Abstract
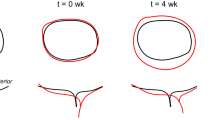
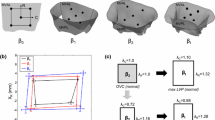
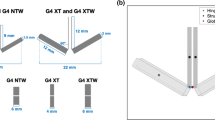
Though mitral valve (MV) repair surgical procedures have increased in the United States [Gammie, J. S., et al. Ann. Thorac. Surg. 87(5):1431–1437, 2009; Nowicki, E. R., et al. Am. Heart J. 145(6):1058–1062, 2003], studies suggest that altering MV stress states may have an effect on tissue homeostasis, which could impact the long-term outcome [Accola, K. D., et al. Ann. Thorac. Surg. 79(4):1276–1283, 2005; Fasol, R., et al. Ann. Thorac. Surg. 77(6):1985–1988, 2004; Flameng, W., P. Herijgers, and K. Bogaerts. Circulation 107(12):1609–1613, 2003; Gillinov, A. M., et al. Ann. Thorac. Surg. 69(3):717–721, 2000]. Improved computational modeling that incorporates structural and geometrical data as well as cellular components has the potential to predict such changes; however, the absence of important boundary condition information limits current efforts. In this study, novel high definition in vivo annular kinematic data collected from surgically implanted sonocrystals in sheep was fit to a contiguous 3D spline based on quintic-order hermite shape functions with C2 continuity. From the interpolated displacements, the annular axial strain and strain rate, bending, and twist along the entire annulus were calculated over the cardiac cycle. Axial strain was shown to be regionally and temporally variant with minimum and maximum values of −10 and 4%, respectively, observed. Similarly, regionally and temporally variant strain rate values, up to 100%/s contraction and 120%/s elongation, were observed. Both annular bend and twist data showed little deviation from unity with limited regional variations, indicating that most of the energy for deformation was associated with annular axial strain. The regionally and temporally variant strain/strain rate behavior of the annulus are related to the varied fibrous-muscle structure and contractile behavior of the annulus and surrounding ventricular structures, although specific details are still unavailable. With the high resolution shape and displacement information described in this work, high fidelity boundary conditions can be prescribed in future MV finite element models, leading to new insights into MV function and strategies for repair.









Similar content being viewed by others
References
Accola, K. D., et al. Midterm outcomes using the physio ring in mitral valve reconstruction: experience in 492 patients. Ann. Thorac. Surg. 79(4):1276–1283, 2005; discussion 1276–1283.
Ahmad, R. M., et al. Annular geometry and motion in human ischemic mitral regurgitation: novel assessment with three-dimensional echocardiography and computer reconstruction. Ann. Thorac. Surg. 78(6):2063–2068, 2004; discussion 2068.
Anderson, R. H., et al. The myth of the aortic annulus: the anatomy of the subaortic outflow tract. Ann. Thorac. Surg. 52(3):640–646, 1991.
Black, M. M., et al. A three-dimensional analysis of a bioprosthetic heart valve. J. Biomech. 24:793–801, 1991.
Braunberger, E., et al. Very long-term results (more than 20 years) of valve repair with Carpentier’s techniques in nonrheumatic mitral valve insufficiency. Circulation 104(12 Suppl 1):I8–I11, 2001.
Burriesci, G., I. C. Howard, and E. A. Patterson. Influence of anisotropy on the mechanical behaviour of bioprosthetic heart valves. J. Med. Eng. Technol. 23(6):203–215, 1999.
Cacciola, G., G. W. Peters, and F. P. Baaijens. A synthetic fiber-reinforced stentless heart valve. J. Biomech. 33(6):653–658, 2000.
Cacciola, G., G. W. Peters, and P. J. Schreurs. A three-dimensional mechanical analysis of a stentless fibre-reinforced aortic valve prosthesis. J. Biomech. 33(5):521–530, 2000.
Caiani, E. G., et al. Evaluation of alterations on mitral annulus velocities, strain, and strain rates due to abrupt changes in preload elicited by parabolic flight. J. Appl. Physiol. 103(1):80–87, 2007.
Carpentier, A. Reconstructive valvuloplasty. A new technique of mitral valvuloplasty. Presse Med. 77(7):251–253, 1969.
Fasol, R., et al. Mitral valve repair with the Colvin-Galloway Future Band. Ann. Thorac. Surg. 77(6):1985–1988, 2004; discussion 1988.
