumigen® TMA-6 (GE Healthcare) for chemiluminescence and photon counting in a plate reader (FLUOstar Optima; BMG Labtech).
Tube forming assay
Ice-cold Matrigel™ (BD Biosciences) was added at 300 μl per well to pre-cooled 24-well plates. 50 μl of additional DMEM containing galectin-1 protein (wild type or P79R mutant; see Supplemental data for details of preparation and purity, Supplemental Fig. 1), TDG, or sucrose control were added to samples as indicated and the plates were kept at 37°C for 30 min. 5 × 105 EAhy926 cells or HUVECs were plated onto the gel surface in 200 μl of DMEM. After 18 h of culture, the cell rearrangement and tube formation were visualized by microscopy. The numbers of tubes and the interconnecting nodes were counted and individual tube lengths recorded.
Generation of galectin-1 knockdown (G1KD) tumor cell lines
pLKO.1-puro (Sigma–Aldrich) encoding a short hairpin RNA (shRNA) as an RNAi expressing vector was used with the targeting sequence for galectin-1: 5′-CCTGACCATCAAGCTGCCAGA-3′. The sequence of the non-target control shRNA was 5′-CAACAAGATGAAGAGCACCAA-3′. Viral supernatants were prepared by transient co-transfection of 293T cells (80% confluence) using CaCl2 and 20 μg of transfer plasmid (pLKO.1-puro, anti-galectin-1 or non-targeting control), 15 μg of packaging plasmid (pCMV-dR8.74) and 6 μg of envelop plasmid (pMD2.G). Media was replaced with supplemented DMEM after 8 h. Viral supernatants were collected after a further 48 h incubation and stored at −80°C until use. 5 μl of the viral stock was added to target cells in 96-well plates in 100 μl of DMEM containing 8 μg/ml of polybrene. After culturing for 24 h, cells were treated with puromycin to select for stable transfectants which were cloned as single colonies and galectin-1 expression analyzed by RT–PCR and immunoblotting.
Tumor mouse models and TDG treatment
Male C57BL/6, female Balb/c and female Balb/c nu/nu mice at 5–6 weeks of age were obtained from the Animal Resources Centre (Perth, WA, Australia). For all studies, aged, sex-matched groups of mice were used for the control and test cohorts. To establish primary solid tumors, B16F10 or 4T1 cells (7 × 105 cells/mouse in 150 μl of PBS) were implanted subcutaneously (s.c.) into the left chest region of C57BL/6 or Balb/c mice. Tumor cells were incubated with TDG (Carbosynth, UK) at 37°C for 1 h before s.c. injection as tumor challenge. After 3 days, mice received TDG (40, 80 and 120 mg/kg) by intratumoral injection which was repeated every 3 days. Tumor volumes were measured using the following formula: tumor volume = [longest diameter × (shortest diameter)2]/2 or by volumetric measurement using ultrasound (with an RMV704 scan head; mean frequency, 25 MHz; resolution, 40 μm; Vevo 770, VisualSonics). After 3 weeks, mice were sacrificed. All animal experiments were approved by the Griffith University animal ethics committee, and followed the procedures and guidelines set out by the Australian NHMRC and ANZCAART regarding animal welfare.
Cell preparation from excised tissues
Tumors were removed, cut into small pieces and incubated in DMEM containing 70 U/ml of collagenase (Sigma) at 37°C for 1 h before cells were washed and resuspended in PBS. Tumor infiltrating lymphocytes (TILs) were collected using Ficoll-Paque Plus (GE Healthcare). Blood was collected by cardiac puncture and peripheral blood mononuclear cells (PBMCs) isolated using Ficoll-Paque Plus. Spleens were removed and treated using 0.83% NH4Cl-Tris hemolysis buffer. The residual white blood cells were then analyzed by flow cytometry.
Three-dimensional power Doppler ultrasonography of tumors
Power Doppler ultrasound imaging of tumors was performed according to a previously published method [19]. Tumor bearing nude mice were anesthetized using isoflurane and the heart rate and body temperature were monitored during imaging by ultrasound. Two-dimensional images (2-D) were taken at 200 μm intervals and reconstituted to produce the final three-dimensional (3-D) volumetric images.
Statistical analysis
All values are expressed as mean ± SE, and the number (n) of samples used was as indicated. The statistical significance of differences between experimental and control groups was determined by Student’s t test with p-values < 0.05 considered significant. Two-way ANOVA with Bonferroni post-test analysis was performed for tumor growth experiments. All statistical analyses were performed using GraphPad Prism v4.03.
Results
Intratumoral treatment with TDG as a single agent suppresses tumor growth by inhibiting galectin-1
Our previous studies had shown that inhibiting galectin-1 using the non-metabolised disaccharide, thiodigalactoside (TDG), was effective as an adjuvant when added together with vaccine immunotherapy to promote anti-tumor CD8+ CTL effectors in vivo [21]. In the present study, TDG was examined as a single agent for its effects on the growth of the B16F10 melanoma and 4T1 mammary carcinoma as preclinical models of cancer. TDG, which had no effect on the growth, adhesion in culture or viability of the cancer cell lines growing in vitro (ref [21] and Supplemental Fig. 2A, B) was used to pre-treat the tumor cell burden before injection in order to block any endogenous galectin-1 presented by the cells during tumor establishment. The ensuing treatment then involved intratumoral TDG injection every 3 days for the duration of the experiments and was found to significantly reduce tumor growth in a dose-dependent manner in both cancer models (Fig. 1a–d). On day 18, the tumor volumes in animals treated with TDG at 120 mg/kg were 3.4-fold less for the melanoma and 2.2-fold less for the mammary carcinomas compared to the corresponding controls.
