Abstract
Purpose
To clarify whether intrapartum transperineal ultrasound (ITU) can be used to evaluate uterine contraction intensity, and whether the intensity is associated with the duration of the second stage.
Methods
A prospective observational study was performed involving 86 women with a normal singleton term fetus and more than three contractions every 10 min. ITU was performed for contractile and non-contractile periods of labor at the beginning of the second stage, and one representative “angle of progression (AoP)” image was selected for each period. The Mann–Whitney U test was used to compare ∆AoP, the difference between the two angles, depending on the duration of the second stage. Receiver operating characteristic curves were used to evaluate the probability of duration of the second stage ≤50 min in nulliparous women.
Results
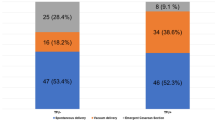
Among nulliparous women, ΔAoP differed significantly according to the duration of the second stage (52.5° ± 5.0° for ≤50 min vs. 30.9° ± 2.1° for >50 min; P < 0.001). Receiver operating characteristic curve analysis showed that approximately 85% of nulliparous women with ΔAoP greater than 40° delivered within 50 min.
Conclusion
These findings could be utilized in the evaluation of uterine contraction intensity, and ∆AoP measurement could be used to predict the duration of the second stage of labor in nulliparous women.




Similar content being viewed by others
References
Dietz HP, Lanzarone V. Measuring engagement of the fetal head: validity and reproducibility of a new ultrasound technique. Ultrasound Obstet Gynecol. 2005;25:165–8.
American College of Obstetrics and Gynecology Committee on Practice Bulletins-Obstetrics. ACOG Practice Bulletin Number 49, December 2003: Dystocia and augmentation of labor. Obstet Gynecol 2003;102:1445–54.
Henrich W, Dudenhausen J, Fuchs I, et al. Intrapartum translabial ultrasound (ITU): sonographic landmarks and correlation with successful vacuum extraction. Ultrasound Obstet Gynecol. 2006;28:753–60.
Barbera AF, Pombar X, Perugino G, et al. A new method to assess fetal head descent in labor with transperineal ultrasound. Ultrasound Obstet Gynecol. 2009;33:313–9.
Ghi T, Farina A, Pedrazzi A, et al. Diagnosis of station and rotation of fetal head in the second stage of labor with intrapartum translabial ultrasound. Ultrasound Obstet Gynecol. 2009;33:331–6.
Eggebo TM, Heien C, Okland I, et al. Ultrasound assessment of fetal head-perineum distance before induction of labor. Ultrasound Obstet Gynecol. 2008;32:199–204.
Youssef A, Bellussi F, Montaguti E, et al. Agreement between two- and three-dimensional transperineal ultrasound methods for assessment of fetal head-symphysis distance in active labor. Ultrasound Obstet Gynecol. 2014;43:183–8.
Morina FS, Terra R, Carrillo MP, et al. What is the most reliable ultrasound parameter for assessment of fetal head descent? Ultrasound Obstet Gynecol. 2010;36:493–9.
Kalache KD, Duckelmann AM, Michaelis SAM, et al. Transperineal ultrasound imaging in prolonged second stage of labor with occipitoanterior presenting fetuses: how well does the ‘angle of progression’ predict the mode of delivery? Ultrasound Obstet Gynecol. 2009;33:326–30.
Tutschek B, Braun T, Chantraine F, et al. A study of labour using intrapartum translabial ultrasound, assessing head station, direction, and of descent. BJOG. 2011;118:62–9.
Roemer VM, Harms K, Buess H, et al. Response of fetal acid-balance to duration second stage of labour. Int J Gynaecol Obstet. 1976;14:455–71.
Ghi T, Maroni E, Youssef A, et al. Sonographic pattern of fetal head descent: relationship with duration of active second stage of labor and occiput position at delivery. Ultrasound Obstet Gynecol. 2014;44:82–9.
Wilmink FA, Wilms FF, Heydanus R, et al. Fetal complications after placement of an intrauterine pressure catheter: a report of two cases and review of the literature. J Matern Fetal Neonatal Med. 2008;21:880–3.
Madanes AE, David D, Cetrulo C. Major complications associated with intrauterine pressure monitoring. Obstet Gynecol. 1982;59:389–91.
Lind BK. Complications caused by extramembranous placement of intrauterine pressure ctheters. Am J Obstet Gynecol. 1999;180:1034–5.
Trudinger BJ, Pryse-Davies J. Fetal hazards of the intrauterine pressure catheter: five case reports. BJOG. 1978;85:567–72.
Nuttall ID. Perforation of a placental fetal vessel by an intrauterine pressure catheter. BJOG. 1978;85:573–4.
Soper DE, Mayhall CG, Dalton HP. Risk factors for intraamniotic infection: a prospective epidemiologic study. Am J Obstet Gynecol. 1989;161:562–8.
Harbison L, Bell L. Anaphylactoid syndrome after intrauterine pressure catheter placement. Obstet Gynecol. 2010;115:407–8.
Bakker JJH, Verhoeven CJM, Janssen PF, et al. Outcomes after internal versus external tocodynamometry for monitoring labor. N Engl J Med. 2010;362:306–13.
Chua S, Kurup A, Arulkumaran S, et al. Augmentation of labor: does internal tocography result in better obstetric outcome than external tocography? Obstet Gynecol. 1990;76:164–7.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical statements
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation and with the Helsinki Declaration of 1964 and later versions.
Conflict of interest
Miyuki Muramoto, Kiyotake Ichizuka, Junichi Hasegawa, Masamitsu Nakamura, Satoshi Dohi, Hiroshi Saito, and Masaaki Nagatsuka declare that they have no conflict of interest.
About this article
Cite this article
Muramoto, M., Ichizuka, K., Hasegawa, J. et al. Intrapartum transperineal ultrasound for evaluating uterine contraction intensity in the second stage of labor. J Med Ultrasonics 44, 117–122 (2017). https://doi.org/10.1007/s10396-016-0752-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10396-016-0752-7