Filip, D. A., A. Radu, and M. Simionescu. Interstitial cells of the heart valve possess characteristics similar to smooth muscle cells. Circ. Res. 59(3):310–320, 1986.
Flameng, W., P. Herijgers, and K. Bogaerts. Recurrence of mitral valve regurgitation after mitral valve repair in degenerative valve disease. Circulation 107(12):1609–1613, 2003.
Gammie, J. S., et al. Trends in mitral valve surgery in the United States: results from the Society of Thoracic Surgeons Adult Cardiac Surgery Database. Ann. Thorac. Surg. 87(5):1431–1437, 2009; discussion 1437–1439.
George, K., et al. Mitral annular myocardial velocity assessment of segmental left ventricular diastolic function after prolonged exercise in humans. J. Physiol. 569(Pt 1):305–313, 2005; (Epub 2005 Aug 18).
Gillinov, A. M., et al. Durability of mitral valve repair for degenerative disease. J. Thorac. Cardiovasc. Surg. 116(5):734–743, 1998.
Gillinov, A. M., et al. Cosgrove-Edwards Annuloplasty System: midterm results. Ann. Thorac. Surg. 69(3):717–721, 2000.
Goldsmith, I. R., G. Y. Lip, and R. L. Patel. A prospective study of changes in the quality of life of patients following mitral valve repair and replacement. Eur. J. Cardiothorac. Surg. 20(5):949–955, 2001.
Gorman, 3rd, J. H., et al. Dynamic three-dimensional imaging of the mitral valve and left ventricle by rapid sonomicrometry array localization. J. Thorac. Cardiovasc. Surg. 112(3):712–726, 1996.
Gould, P. L., et al. Stress analysis of the human aortic valve. Comput. Struct. 3:377, 1973.
Hamid, M. S., H. N. Sabbah, and P. D. Stein. Influence of stent height upon stresses on the cusps of closed bioprosthetic valves. J. Biomech. 19:759–769, 1986.
Hashima, A. R., et al. Nonhomogeneous analysis of epicardial strain distributions during acute myocardial ischemia in the dog. J. Biomech. 26:19–35, 1993.
Hayashi, S. Y., et al. Analysis of mitral annulus motion measurements derived from M-mode, anatomic M-mode, tissue Doppler displacement, and 2-dimensional strain imaging. J. Am. Soc. Echocardiogr. 19(9):1092–1101, 2006.
Hinton, E., and D. R. J. Owen. An Introduction to Finite Element Computations (1st ed.). Swansea, UK: Pineridge Press Limited, p. 385, 1979
Ho, S. Y. Anatomy of the mitral valve. Heart 88(Suppl 4):iv5–iv10, 2002.
Huang, X., et al. A two dimensional finite element analysis of a bioprosthetic heart valve. J. Biomech. 23:753–762, 1990.
Krucinski, S., et al. Numerical simulation of leaflet flexure in bioprosthetic valves mounted on rigid and expansile stents. J. Biomech. 26:929–943, 1993.
Kunzelman, K. S., M. S. Reimink, and R. P. Cochran. Annular dilatation increases stress in the mitral valve and delays coaptation: a finite element computer model. Cardiovasc. Surg. 5(4):427–434, 1997.
Kunzelman, K. S., M. S. Reimink, and R. P. Cochran. Variations in annuloplasty ring and sizer dimensions may alter outcome in mitral valve repair. J. Card. Surg. 12(5):322–329, 1997.
Leat, M. E., and J. Fisher. Comparative study of the function of the Abiomed polyurethane heart valve for use in left ventricular assist devices. J. Biomed. Eng. 15(6):516–520, 1993.
Li, J., X. Y. Luo, and Z. B. Kuang. A nonlinear anisotropic model for porcine aortic heart valves. J. Biomech. 34(10):1279–1289, 2001.
Messier, Jr., R. H., et al. Dual structural and functional phenotypes of the porcine aortic valve interstitial population: characteristics of the leaflet myofibroblast. J. Surg. Res. 57(1):1–21, 1994.
Mulholland, D. L., and A. I. Gotlieb. Cell biology of valvular interstitial cells. Can. J. Cardiol. 12(3):231–236, 1996.
Nowicki, E. R., et al. Mitral valve repair and replacement in northern New England. Am. Heart J. 145(6):1058–1062, 2003.
Quick, D. W., et al. Collagen synthesis is upregulated in mitral valves subjected to altered stress. ASAIO J. 43(3):181–186, 1997.