TDG suppresses B16F10 and 4T1 tumor growth in vivo. B16F10 or 4T1 cells were injected s.c. into C57BL/6 or Balb/c mice respectively. The mice were treated with intratumoral injections of TDG (40, 80 or 120 mg/kg), every 3 days and tumor volumes monitored (a B16F10, c 4T1). After 18 days, mice were sacrificed and tumor weights measured (b B16F10, d 4T1). Galectin-1 expression was knocked down using shRNA. e Levels of galectin-1 expressed in B16F10 and 4T1 cells were analyzed by western blotting and flow cytometry (f B16F10 and g 4T1). The G1KD B16F10 or 4T1 cells (7 × 105 cells/mouse) were injected s.c. into C57BL/6 or Balb/c mice respectively, and tumor volumes were monitored (h G1KD B16F10 and j G1KD 4T1). On day 28, the mice were sacrificed and the tumor weights were measured (i G1KD B16F10 and k G1KD 4T1). Three independent experiments were performed (total n = 7–9) and data represent the mean ± S.E. The statistical significance of the difference between groups compared was determined using students-t test: *p < 0.05, **p < 0.01, ***p < 0.001
Next, intratumoral TDG treatment was examined for its effect on the progression of tumors derived from the B16F10 and 4T1 cell lines in which galectin-1 expression had been knocked down (G1KD) by lentiviral infection with a galectin-1 specific shRNA-encoding vector. A slight increase in the levels of galectin-3 expression in the B16F10 and 4T1 G1KD cell lines was noted compared to the parental cells (Supplemental Fig. 2C). However, significantly reduced levels of the 14.5 kDa galectin-1 protein expression were obtained using the shRNA galectin-1 knock down vector and individual clones of B16F10 and 4T1 G1KD cell lines were selected (Fig. 1e). These findings were confirmed by quantitative analysis of intracellular levels of protein expression using flow cytometry whereas the plasmid carrying the non-silencing shRNA control (NC) showed only a slightly reduced galectin-1 protein expression (Fig. 1f, g). Again, an analysis of adding TDG, even up to high levels of 20 mg/ml, on the wild type or G1KD cancer cell lines growing in culture showed no effects on either proliferation or adhesion over several days in culture (Supplemental Fig. 2B). The G1KD B16F10 and 4T1 cells were implanted into C57BL/6 or Balb/c mice respectively and tumor growth was monitored. The growth rates of the G1KD tumors were considerably slower than those of the wild type tumors. Moreover, intratumoral TDG injection no longer affected the G1KD tumor growth analyzed by size and weight (Fig. 1h–k). Although no significant difference was found either by Mann–Whitney rank sum or students t test between treated and untreated G1KD tumors, the TDG treated tumors did show a clear trend with reduced weight suggesting a residual effect of TDG on the remaining galectin-1 produced by the G1KD tumors. This data provides support for galectin-1 as the major target for the effects of TDG on tumor growth.
Sucrose injected in the same manner as for TDG by intratumoral injection at the equivalent dose had no detectable effect on the tumor growth (Supplemental Fig. 3), indicating the effects of TDG were not due to an osmotic shock. This is also supported by the results in Supplemental Fig. 2B, because TDG or sucrose, even at 20 mg/ml, had no effect on the growth of the tumor cells in culture. The results indicating a remarkable and significantly reduced growth rate with the Gal-1 knock down cells were not due to clonal variation. In additional studies, G1KD pools of cells without clonal isolation as well as a distinct clone of 4T1 galectin-1 knockdown cells (indicated as G1KD pool and G1KD-2, respectively, in Supplemental Fig. 3, right hand panel) were tested by s.c. injection and tumor volumes were monitored. The results again showed that both G1KD pools and G1KD-clone 2 growth were also similarly delayed in growth in agreement with our previous results in Fig. 1. In addition, a scrambled shRNA transfected 4T1 cell control was tested and showed no significant effect on tumor growth.
Intratumoral TDG treatment promotes infiltration of CD8+ lymphocytes into tumors and reduces tumor angiogenesis in vivo
The effects of intratumoral TDG treatment on resident immune cell populations was investigated by immunohistochemistry. Of particular note, the levels of CD8+ lymphocytes in the immunostained sections derived from TDG treated tumors were markedly increased, with very few, if any, observed in sections from the untreated B16 or 4T1 tumors (Fig. 2a, b). In addition, numbers of CD8+ lymphocytes were found to be localised in the extravascular TDG treated tumor tissue, occurring in regions of tumor adjacent to the tumor vasculature, indicating increased tumor infiltration by these lymphocytes.
TDG regulates tumor angiogenesis and increases CD8+ lymphocyte infiltration into tumors. Frozen solid tumor tissues were sectioned followed by immunostaining with Alexa Fluor 488 anti-CD31 IgG (green), PE anti-CD8a IgG (red) and DAPI. a and b Vessel diameters and c green fluorescence intensity were analyzed (n = 5). d Wild type (left) or G1KD (right) tumor sections were stained with anti-CD31 IgG and anti-CD8a IgG. Data shown were representative of three independent experiments (n = 6–9). Scale bar 100 μm. Single tumor cell suspensions from tumors were stained with Alexa Fluor 488 anti-CD31 IgG and PE anti-CD8a IgG and analyzed by flow cytometry. e CD31+ and f CD8+ cells in wild type tumors. g CD31+ and h CD8+ cells in G1KD tumors. Three independent experiments were performed (n = 6–9) and percentages were normalized. The data represent the mean ± S.E. The statistical significance of the difference between samples compared was determined by students-t test: *p < 0.05, **p < 0.01
TDG treatment was found to cause marked changes in the tumor vessel networks within the treated tumors, particularly with the B16F10 melanoma where blood vessel diameters were considerably reduced in treated tumors (Fig. 2a, b). The average intensity of green fluorescence, indicating the levels of CD31+ as a marker of ECs, was also greatly reduced in both types of tumors treated with TDG (Fig. 2c) as was the degree of tumor vascularization observed in thin sections analyzed by immunohistochemistry in both of the treated tumor types (Fig. 2d). Examining the vasculature in the control tumors showed that B16F10 melanoma had obvious branched structures of larger vessel size (Fig. 2d) consistent with a previous report [22]. By contrast, the 4T1 tumors showed a more uniform bed of finer capillaries throughout the sections, with a more web-like appearance (Fig. 2d).
In order to quantify the findings more accurately, the changes in numbers of tumor infiltrating lymphocytes (TILs) and EC’s were measured using flow cytometry to analyse cell populations prepared from whole tumors. In both tumor types, a significant decrease in the percentages of cells that were CD31+, as a marker of ECs was detected (Fig. 2e) and this was associated with significantly increased levels of CD8+ lymphocytes in the TDG-treated B16F10 and 4T1 tumors (Fig. 2f). Isotype matched control antibodies showed no detectable background level of staining (Supplemental Fig. 4).
