Abstract
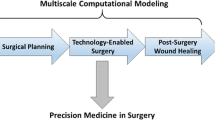
This paper discusses some of the concept of modeling surgery outcome. It is also an attempt to offer a road map for progress. This paper may serve as a common ground of discussion for both communities i.e surgeons and computational scientist in its broadest sense. Predicting surgery outcome is a very difficult task. All patients are different, and multiple factors such as genetic, or environment conditions plays a role. The difficulty is to construct models that are complex enough to address some of these significant multiscale elements and simple enough to be used in clinical conditions and calibrated on patient data. We will provide a multilevel progressive approach inspired by two applications in surgery that we have been working on. One is about vein graft adaptation after a transplantation, the other is the recovery of cosmesis outcome after a breast lumpectomy. This work, that is still very much in progress, may teach us some lessons. We are convinced that the digital revolution that is transforming the working environment of the surgeon makes closer collaboration between surgeons and computational scientist unavoidable. We believe that “computational surgery” will allow the community to develop predictive model of the surgery outcome and greatprogresses in surgery procedures that goes far beyond the operating room procedural aspect.
Similar content being viewed by others
References
LeRoy Heinrichs, W., Srivastava, S., Montgomery, K., et al.: The fundamental manipulations of surgery: a structured vocabulary for designing surgical curricula and simulators. The Journal of the American Association of Gynecologic Laparoscopists 11, 450–456 (2004)
de Bissy, F., et Guerrand, R. H.: Ambroise Paré, Oeuvres completes remises en ordre et en francais moderne, Union latine del’edition, 3 tomes et un index (1983)
Chaplain, M. A. J.: Modelling aspects of cancer growth: Insight from mathematical and numerical analysis and computational simulation. Multiscale Problems in the Life Sciences, Lecture Note in Mathematics 1940, 147–200 (2008)
Cristini, V., Lowengrub, J.: Multiscale Modeling of Cancer: an Integrated Experimental and Mathematical Modeling Approach. Cambrdge University Press (2010)
Rockne, R., Rockhill, J. K., Mrugala, M., et al.: Predicting the efficacy of radiotherapy in individual glioblastoma patients in vivo: a mathematical modelling approach. Physics in Medicine and Biology, 55, 3271–3285 (2010)
Swanson, K. R., Alvord Jr. E. C., Murray, J. D.: A quantitative model for differential motility of gliomas in grey and white matter. Cell Proliferation 33, 317–329 (2000)
Wang, C., Rockhill, J. K., Mrugala, M., et al.: Prognostic significance of growth kinetics in newly diagnosed glioblastomas revealed by combining serial imaging with a novel biomathematical model. Cancer Research 69, 9133–9140 (2009)
Campbell, A., Sivakumaran, T., Davidson, M., et al.: Mathematical modeling of liver metastases tumour growth and control with radiotherapy. Phys. Med. Biol. 53, 7225–7239 (2008)
Furchtgott, L. A., Chow, C. C., Vipul, P.: A model of liver regeneration. Biophysical Journal Volume 96, 3926–3935 (2009)
Hoehme, S., Brulport, M., Bauer, A., et al.: Prediction and validation of cell alignment along microvessels as order principle to restore tissue architecture in liver regeneration. Proc. Natl. Acad. Sci. (USA) 107, 10371–10376 (2010)
Berceli, S. A., Tran-Son-Tay, R., Garbey, M. et al.: Hemodynamically driven vein graft remodeling: a systems biology approach. Vascular 17, 24–31 (2009)
Fitzgibbon, G. M., Kafka, H. P., Leach, A. J., et al.: Coronary bypass graft fate and patient outcome: Angiographic follow-up of 5,065 grafts related to survival and reoperation in 1388 patients during 25 years. J. Am. Coll. Cardiol. 28, 616–626 (1996)
Dobrin, P. B., Littooy, F. N., Endean, E. D.: Mechanical factors predisposing to intimal hyperplasia and medial thickening in autogenous vein grafts. Surgery 105, 393–400 (1989)
Fillinger, M. F., Cronenwett, J. L., Besso, S., et al.: Vein adaptation to the hemodynamic environment of infrainguinal grafts. J. Vasc. Surg. 19, 970–979 (1994)
Galt, S. W., Zwolak, R. M., Wagner, R. J., et al.: Differential response of arteries and vein grafts to blood flow reduction. J. Vasc. Surg. 17, 563–570 (1993)
Mills, J. L., Bandyk, D. F., Gahtan, V., et al.: The origin of infrainguinal vein graft stenosis: A prospective study based on duplex surveillance, J. Vasc. Surg. 21, 16–25 (1995)
Varty, K., Allen, K. E., Bell, P. R. F., et al.: Infrainguinal vein graft stenosis. Br. J. Surg. 80, 825–833 (1993)
Zwolak, R. M., Adams, M. C, Clowes, A. W.: Kinetics of vein graft hyperplasia: Association with tangential stress. J. Vasc. Surg. 5, 126–136 (1987)
Berceli, S. A., Davies, M. G., Kenagy, R. D., et al.: Flow-induced neointimal regression in baboon polytetrafluoroethylene grafts is associated with decreased cell proliferation and increased apoptosis. Journal of Vascular Surgery 36, 1248–1255 (2002)