Rabkin, E., et al. Evolution of cell phenotype and extracellular matrix in tissue-engineered heart valves during in vitro maturation and in vivo remodeling. J. Heart Valve Dis. 11(3):308–314, 2002; discussion 314.
Rabkin-Aikawa, E., et al. Dynamic and reversible changes of interstitial cell phenotype during remodeling of cardiac valves. J. Heart Valve Dis. 13(5):841–847, 2004.
Sacks, M. S., et al. In vivo dynamic deformation of the mitral valve anterior leaflet. Ann. Thorac. Surg. 82(4):1369–1377, 2006.
Sacks, M. S., et al. In vivo biomechanical assessment of trigycidylamine crosslinked pericardium. Biomaterials 28(35):5390–5398, 2007.
Salgo, I. S., et al. Effect of annular shape on leaflet curvature in reducing mitral leaflet stress. Circulation 106(6):711–717, 2002.
Sands, M. P., et al. An anatomical comparison of human pig, calf, and sheep aortic valves. Ann. Thorac. Surg. 8(5):407–414, 1969.
Smith, D. B., et al. Surface geometric analysis of anatomic structures using biquintic finite element interpolation. Ann. Biomed. Eng. 28(6):598–611, 2000.
Stoylen, A., et al. Strain rate imaging in normal and reduced diastolic function: comparison with pulsed Doppler tissue imaging of the mitral annulus. J. Am. Soc. Echocardiogr. 14(4):264–274, 2001.
Sun, W., A. Abad, and M. S. Sacks. Simulated bioprosthetic heart valve deformation under quasi-static loading. J. Biomech. Eng. 127(6):905–914, 2005.
Taylor, P. M., et al. The cardiac valve interstitial cell. Int. J. Biochem. Cell Biol. 35(2):113–118, 2003.
Timek, T. A., et al. Aorto-mitral annular dynamics. Ann. Thorac. Surg. 76(6):1944–1950, 2003.
Yacoub, M., et al. Surgical treatment of mitral regurgitation caused by floppy valves: repair versus replacement. Circulation 64(2 Pt 2):II210–II216, 1981.
Young, A. A., P. J. Hunter, and B. H. Smaill. Estimation of epicardial strain using the motions of coronary bifurcations in biplane cineangiography. IEEE Trans. Biomed. Eng. 39(5):526–531, 1992.
Acknowledgments
This work was made possible by NIH Grant HL-073021NIH, an American Heart Association Pre-Doctoral Fellowship (CEE), the NIH/NIBIB T32 “Biomechanics in Regenerative Medicine” training Grant (NIBIB T32 EB003392-01).
Author information
Authors and Affiliations
Corresponding author
Additional information
Chad Eckert and Brett Zubiate contributed equally to this work.
Appendix
Appendix
Appendix A—Quintic Hermite Shape Functions
The six shape functions \( N_{\alpha }^{i} \) of the 1D quintic finite element used in this study are defined as follows24:
where the subscript indicates the node number, the superscript the order of the derivative with respect to the local coordinate ξ, and the coordinate values at nodes 1 and 2 are −1 and 1, respectively.
Appendix B—Generalized Least Squares Regression
With the data properly oriented, the parameter estimation for the interpolation is done using the general matrix formulation for linear least squares. The function describing the component being fit is defined by:
where e is error and [a] is a vector containing the nodal fit parameters for the function f. Expressed in matrix form the relationship can be written concisely as:
In this case, f is the component of the data being fit (r(θ) or z(θ)) and e is the error associated with the fit at a given point. The rows of matrix [ψ] are the shape functions evaluated at there isoparametric coordinate corresponding to the data point observed. It can be shown that the minimization of the sum square of errors associated with the partial derivatives of f with respect to each of the parameters can be reduced to the following expression:
So the parameters are computed by simply inverting [ψ]T [ψ] and left multiplying both sides of the equation. After estimating the parameters for each element, the curve can be interpolated by evaluating the polynomials for each element at any point within the domain. In the case of smoothing via the Sobolev algorithm, the Sobolev penalty function is added to the matrix [ψ]T [ψ]. The nodal parameters for the smoothed fit are computed using:
The described general matrix formulation for linear least squares is then used in the same manner to determine the parameters for each element.
Rights and permissions
About this article
Cite this article
Eckert, C.E., Zubiate, B., Vergnat, M. et al. In Vivo Dynamic Deformation of the Mitral Valve Annulus. Ann Biomed Eng 37, 1757–1771 (2009). https://doi.org/10.1007/s10439-009-9749-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10439-009-9749-3