Previous reports had shown using galectin-1 knockout mice and anginex as a peptide affecting galectin-1 function, that host cell/EC derived galectin-1 was important for tumor angiogenesis [4], although targeting the role of tumor-derived galectin-1 had not been addressed. When tumors were established using G1KD cells, the differences in vascularization observed in thin sections comparing between control and TDG treated animals was much less pronounced (Fig. 2d). The significant increase in infiltration by CD8+ lymphocytes observed by immunohistochemistry in the TDG-treated sections from wild type tumors was not detected in the G1KD tumors (Fig. 2d) which also showed no significant differences in the CD31+ cell count between the control and TDG-treated tumor groups (Fig. 2g). In addition, TDG treatment did not significantly affect the CD8+ lymphocyte count in G1KD tumors detected by flow cytometric analyses (Fig. 2h).
A comparison of the relative populations of CD4+ and CD8+ lymphocytes in TILs, blood and spleen of the animals treated or not with TDG was undertaken on day 18 (Fig. 3). In addition to the increase in CD8+ lymphocyte numbers, the CD4+ lymphocytes among the TIL populations from the TDG treated B16F10 and 4T1 tumors were also increased, as was the trend in the CD4+ and CD8+ lymphocyte numbers in the blood and spleen, although differences in the blood and spleen of the control and TDG treated groups were not statistically significant. These data suggest that TDG treatment was promoting the infiltration of CD4+ and CD8+ T lymphocytes into the tumors as well as inhibiting tumor angiogenesis.
TDG increases the populations of CD4+ and CD8+ lymphocytes in vivo in tumor-burdened animals. Lymphocytes were prepared from the tumor tissue, blood and spleen of TDG treated or untreated mice and were stained with FITC-anti-CD4 IgG and PE-anti-CD8a IgG. The lymphocytes were gated in SSC-FSC plots and the ratios of numbers of cells in the CD4+ (X-axis) and CD8+ (Y-axis) cell populations were analyzed by flow cytometry. Data are representative of three independent experiments (n = 6–9)
Relative contribution of T cell immunity and anti-angiogenic effects of TDG determined by comparing wild type with immunocompromised mice
The above data indicated that TDG treatment affected tumor vascularization and increased the CD4+ and CD8+ lymphocyte populations of tumors in immunocompetent wild type mice (Figs. 2, 3). The extent of the specific contribution from T cell immunity versus the anti-angiogenic activity provided by blocking galectin-1 with TDG was examined by comparison with syngeneic Balb/c nude mice, defective in T cell immunity. Mice with tumors derived using the parental 4T1 cells were treated with TDG (120 mg/kg) injected every 3 days and this treatment suppressed the 4T1 tumor growth rate in nude mice (Fig. 4a, b), although the effects on both angiogenesis and tumor growth were not as remarkable as those obtained by TDG treatment of tumors in wild type Balb/c mice. A direct comparison of relative tumor growth at day 12 in treated versus untreated animals showed a 67% reduction with wild type Balb/c mice versus only a 47% reduction in the immunocompromised nude mice (Supplemental Fig. 5). Thus, these results suggest that TDG therapy has additive effects obtained on both angiogenesis and T cell immunity by blocking galectin-1.
TDG suppresses 4T1 growth and decreases tumor angiogenesis in nude mice. 4T1 cells were injected s.c. into syngeneic Balb/c nude mice. a Mice were treated with intratumoral TDG (120 mg/kg) every 3 days and tumor volumes were monitored. b Comparison of tumor weights measured at day 13. c Relative vascularization (%) in each tumor was estimated. d Single cell suspensions from tumors were stained with Alexa Fluor 488-anti-CD31 IgG and analyzed by flow cytometry. e 2-D (upper) and 3-D (lower) images of Doppler signals from intratumoral blood flow on days 6, 9 and 12 (n = 5). f Frozen tumor tissues were sectioned and stained with Alexa Fluor 488-anti-CD31 IgG (Green) and DAPI and in g levels of green fluorescence intensity was measured. Scale bar 100 μm. Three independent experiments were performed (total n = 9–10). The data represent the mean ± S.E. The statistical significance of the difference between samples compared was determined by students-t test, *p < 0.05, **p < 0.01, ***p < 0.001
The percent vascularization obtained by imaging tumor blood vessels using the ultrasound Power Doppler function directly showed significant differences in blood flows in treated tumors associated with considerable inhibition of tumor angiogenesis, particularly in the more vascularised peripheral regions of the tumors, as a result of treatment with TDG (Fig. 4c, e). Similarly, considerably decreased numbers of CD31+ cells existed in the treated tumors analyzed either by flow cytometry (Fig. 4d) or microscopic observations of immunostained sections from the TDG-treated tumors or by examining their average fluorescent intensity (Fig. 4f, g). Hence, a marked reduction in vascular structures and associated blood flow was observed in the TDG treated tumors.
TDG inhibits galectin-1 binding via the CRD to laminin and ECs
We next investigated the mechanisms of action of TDG in affecting EC function. Given that various types of tumor cells express and secrete considerable amounts of galectin-1 [23–25], it was important to determine first whether TDG would block galectin-1 binding to the surface of ECs. Thus, the ability of TDG to inhibit recombinant galectin-1 binding to laminin, a major component of endothelial basal membranes, as well as to the surface of the human ECs, EAhy926 and HUVECs was determined. The results showed that TDG dose-dependently inhibited galectin-1 binding to laminin and to the ECs, whereas sucrose (as a negative control disaccharide unable to bind galectin-1), was inactive (Fig. 5a). The inhibitory effects of TDG on galectin-1 binding to live ECs was also assessed by flow cytometry (Fig. 5b, c). A mutant form of galectin-1, P79R, with defective CRD function, was used as a negative control [26, 27] and exhibited a lack of binding capacity for laminin as well as low binding to the ECs compared to the wild type galectin-1 protein (Fig. 5a–c). Histogram profiles showed high binding levels of galectin-1 to the EAhy926 cells and HUVECs and that TDG significantly reduced the galectin-1 binding to these ECs (Fig. 5c). TDG further reduced the low levels of the mutant P79R binding to cells probably because the mutant protein retains some residual CRD binding capacity.