Furuyama, T., Komori, K., Shimokawa, H., et al.: Long-term inhibition of Rho kinase suppresses intimal thickening in autologous vein grafts in rabbits. Journal of Vascular Surgery 43, 1249–1256 (2006)
Jiang, Z., Wu, L., Miller, B. L., et al.: A novel vein graft model: adaptation to differential flow environments. American Journal of Physiology — Heart and Circulatory Physiology 286, H240–H245 (2004)
Jiang, Z., Tao, M., Omalley, K. A., et al.: Established neointimal hyperplasia in vein grafts expands via TGF-β-mediated progressive fibrosis. American Journal of Physiology - Heart and Circulatory Physiology 297, H1200–H1207 (2009)
Hoch, J. R., Stark, V. K., Rooijen, N,, et al.: Macrophage depletion alters vein graft intimal hyperplasia. Surgery 126, 428–437 (1999)
Bass, B. L., Garbey, M.: Breast conservative therapy for breast cancer: targets for investigation to improve results, In: Garbey, M., Bass, B. L., Collet, C., et al., eds. Computational Surgery and Dual Training. Springer, New York (2010)
Thanoon, D., Garbey, M., Kim, N. H., et al.: a computational framework for breast surgery: application to breast conserving therapy, In Garbey, M., Bass, B., De Matelin, M., et al. eds. Computational Surgery and Dual Training, Springer Verlag, 249–268 (2009)
Whelan, T. J., Levine, M., Julian, J., et al.: The effects of radiation therapy on quality of life of women with breast carcinoma: Results of a randomized trial. American Cancer Society 88, 2260–2266 (2000)
Budrukkar, A., Sarin, R., Shrivastava, S. et al.: Cosmesis, late sequelae and local control after breast-conserving therapy: Influence of type of tumour bed boost and adjuvant chemotherapy. Clinical Oncology 19, 596–603 (2007)
Al-Ghazal, S. K., Fallowfield, L., Blamey, R. W.: Does cosmetic outcome from treatment of primary breast cancer influence psychosocial morbidity? European Journal of Surgical Oncology 25, 571–573 (1999)
Garbey, M., Thanoon, D., Salmon, R., et al.: Multiscale modeling and computational surgery: application to breast conservative therapy. JSSCM 5, 81–89 (2011)
Fung, Y. C.: Biomechanics: Motion, Flow, Stress and Growth, Springer Verlag, New York (1990)
Murray, J. D.: Mathematical Biology: II Spatial Modles and Biomedical Applications. 3rd edn. Springer, New York 2003.
Garbey, M., Berceli, S., Tran Son Tay, R., et al.: A Dynamical System that Describes Vascular Adaptation, manuscript submitted.
Thanoon, D.: Computational framework for local breast cancer treatment, [Ph. D. Thesis] Department of Computer Science, University of Houston (2011)
Dormand, E. L., Banwell, P. E., EE Goodacre, T.: Radiotherapy and Wound Healing. International Wound Journal. 2, (2005)
Tranquillo, R. T., Murray, J. D.: Continuum model of fibroblast-driven wound contraction: inflammation-mediation. Journal of Theoretical Biology 158, 135–172 (1992)
Olsen, L., Sherratt, J. A., Maini, P. K.: A mechanochemical model for adult dermal wound contraction and the permanence of the contracted tissue displacement profile. J. Theor. Biol. 177, 113–128 (1995)
Mc Dougall, S., Dallon, J., Serratt, J., et al.: Fibroblast migration and collagen deposition during dermal wound healing: mathematical modelling and clinical implications. Phil, Trans. R. Soc. A 364, 1385–1405 (2006)
Javierre, E., Vermolen, F. J., Vuik, C., et al.: A mathematical analysis of physiological and morphological aspects of wound closure. J. Math. Biol. 59, 605–630 (2009)
Sherrat, J. A., Dallon, J. C.: Theoretical model of wound healing: past successes and future challenges. C. R. Biologies 325, 557–564 (2002)
Javierre, E., Moreo, P., Doblar’e, M., et al.: Numerical model of mechano-chemical theory for wound contraction analysis. International Journal of Solids and Structures 46, 3597–3606 (2009)
Osher, S., Fedkiw, R.: Level Set Methods and Dynamic Implicit Surfaces. Applied Mathematics Science series 153, Springer Verlag (2003)
Ramière, I., Angot, P., Belliard, M.: A general fictitious domain method with immersed jumps and multilevel nested structured meshes. Journal of Computational Physics 225, 1347–1387 (2007)
Omens, J. H., Miller, T. R., Covell, J.W.: Relationship between passive tissue strain and collagen uncoiling during healing of infarcted myocardium. Cardiovascular Research 33, 351–358 (1997)
Hwang, M., Berceli, S. A., Garbey, M., et al.: The dynamics of vein graft remodeling induced by hemodynamic forces - a mathematical model. Biomechanics and Modeling in Mechanobiology. 11, 411–423 (2012)
Hwang, M., Garbey, M., Berceli, S. A., et al.: Ruled-based simulation of multi-cellular biological systems - a review of modeling techniques. Cellular and Molecular Bioengineering 2, 285–295 (2009)
Hwang, M., Berceli, S. A., Tran-Son-Tay, R.: Modeling and role of leukocytes in inflammation, In: Garbey, M., Bass, B. L., Collet, C., et al., eds. Computational Surgery and Dual Training. Springer, New York (2010)
Hwang, M., Garbey, M., Berceli, S. A., et al.: A First Rule Base Simulation of Vein Graft Remodeling In: Garbey, B., Bass, S., Berceli, P., et al., eds. Computational Surgery and Dual Training. New York: Springer Verlag (2012)
Hwang, M., Garbey, M., Berceli, S. A., et al.: Rule-Based Model of Vein Graft Remodeling, mansucript submitted.
