Abstract
Purpose
Radio-frequency (RF) signals from the most dominant scatterer in a dermis, i.e., collagen fibers, are collected as backscattered signals. We aim to confirm the frequency dependence of the spatial distribution of features in ultrasound images, as well as the attenuation coefficient (AC) and backscatter coefficient (BSC) of skin tissue without [LE (−)] and with lymphedema [LE (+)].
Methods
Measurement samples (n = 13) were excised from human skin tissue with LE (−) and middle severity LE (+). A laboratory-made scanner and single-element concave transducers (range 9–47 MHz) were used to measure RF data. A localized AC was computed from the normalized power spectrum using the linear least squares technique. The reflector method and compensation technique of the attenuation of tissue were applied to calculate the BSC. In addition, effective scatterer diameter (ESD), effective acoustic concentration (EAC), and integrated BSC (IBS) were calculated from the BSC as the benchmark to differentiate LE (−) and LE (+) tissues.
Results
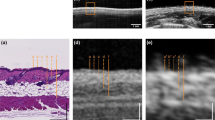
High-frequency ultrasound displayed different echogenicity and texture compared between LE (−) and LE (+) in all transducers. The AC for LE (−) (0.22 dB/mm/MHz) and LE (+) (0.29 dB/mm/MHz) was comparable. BSC in LE (−) and LE (+) increased linearly with each transducer. The difference of intercept of the BSC between LE (−) and LE (+) indicated that both EAC and IBS of LE (+) were higher than that of LE (−). In contrast, ESD correlated with the slope of the BSC demonstrated the same tendency for both LE (−) and LE (+). These tendencies appeared for each transducer independent of the frequency bandwidth.
Conclusion
Frequency independence of AC and BSC in LE (−) and LE (+) was confirmed. Several 9- to 19-MHz ultrasound beams are sufficient for BSC analysis to discriminate LE (−) and LE (+) in terms of the penetration depth of the ultrasound.







Similar content being viewed by others
References
Akita S, Mitsukawa N, Kazama T, Kuriyama M, Kubota Y, Omori N, et al. Comparison of lymphoscintigraphy and indocyanine green lymphography for the diagnosis of extremity lymphoedema. J Plast Reconstr Aesthetic Surg. Elsevier Ltd. 2013;66:792–8.
Akita S, Mitsukawa N, Rikihisa N, Kubota Y, Omori N, Mitsuhashi A, et al. Early diagnosis and risk factors for lymphedema following lymph node dissection for gynecologic cancer. Plast Reconstr Surg. United States. 2013;131:283–90.
Kleinerman R, Whang TB, Bard RL, Marmur ES. Ultrasound in dermatology: principles and applications. J Am Acad Dermatol. 2012;67:478–87.
Kumagai K, Koike H, Nagaoka R, Sakai S, Kobayashi K, Saijo Y. High-resolution ultrasound imaging of human skin in vivo by using three-dimensional ultrasound microscopy. Ultrasound Med Biol. 2012;38:1833–8.
Suehiro K, Morikage N, Yamashita O, Harada T, Samura M, Takeuchi Y, et al. Correlation between the severity of subcutaneous echo-free space and the amount of extracellular fluid determined by bioelectrical impedance analysis of leg edema. Lymphat Res Biol. 2017;15:172–6.
Guittet C, Ossant F, Vaillant L, Berson M. In vivo high-frequency ultrasonic characterization of human dermis. IEEE Trans Biomed Eng. 1999;46:740–6.
Fournier C, Bridal SL, Berger G, Laugier P. Reproducibility of skin characterization with backscattered spectra (12–25 MHz) in healthy subjects. Ultrasound Med Biol. 2001;27:603–10.
Bridal SL, Fournier C, Coron A, Leguerney I, Laugier P. Ultrasonic backscatter and attenuation (11–27 MHz) variation with collagen fiber distribution in ex vivo human dermis. Ultrason Imaging. 2006;28:23–40.
Moran CM, Bush NL, Bamber JC. Ultrasonic propagation properties of excised human skin. Ultrasound Med Biol. 1995;21:1177–90.
Raju BI, Srinivasan MA. High-frequency ultrasonic attenuation and backscatter coefficients of in vivo normal human dermis and subcutaneous fat. Ultrasound Med Biol. 2001;27:1543–56.