TDG inhibits galectin-1 binding to laminin and ECs. a TDG (0.5, 1.0 and 5.0 mg/ml) or sucrose (5 mg/ml) as shown was incubated with galectin-1 (100 μg/ml). Levels of galectin-1 binding to laminin or fixed ECs were detected by ELISA. b Purified P79R galectin-1 mutant protein (100 μg/ml) was applied to laminin coated plates. Levels of bound wild type or P79R mutant galectin-1 protein were measured by ELISA. c Live EAhy926 cells and HUVECs were treated with galectin-1 with or without TDG. After incubation for 1 h, the cells were fixed and galectin-1 levels binding to ECs were detected by flow cytometry (dotted line: isotype control). All procedures were performed at RT. Data represent the mean ± S.E. and the statistical significance of the difference from the corresponding controls was determined by students-t test: *p < 0.05, **p < 0.01, ***p < 0.001
TDG suppresses EC function in vitro
Next, the effect of TDG on the biological activities of ECs was investigated in vitro. Firstly, the ability of ECs to form tubes was assessed when grown in Matrigel. The number of tubes and interconnecting tube nodes were found to be increased by adding recombinant galectin-1 to cultures (Fig. 6a). However, TDG significantly reduced the number of tubes and tube nodes formed in the presence of added galectin-1. In contrast, adding the same levels of the P79R mutant galectin-1 protein (with defective CRD) failed to significantly alter the number of tubes or connected nodes compared to the controls with no added galectin-1 or containing sucrose (Fig. 6a). Addition of galectin-1 did not affect the average tube lengths of HUVECs, but slightly reduced the lengths of EAhy926 compared to controls and this reduction was inhibited by TDG (bottom bar graphs in Fig. 6a). We are unable to explain the reasons for why no change in HUVEC tube length was detected after adding Gal-1, despite increased numbers of nodes and tubes. The P79R mutant protein, albeit less noticeably, also reduced EAhy926 tube lengths and this reduction in tube length was prevented by the inclusion of either TDG or sucrose. The reasons for the unexpected result with EAhy926 cells and the mutant protein with or without sucrose as negative controls remains unresolved.
Galectin-1 increases endothelial function and TDG inhibits the galectin-1 effects in vitro. a and b Galectin-1 (100 μg/ml), P79R (100 μg/ml), TDG (1 mg/ml) or sucrose (1 mg/ml) were mixed in Matrigel. EAhy926 cells or HUVECs were seeded on top of the Matrigel. After incubation for 18 h, endothelial tube formation was imaged by microscopy and the number of tubes, connecting tube nodes and tube lengths were analyzed. Scale bar: 100 μm. c ECs were incubated with galectin-1 (200 μg/ml) and/or TDG (1 mg/ml). After incubation for 8 h, cell viability was measured by MTT assay. Data are representative of three independent experiments (n = 9) with mean values shown ± S.E. The statistical significance of the differences was determined by students-t test: * or † p < 0.05, ** or †† p < 0.01, *** or ††† p < 0.001 (*; versus control, †; versus respective groups)
The proliferation of both EAhy926 and HUVEC was enhanced by the addition of galectin-1 and this enhancement was inhibited by TDG (Fig. 6c). These findings show that galectin-1 promotes the tube-forming activity of ECs as well as their proliferation and these processes are dependent on the CRD binding site of galectin-1 because they were inhibited by TDG, which has a high affinity for binding to the galectin-1 CRD.
Inhibiting galectin-1 with TDG affects EC viability under conditions of oxidative stress
The tumor microenvironment frequently results in regions with high levels of oxidative stress leading to tumor necrosis and can also affect EC proliferation and migration, as well as causing their apoptosis [28]. Hypoxia and oxidative stress have been shown to promote HIF-1 stabilization and increase galectin-1 secretion by cancer cells [6]. Therefore the role of galectin-1 and its inhibition by TDG on EC viability and apoptosis was examined under conditions of oxidative stress induced by H2O2. EAhy926 cells, with their greater sensitivity to oxidative stress than HUVECs (Fig. 7a, b) were used for these studies and the addition of galectin-1 was found to protect against the cytotoxic effects of 10 μM H2O2 (Fig. 7a). However, addition of TDG suppressed the antioxidant protection mediated by galectin-1 on EAhy926 cell survival. Sucrose, as the control disaccharide, had no effect on the galectin-1 protective activity against H2O2. Next, the annexin V/PI method was used to measure levels of apoptotic EAhy926 cells when exposed to higher concentrations required to induce apoptosis (30 μM H2O2). The fraction of early apoptotic EAhy926 cells (annexin V+/PI−) present after 8–12 h of oxidative stress was markedly reduced when galectin-1 was included in the cultures (Fig. 7b). TDG was again found to suppress the protective effect of galectin-1 against the apoptosis induced by H2O2 (Fig. 7c) and the proportion of apoptotic EAhy926 cells induced by H2O2 was increased when TDG was included compared to the galectin-1 alone treated group.
Galectin-1 promotes EC survival against oxidative stress and TDG inhibits the antioxidant galectin-1 protective effect. EAhy926 cells treated with galectin-1 (200 μg/ml), TDG (1 mg/ml) and/or H2O2 (10 μM) as indicated were incubated for 2, 4 or 8 h. a Cell viability was measured by MTT assay. b and c Cells were stained with FITC-annexin V and PI, and analyzed by flow cytometry (X-axis; FITC-annexin V, Y-axis; PI). b Early apoptotic cells (annexin V+/PI−) in samples as a percent of the total cell number are presented in the bar graph. c Representative scatter plots from flow cytometric analyses. Two independent experiments (n = 6) were performed to obtain the data in b shown as the mean ± S.E. The statistical significance of the differences between groups compared were determined using students-t test: *p < 0.05, **p < 0.01 or † p < 0.05. d EAhy926 cells treated with conditioned media (CM) derived from confluent B16F10 or 4T1 tumor cell cultures, either wild type (WD) or G1KD as indicated. The conditioned media was added at 30% final concentration to the ECs and incubated for 12 h with or without TDG (1 mg/ml) and 10 mM H2O2 as shown. Cells were then stained with FITC-annexin V plus propidium iodide (PI), and analyzed by flow cytometry. Each scatter plot shows the average value for the gated annexin V+ cell population as % of total ± S.E. (n = 2)
The ability of galectin-1 endogenously produced from tumor cells in culture to protect against H2O2 induced EC apoptosis was assessed by adding conditioned media prepared from confluent cultures of the cancer cell lines to EAhy926 cell cultures (Fig. 7d). When conditioned media from the wild type B16F10 or 4T1 cell lines was added to a final concentration in the EC media of 30%, the levels of H2O2 induced EC apoptosis over 12 h incubation detected by FITC annexin-V+ staining was reduced from 24.55 to 17.25% and 21.55% respectively (p < 0.05). However, 30% conditioned media from the B16F10 or 4T1 G1KD cell lines was not as protective and H2O2 induced EC apoptosis was increased to 30.8% with the 4T1 G1KD media (p < 0.05). When the added 30% conditioned media also included TDG (1 mg/ml), this had little difference with the G1KD conditioned media but negated the protective effects of the conditioned media from the galectin-1 wild type cancer cells and the levels of H2O2 induced EC apoptosis were similar to the controls (Fig. 7d). These results are consistent with a protective effect provided by secreted galectin-1 from the tumor cells against oxidative stress.