Wang, Y., Xu, M., Wang, Z., et al.: How to cluster gene expression dynamics in response to environmental signals. Briefings in Bioinformatics 13, 162–174 (2011)
Deutsch, A., Dormann, S.: Cellular Automaton Modeling of Biological Pattern Formation. Birkhuser, Boston (2005)
Thorne, B. C., Bailey, A. M., Peirce, S. M.: Combining experiments with multi-cell agent-based modeling to study biological tissue patterning. Brief Bioinform 8, 245–257 (2007)
Gilles, M.: Breast conservative surgery pilot study: data acquisition design and image processing. Master Thesis, Department of Computer Science, University of Houston, (2012)
Azar, F. S., Metaxas, D. N., Schnall, M. D.: A finite element model of the breast for predicting mechanical deformations during interventional procedures. Proc. Int. Soc. Magn. Reson. Med. 7, 1084–1085 (1999)
Azar, F. S., Metaxas, D. N., Schnall, M. D.: Methods for modeling and predicting mechanical deformations of the breast under external perturbations. Medical Image Analysis 6, 1–27 (2002)
Chung, J. H.: Modelling mammographic mechanics, Auckland Bioengineering Institute, The University of Auckland (2008)
Ozan, C.: Mechanical modeling of brain and breast tissue, [Ph. D. Thesis] Georgia Institute of Technology (2008)
Tanner, C.: A method for the comparison of biomechanical breast models, Mathmatical Methods in Biomedical Image Analysis, 11–18 (2001)
Tanner, C.: The comparison of biomechanical breast models: initial results, ANSYS Proceedings (2002)
Tanner, C., Schnabel, J. A., Derek, L. G. H., et al.: Factors influencing the accuracy of biomechanical breast models, American Association of Physicists in Medicine 33, 1758–1769 (2006)
Taylor, et al.: Factors influencing cosmetic results after conservation therapy for breast cancer. Int. J. Radiation Oncology Biol. Phys. 31, 753–764 (1995)
Lankton, S., Tannenbaum, A.: Localizing region-based active contours. Image Processing, IEEE Transactions on, 17, 1–11 (2008)
Yang, S. C., Wang, C. M., Hsu, H. H., et al.: Contrast enhancement and tissues classification of breast MRI using Kalman filter-based linear mixing method. Comput Med Imaging Graph. 33, 187–196 (2009)
Rajagopal, V.: Modelling Breast Tissue Mechanics Under Gravity Loading, Auckland Bioengineering Institute, The University of Auckland (2007)
Rose, S. C., Nelson, T. R., Deutsch, R. J.: Display of — dimensional ultrasonographic images for interventional procedures: volume-rendered versusmultiplanar display. Ultrasound Med. 23, 1465–1473 (2004)
Garbey, M., Tromeur-Dervout, D.: A parallel adaptive coupling algorithm for systems of differential equations. J. Comput. Phys. 161, 401–427 (2000)
Roller, S., Klimach, H.: A multi-scale coupling scheme on heterogeneous supercomputers. In: Proceedings of The Seventh International Conference on Engineering Computational Technology (ECT2010), Valencia, Spain (2010)
Collins, E. D., Moore, C. P., Clay, K. F., et al.: Can women with early-stage breast cancer make an informed decision for mastectomy? J. Clin. Oncol. 27, 519–525 (2009)
Lacovara, J. E., Arzouman, J., Kim, C. J., et al.: Are patients with breast cancer satised with their decision making? a comparison over time. Clin. J. Oncol. Nurs. 15, 320–323 (2011)
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Garbey, M., Bass, B.L. & Berceli, S. Multiscale mechanobiology modeling for surgery assessment. Acta Mech Sin 28, 1186–1202 (2012). https://doi.org/10.1007/s10409-012-0133-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10409-012-0133-4