Raju BI, Srinivasan MA. Statistics of envelope of high-frequency ultrasonic backscatter from human skin in vivo. IEEE Trans Ultrason Ferroelectr Freq Control. 2002;49:871–82.
Raju BI, Swindells KJ, Gonzalez S, Srinivasan MA. Quantitative ultrasonic methods for characterization of skin lesions in vivo. Ultrasound Med Biol. 2003;29:825–38.
Lin Y-H, Huang C-C, Wang S-H. In vivo assessment of inflammatory skin using high frequency ultrasound image and quantitative parameters. In: 2010 IEEE international ultrasonics symposium. San Diego: IEEE; 2010. p. 2311–4.
Omura M, Yoshida K, Akita S, Yamaguchi T. Verification of echo amplitude envelope analysis method in skin tissues for quantitative follow-up of healing ulcers. Jpn J Appl Phys. 2018;57:07LF15-1–11.
Chen X, Phillips D, Schwarz KQ, Mottley JG, Parker KJ. The measurement of backscatter coefficient from a broadband pulse-echo system: a new formulation. IEEE Trans Ultrason Ferroelectr Freq Control. 1997;44:515–25.
Lavarello RJ, Ghoshal G, Oelze ML. On the estimation of backscatter coefficients using single-element focused transducers. J Acoust Soc Am. 2011;129:2903–11.
Oelze ML, O’Brien WD. Frequency-dependent attenuation-compensation functions for ultrasonic signals backscattered from random media. J Acoust Soc Am. 2002;111:2308.
Franceschini E, Guillermin R. Experimental assessment of four ultrasound scattering models for characterizing concentrated tissue-mimicking phantoms. J Acoust Soc Am. 2012;132:3735–47.
Oelze ML, Zachary JF, O’Brien WD. Characterization of tissue microstructure using ultrasonic backscatter: theory and technique for optimization using a Gaussian form factor. J Acoust Soc Am. 2002;112:1202–11.
Suehiro K, Morikage N, Murakami M, Yamashita O, Ueda K, Samura M, et al. Subcutaneous tissue ultrasonography in legs with dependent edema and secondary lymphedema. Ann Vasc Dis. 2014;7:21–7.
Tashiro K, Feng J, Wu SH, Mashiko T, Kanayama K, Narushima M, et al. Pathological changes of adipose tissue in secondary lymphoedema. Br J Dermatol. 2017;177:158–67.
Meijer R, Douven LFA, Oomens CWJ. Characterisation of anisotropic and non-linear behaviour of human skin in vivo. Comput Methods Biomech Biomed Eng. 1999;2:13–27.
Yamaji Y, Akita S, Akita H, Miura N, Gomi M, Manabe I, et al. Development of a mouse model for the visual and quantitative assessment of lymphatic trafficking and function by in vivo imaging. Sci Rep. 2018;8:5921.
Coila AL, Lavarello R. Regularized spectral log difference technique for ultrasonic attenuation imaging. IEEE Trans Ultrason Ferroelectr Freq Control. 2018;65:378–89.
Vajihi Z, Rosado-Mendez IM, Hall TJ, Rivaz H. Low variance estimation of backscatter quantitative ultrasound parameters using dynamic programming. IEEE Trans Ultrason Ferroelectr Freq Control IEEE. 2018;65:2042–53.
Acknowledgements
This work was partly supported by the JSPS Core-to-Core Program (A. Advanced Research Networks) and KAKENHI Grant Numbers 17H05280 and 17J07762. We also acknowledge financial support from the Institute for Global Prominent Research and the Frontier Science Program of Graduate School of Science and Engineering at Chiba University. We would like to express our gratitude to Professor Ichiro Manabe and Dr. Noriko Yamanaka with respect to histopathological findings.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that there are no conflicts of interest.
Human rights statements and informed consent
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1964 and later versions. Informed consent was obtained from all patients for being included in the study. Additional informed consent was obtained from all patients for which identifying information is included in this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Omura, M., Yoshida, K., Akita, S. et al. Frequency dependence of attenuation and backscatter coefficient of ex vivo human lymphedema dermis. J Med Ultrasonics 47, 25–34 (2020). https://doi.org/10.1007/s10396-019-00973-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10396-019-00973-z