Hence, galectin-1, which has been shown by us (Fig. 1e–g and ref [21]) and others [25, 29, 30] to be commonly expressed and secreted by tumor cells will act to protect ECs and promote their function in tumor tissues, particularly in regions of high oxidative stress known to be common in tumors [11]. However, TDG, is a suitable agent for blocking the protective functions of galectin-1 on ECs.
Discussion
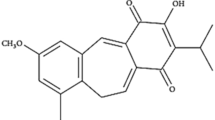
Galectins bind β-galactosides such as lactose, lactulose and N-acetyllactosamine (Galβ1,3/4GlcNAc) “LacNAc” with low inhibitory potency and K d values of ~1.0 and ~0.2 mM, respectively whereas natural disaccharides that are extended from the C3′ position of galactose, replacing the 3′-OH, showed enhanced affinity for some galectins [31]. Compared to the natural ligands such as those above, TDG (which we have used extensively here and elsewhere [1]), has advantages because it is readily available, has a higher affinity and Κ d of ~78 μM for galectin-1 and is a simple, synthetic and non-metabolizable disaccharide. TDG was very effective at suppressing tumor growth by inhibiting multiple tumor promoting and protective activities of tumor-derived galectin-1, including immune cell dysregulation, angiogenesis, and protection against oxidative stress. Indeed, intratumoral treatment with TDG significantly suppressed both melanoma and mammary carcinoma growth in mouse models, with much less effect observed for the G1KD tumors in which the protective functions of tumor-derived galectin-1 would be greatly reduced (Fig. 1). Therefore, our evidence strongly implicates TDG acting mainly by blocking the CRD of galectin-1 to exert its effects and interfere with the tumor-promoting and protective functions of the tumor-derived galectin-1 protein. Although a contribution of other galectins such as galectin-3 remains a possibility, our evidence, particularly based on the galectin-1 knockdown tumor studies, supports a key role for tumor derived galectin-1 in tumor development and makes the contributions of other members of the galectin family much less likely [32].
Perhaps most interestingly, one of the significant effects demonstrated here with intratumoral TDG treatment was the large increase in numbers of tumor-infiltrating CD4+ and CD8+ lymphocytes (Figs. 2, 3). Similarly, the populations of CD4+ and CD8+ lymphocytes in blood and spleen as immune organs were also increased following this treatment (Fig. 3).
We attempted to resolve the relative contribution mediated by the increased infiltration of the immune effector T cell populations versus the anti-angiogenic activity and which is the most important outcome that results from TDG inhibition of galectin-1 function. Thus, the comparison revealed that intratumoral TDG treatment suppressed tumor volume in nude mice by 47% versus the untreated control (Fig. 4), which was much less than the 67% reduction obtained when TDG was used to treat tumors in immunocompetent mice. These differences highlight the importance of T cell immunity and tumor infiltration by TILs to maximize the combined effects of TDG-mediated inhibition of galectin-1 function on both angiogenesis and immune activation. Supporting this viewpoint, our previous results [21] showed that TDG treatment promoted the induction of splenic-derived CD8+ CTL responses raised against breast cancer cells and slowed tumor progression. Hence, blocking galectin-1 induces greater anti-tumor effects by a combination of effects of modulating tumor neovascularization and promoting the infiltration of CD8+ T cells into the tumors.
The inhibitory effects of TDG on the pro-angiogenic function of galectin-1 were shown to be highly significant, both in vitro and in vivo, reducing binding to laminin and the tube-forming activity of ECs, as well as EC proliferation (Fig. 6). More importantly, our data provides a possible explanation for how TDG could act to inhibit the tumor protective function of galectin-1 in promoting survival of ECs subjected to tumor derived oxidative stress, with the result that TDG blocking galectin-1 would mean greater exposure to the tumor oxidative stress, enhancing the loss of EC by apoptosis (Fig. 7). This could explain the marked changes observed in the tumor vascular networks and the CD31+ EC populations within tumors, which were considerably reduced by intratumoral TDG treatment (Figs. 1, 2). In addition, we have for the first time shown considerable reductions in blood flow occurring within the TDG treated tumors, particularly in the highly vascularised periphery. These observations confirmed that TDG, as a single agent, inhibited tumor angiogenesis by blocking the functions of galectin-1 in promoting EC growth and survival and blood flow in our tumor models and presumably would do so in other tumors.
Anti-angiogenic therapy and immunotherapy are currently being used to improve the treatment of cancer patients. Enhancing immune responses by using cancer vaccines or adoptive transfer of ex vivo expanded immune cells has significantly progressed recently and several strategies are already being tested. Although tumor-specific T cells in the circulation can be effectively generated using these protocols, they have met with limited success with complete responses being uncommon [33]. Our results highlight that inhibiting galectin-1 function with TDG has multiple effects including promoting increased numbers of immune cells and their infiltration into tumors, apparently involving modifications to the tumor vasculature. Accumulating evidence suggests that the lack of correlation between the presence of circulating immunotherapy-induced lymphocytes and tumor regression is probably due to the restricted lymphocyte infiltration and recruitment caused by physical barriers associated with biologically aberrant tumor neovasculature [12, 34]. In order to evade immune cell infiltration, tumors decrease EC expression of adhesion molecules, such as ICAM-1, VCAM-1 and E-selectins, thereby preventing lymphocytes from trafficking into tumors [35, 36]. It has been shown that normalization of the aberrant tumor vasculature can increase tumor infiltration of cytotoxic T cells leading to enhanced survival of experimental animals [13]. In addition, administration of anti-vascular endothelial growth factor (VEGF) antibody to disrupt the VEGF/VEGFR-2 signaling axis increases the effects of adoptive T cell transfer therapy in the B16 murine melanoma model by normalizing the vasculature to allow T cell extravasation into the tumor stroma [37]. Therefore, for tumor immunotherapeutic strategies to be more effective, it may be beneficial to normalize their abnormal tumor blood vessels, perhaps using a drug such as anti-VEGF or TDG.
Galectin-1 is becoming widely recognized as an important lectin protein with significant roles in tumor progression and one of the roles of galectin-1 is its contribution to tumor cell evasion of immune cell surveillance [38, 39]. Galectin-1 has been shown to directly suppress T cell immunity by inducing T cell apoptosis [38], inhibiting T cell activation [40] and promoting regulatory T cell function [41]. In addition, we previously showed that blocking galectin-1 with TDG increased the induction of tumor-specific CD8+ T cell cytotoxicity, thereby suppressing growth of breast tumors in a murine model [21]. Therefore, blocking galectin-1 with metabolically stable disaccharides such as TDG should protect T cells from the negative impact of tumor derived galectin-1, and enhance T cell activity against many different types of cancers.
Another reason why galectin-1 is a promising new cancer target is because of its angiogenic promoting activities and its highly increased expression by tumors and tumor endothelium where elevated galectin-1 promotes EC proliferation and migration [7, 30]. Adding to this area, our results from the tube-forming assay using Matrigel and the MTT assay further advance understanding of the mechanisms whereby exogenous galectin-1 promotes angiogenesis by enhancing the tube-forming activity of ECs and their cell proliferation as observed with both EAhy926 and HUVECs (Fig. 6). These studies suggest that galectin-1 has an important function in cell to cell adhesion of ECs that is mediated by the CRD. Consistent with these reports and our results it appears that galectin-1 produced by tumors directly contributes to the formation of abnormal tumor vascular endothelium typifying the blood vessels in solid tumors as another of its tumor promoting functions. Thus, it was shown recently that tumor-derived and secreted galectin-1 is transported inside ECs where it specifically promotes H-Ras signaling, activating the Raf/mitogen-activated protein kinase/extracellular signal-regulated kinase (Erk) kinase (MEK)/Erk pathway to promote EC proliferation [14].
Hypoxia and oxidative stress are other important features of tumor microenvironments [11], where galectin-1 also plays a role as a well described hypoxia-inducible protein, mediated by the HIF-1 transcription factor [6, 29]. A poor blood supply due to the abnormal outgrowth of chaotically arranged blood vessels frequently results in regions of oxygen insufficiency within tumors. This promotes production of reactive oxygen species (ROS) [11] causing HIF-1 stabilization which in turn induces transcription of VEGF, the glucose transporter-1 (GLUT-1) and galectin-1 [6]. On the basis of our results, it is now clear that galectin-1 secretion by tumor cells will protect EC survival and promote their growth, reducing the levels of apoptosis caused by tumor-associated oxidative stress. Blocking the CRD of galectin-1 with TDG suppressed its protective effects against hydrogen peroxide-induced oxidative stress to ECs, and would promote vascular EC function within the tumor microenvironment. Given that the galectin-1 molecule contains six cysteine residues and is secreted from cells in the reduced form, perhaps galectin-1 could act as an antioxidant by conversion of its cysteines to sulfenic or sulfonic acids thereby absorbing ROS produced by tumors under oxidative stress [20, 42]. Certainly, our results showed that blocking the CRD of galectin-1 suppressed its protective effects against hydrogen peroxide-induced oxidative stress to ECs. However, the precise contributions of galectin-1 to the pro-angiogenic activities within tumor regions undergoing oxidative stress, including the relationship between the structures of reduced versus oxidized galectin-1 and biological actions of the galectin-1 CRD remain to be resolved.
Intensive chemical structural studies have been aimed at developing more effective and selective galectin inhibitors or their conjugates. Such compounds may produce stronger anti-tumor effects than the TDG disaccharide used here as proof-of-principle. For example, Nilsson et al. [43, 44] have developed TDG derivatives bearing aromatic amide substituents and aromatic lactose 2-O-ester derivatives with much lower K d values than the prototypic disaccharide used in our study. In addition, a β-sheet forming peptide-based galectin-1 antagonist has been shown to significantly suppress tumor angiogenesis [4, 45, 46]. Whether these compounds will prove to be effective and free of side effects in vivo remains to be demonstrated.
To conclude, our results emphasize the substantial promise of drugs such as TDG as inhibitors of galectin-1, an emerging target against cancer. Since galectin-1 is a multi-functional protein promoting tumor progression, such inhibitors should now be tested in clinical trials. In addition, the discovery that blocking galectin-1 function promotes T-cell infiltration into tumors supports the therapeutic potential for combining galectin-1 inhibitors as adjuvants to be used with immunotherapy and/or chemotherapy to improve existing cancer treatments.
References
Rabinovich GA (2005) Galectin-1 as a potential cancer target. Br J Cancer 92(7):1188–1192. doi:10.1038/sj.bjc.6602493
Camby I, Le Mercier M, Lefranc F, Kiss R (2006) Galectin-1: a small protein with major functions. Glycobiology 16(11):137R–157R. doi:10.1093/glycob/cwl025
Le Mercier M, Fortin S, Mathieu V, Roland I, Spiegl-Kreinecker S, Haibe-Kains B, Bontempi G, Decaestecker C, Berger W, Lefranc F, Kiss R (2009) Galectin 1 proangiogenic and promigratory effects in the Hs683 oligodendroglioma model are partly mediated through the control of BEX2 expression. Neoplasia 11(5):485–496
Thijssen VL, Postel R, Brandwijk RJ, Dings RP, Nesmelova I, Satijn S, Verhofstad N, Nakabeppu Y, Baum LG, Bakkers J, Mayo KH, Poirier F, Griffioen AW (2006) Galectin-1 is essential in tumor angiogenesis and is a target for antiangiogenesis therapy. Proc Natl Acad Sci USA 103(43):15975–15980. doi:10.1073/pnas.0603883103
Thijssen VL, Hulsmans S, Griffioen AW (2008) The galectin profile of the endothelium: altered expression and localization in activated and tumor endothelial cells. Am J Pathol 172(2):545–553. doi:10.2353/ajpath.2008.070938
Zhao XY, Chen TT, Xia L, Guo M, Xu Y, Yue F, Jiang Y, Chen GQ, Zhao KW (2010) Hypoxia inducible factor-1 mediates expression of galectin-1: the potential role in migration/invasion of colorectal cancer cells. Carcinogenesis 31(8):1367–1375. doi:10.1093/carcin/bgq116
Thijssen VL, Poirier F, Baum LG, Griffioen AW (2007) Galectins in the tumor endothelium: opportunities for combined cancer therapy. Blood 110(8):2819–2827. doi:10.1182/blood-2007-03-077792
Poyton RO, Castello PR, Ball KA, Woo DK, Pan N (2009) Mitochondria and hypoxic signaling: a new view. Ann NY Acad Sci 1177:48–56. doi:10.1111/j.1749-6632.2009.05046.x
Griffioen AW, Molema G (2000) Angiogenesis: potentials for pharmacologic intervention in the treatment of cancer, cardiovascular diseases, and chronic inflammation. Pharmacol Rev 52(2):237–268
Hanahan D, Folkman J (1996) Patterns and emerging mechanisms of the angiogenic switch during tumorigenesis. Cell 86(3):353–364. doi:S0092-8674(00)80108-7[pii]
Brown NS, Bicknell R (2001) Hypoxia and oxidative stress in breast cancer. Oxidative stress: its effects on the growth, metastatic potential and response to therapy of breast cancer. Breast Cancer Res 3(5):323–327
Castermans K, Griffioen AW (2007) Tumor blood vessels, a difficult hurdle for infiltrating leukocytes. Biochim Biophys Acta 1776(2):160–174. doi:10.1016/j.bbcan.2007.07.005
Hamzah J, Jugold M, Kiessling F, Rigby P, Manzur M, Marti HH, Rabie T, Kaden S, Grone HJ, Hammerling GJ, Arnold B, Ganss R (2008) Vascular normalization in Rgs5-deficient tumours promotes immune destruction. Nature 453(7193):410–414. doi:10.1038/nature06868
Thijssen VL, Barkan B, Shoji H, Aries IM, Mathieu V, Deltour L, Hackeng TM, Kiss R, Kloog Y, Poirier F, Griffioen AW (2010) Tumor cells secrete galectin-1 to enhance endothelial cell activity. Cancer Res 70(15):6216–6224. doi:10.1158/0008-5472.CAN-09-4150
He J, Baum LG (2006) Endothelial cell expression of galectin-1 induced by prostate cancer cells inhibits T-cell transendothelial migration. Lab Invest 86(6):578–590. doi:10.1038/labinvest.3700420
Norling LV, Sampaio AL, Cooper D, Perretti M (2008) Inhibitory control of endothelial galectin-1 on in vitro and in vivo lymphocyte trafficking. FASEB J 22(3):682–690. doi:10.1096/fj.07-9268com
Mathieu V, Le Mercier M, De Neve N, Sauvage S, Gras T, Roland I, Lefranc F, Kiss R (2007) Galectin-1 knockdown increases sensitivity to temozolomide in a B16F10 mouse metastatic melanoma model. J Invest Dermatol 127(10):2399–2410. doi:10.1038/sj.jid.5700869
Le Mercier M, Mathieu V, Haibe-Kains B, Bontempi G, Mijatovic T, Decaestecker C, Kiss R, Lefranc F (2008) Knocking down galectin 1 in human hs683 glioblastoma cells impairs both angiogenesis and endoplasmic reticulum stress responses. J Neuropathol Exp Neurol 67(5):456–469. doi:10.1097/NEN.0b013e318170f892
Dong LF, Swettenham E, Eliasson J, Wang XF, Gold M, Medunic Y, Stantic M, Low P, Prochazka L, Witting PK, Turanek J, Akporiaye ET, Ralph SJ, Neuzil J (2007) Vitamin E analogues inhibit angiogenesis by selective induction of apoptosis in proliferating endothelial cells: the role of oxidative stress. Cancer Res 67(24):11906–11913. doi:10.1158/0008-5472.CAN-07-3034
Scott SA, Bugarcic A, Blanchard H (2009) Characterisation of oxidized recombinant human galectin-1. Protein Pept Lett 16(10):1249–1255
Stannard KA, Collins PM, Ito K, Sullivan EM, Scott SA, Gabutero E, Darren Grice I, Low P, Nilsson UJ, Leffler H, Blanchard H, Ralph SJ (2010) Galectin inhibitory disaccharides promote tumour immunity in a breast cancer model. Cancer Lett 299(2):95–110. doi:10.1016/j.canlet.2010.08.005
Solesvik OV, Rofstad EK, Brustad T (1984) Vascular changes in a human malignant melanoma xenograft following single-dose irradiation. Radiat Res 98(1):115–128
Saussez S, Glinoer D, Chantrain G, Pattou F, Carnaille B, Andre S, Gabius HJ, Laurent G (2008) Serum galectin-1 and galectin-3 levels in benign and malignant nodular thyroid disease. Thyroid 18(7):705–712. doi:10.1089/thy.2007.0361
Saussez S, Lorfevre F, Lequeux T, Laurent G, Chantrain G, Vertongen F, Toubeau G, Decaestecker C, Kiss R (2008) The determination of the levels of circulating galectin-1 and-3 in HNSCC patients could be used to monitor tumor progression and/or responses to therapy. Oral Oncol 44(1):86–93. doi:10.1016/j.oraloncology.2006.12.014
Demydenko D, Berest I (2009) Expression of galectin-1 in malignant tumors. Exp Oncol 31(2):74–79. doi:39/752[pii]
Scott K, Zhang J (2002) Partial identification by site-directed mutagenesis of a cell growth inhibitory site on the human galectin-1 molecule. BMC Cell Biol 3:3
Scott K, Weinberg C (2004) Galectin-1: a bifunctional regulator of cellular proliferation. Glycoconj J 19(7–9):467–477. doi:10.1023/B:GLYC.0000014076.43288.89
Ran S, Downes A, Thorpe PE (2002) Increased exposure of anionic phospholipids on the surface of tumor blood vessels. Cancer Res 62(21):6132–6140
Le QT, Shi G, Cao H, Nelson DW, Wang Y, Chen EY, Zhao S, Kong C, Richardson D, O’Byrne KJ, Giaccia AJ, Koong AC (2005) Galectin-1: a link between tumor hypoxia and tumor immune privilege. J Clin Oncol 23(35):8932–8941. doi:10.1200/JCO.2005.02.0206
Chiang WF, Liu SY, Fang LY, Lin CN, Wu MH, Chen YC, Chen YL, Jin YT (2008) Overexpression of galectin-1 at the tumor invasion front is associated with poor prognosis in early-stage oral squamous cell carcinoma. Oral Oncol 44(4):325–334. doi:10.1016/j.oraloncology.2007.03.004
Cumpstey I, Sundin A, Leffler H, Nilsson UJ (2005) C2-symmetrical thiodigalactoside bis-benzamido derivatives as high-affinity inhibitors of galectin-3: efficient lectin inhibition through double arginine-arene interactions. Angew Chem Int Ed Engl 44(32):5110–5112. doi:10.1002/anie.200500627
Liu FT, Rabinovich GA (2005) Galectins as modulators of tumour progression. Nat Rev Cancer 5(1):29–41. doi:10.1038/nrc1527
Appay V, Jandus C, Voelter V, Reynard S, Coupland SE, Rimoldi D, Lienard D, Guillaume P, Krieg AM, Cerottini JC, Romero P, Leyvraz S, Rufer N, Speiser DE (2006) New generation vaccine induces effective melanoma-specific CD8 + T cells in the circulation but not in the tumor site. J Immunol 177(3):1670–1678. doi:177/3/1670[pii]
Chen Q, Wang WC, Evans SS (2003) Tumor microvasculature as a barrier to antitumor immunity. Cancer Immunol Immunother 52(11):670–679. doi:10.1007/s00262-003-0425-4
Griffioen AW (2008) Anti-angiogenesis: making the tumor vulnerable to the immune system. Cancer Immunol Immunother 57(10):1553–1558. doi:10.1007/s00262-008-0524-3
Dirkx AE, Oude Egbrink MG, Kuijpers MJ, van der Niet ST, Heijnen VV, Bouma-ter Steege JC, Wagstaff J, Griffioen AW (2003) Tumor angiogenesis modulates leukocyte-vessel wall interactions in vivo by reducing endothelial adhesion molecule expression. Cancer Res 63(9):2322–2329
Shrimali RK, Yu Z, Theoret MR, Chinnasamy D, Restifo NP, Rosenberg SA (2010) Antiangiogenic agents can increase lymphocyte infiltration into tumor and enhance the effectiveness of adoptive immunotherapy of cancer. Cancer Res 70(15):6171–6180. doi:10.1158/0008-5472.CAN-10-0153
Rubinstein N, Alvarez M, Zwirner NW, Toscano MA, Ilarregui JM, Bravo A, Mordoh J, Fainboim L, Podhajcer OL, Rabinovich GA (2004) Targeted inhibition of galectin-1 gene expression in tumor cells results in heightened T cell-mediated rejection; a potential mechanism of tumor-immune privilege. Cancer Cell 5(3):241–251. doi:S1535610804000248[pii]
Salatino M, Croci DO, Bianco GA, Ilarregui JM, Toscano MA, Rabinovich GA (2008) Galectin-1 as a potential therapeutic target in autoimmune disorders and cancer. Expert Opin Biol Ther 8(1):45–57. doi:10.1517/14712598.8.1.45
Chung CD, Patel VP, Moran M, Lewis LA, Miceli MC (2000) Galectin-1 induces partial TCR zeta-chain phosphorylation and antagonizes processive TCR signal transduction. J Immunol 165(7):3722–3729
Garin MI, Chu CC, Golshayan D, Cernuda-Morollon E, Wait R, Lechler RI (2007) Galectin-1: a key effector of regulation mediated by CD4 + CD25 + T cells. Blood 109(5):2058–2065. doi:10.1182/blood-2006-04-016451
Inagaki Y, Sohma Y, Horie H, Nozawa R, Kadoya T (2000) Oxidized galectin-1 promotes axonal regeneration in peripheral nerves but does not possess lectin properties. Eur J Biochem 267(10):2955–2964. doi:ejb1311[pii]
Cumpstey I, Salomonsson E, Sundin A, Leffler H, Nilsson UJ (2007) Studies of arginine-arene interactions through synthesis and evaluation of a series of galectin-binding aromatic lactose esters. Chembiochem 8(12):1389–1398. doi:10.1002/cbic.200700040
Delaine T, Cumpstey I, Ingrassia L, Le Mercier M, Okechukwu P, Leffler H, Kiss R, Nilsson UJ (2008) Galectin-inhibitory thiodigalactoside ester derivatives have antimigratory effects in cultured lung and prostate cancer cells. J Med Chem 51(24):8109–8114. doi:10.1021/jm801077j
Griffioen AW, van der Schaft DW, Barendsz-Janson AF, Cox A, Struijker Boudier HA, Hillen HF, Mayo KH (2001) Anginex, a designed peptide that inhibits angiogenesis. Biochem J 354(Pt 2):233–242
Dings RP, van der Schaft DW, Hargittai B, Haseman J, Griffioen AW, Mayo KH (2003) Anti-tumor activity of the novel angiogenesis inhibitor anginex. Cancer Lett 194(1):55–66. doi:S0304383503000156[pii]
Acknowledgments
The authors acknowledge Dr Ken Scott (University of Auckland, NZ) for contributing the mutant galectin-1 protein expression construct. We also thank Prof. R.K. Ralph, Dr Andy Wu and Dr Yuki Masuda for help in editing the manuscript and Dr Pauline Low and Dr Wendy Kelly for technical support. This study was supported by grant funding from the Cancer Council Queensland, Australia and from the Neumedix Health Group.
Conflict of interest
No conflicts of interest by any of the authors.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Ito, K., Scott, S.A., Cutler, S. et al. Thiodigalactoside inhibits murine cancers by concurrently blocking effects of galectin-1 on immune dysregulation, angiogenesis and protection against oxidative stress. Angiogenesis 14, 293–307 (2011). https://doi.org/10.1007/s10456-011-9213-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10456-011-9213-5