Abstract
Purpose
To investigate whether transperineal ultrasound examination just after full cervical dilatation is determined can predict the mode of delivery.
Methods
This was a prospective observational study of pregnant women. After full cervical dilatation was determined by vaginal examination during labor, transperineal ultrasound was immediately performed, and the head direction (HD), progression distance (PD), and angle of progression (AoP) were measured. The cases were divided into two groups: spontaneous vaginal delivery and operative delivery due to failure of progression. Differences between the groups were statistically analyzed using Student’s t test and Fisher’s exact test.
Results
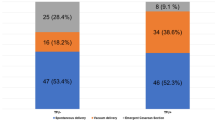
Of the 50 women, 42 had spontaneous vaginal deliveries and 8 had vacuum extractions. The spontaneous delivery group had significantly higher HD, PD, and AoP values than the vacuum extraction group. The areas under the receiver-operating characteristic curves for the prediction of spontaneous vaginal delivery were 0.850 for HD, 0.827 for PD, and 0.783 for AoP. The optimum cut-off points and positive predictive values were 83° and 92.9 % for HD, 56 mm and 94.9 % for PD, and 146° and 94.3 % for AoP, respectively.
Conclusion
Transperineal ultrasound examination just after full cervical dilatation was determined was useful in predicting spontaneous vaginal delivery.



Similar content being viewed by others
References
Sherer DM, Miodovnik M, Bradley KS, et al. Intrapartum fetal head position I: comparison between transvaginal digital examination and transabdominal ultrasound assessment during the active stage of labor. Ultrasound Obstet Gynecol. 2002;19:258–63.
Sherer DM, Miodovnik M, Bradley KS, et al. Intrapartum fetal head position II: comparison between transvaginal digital examination and transabdominal ultrasound assessment during the active stage of labor. Ultrasound Obstet Gynecol. 2002;19:264–8.
Dupuis O, Ruimark S, Corinne D, et al. Fetal head position during the second stage of labor: comparison of digital vaginal examination and transabdominal ultrasonographic examination. Eur J Obstet Gynecol Reprod Biol. 2005;123:193–7.
Dupuis O, Silveira R, Zentner A, et al. Birth simulator: reliability of transvaginal assessment of fetal head station as defined by the American College of Obstetricians and Gynecologists classification. Am J Obstet Gynecol. 2005;192:868–74.
Buchmann E, Libhaber E. Interobserver agreement in intrapartum estimation of fetal head station. Int J Gynecol Obstet. 2008;101:285–9.
Dietz HP, Lanzarone V. Measuring engagement of the fetal head: validity and reproducibility of a new ultrasound technique. Ultrasound Obstet Gynecol. 2005;25:165–8.
Barbera AF, Pombar X, Peruginoj G, et al. A new method to assess fetal head descent in labor with transperineal ultrasound. Ultrasound Obstet Gynecol. 2009;33:313–9.
Ghi T, Farina A, Pedrazzi A, et al. Diagnosis of station and rotation of the fetal head in the second stage of labor with intrapartum translabial ultrasound. Ultrasound Obstet Gynecol. 2009;33:331–6.
Dückelmann AM, Bamberg C, Michaelis SA, et al. Measurement of fetal head descent using the “angle of progression” on transperineal ultrasound imaging is reliable regardless of fetal head station or ultrasound expertise. Ultrasound Obstet Gynecol. 2010;35:216–22.
Ghi T, Contro E, Farina A, et al. Three-dimensional ultrasound in monitoring progression of labor: a reproducibility study. Ultrasound Obstet Gynecol. 2010;36:500–6.
Molina FS, Terra R, Carrillo MP, et al. What is the most reliable ultrasound parameter for assessment of fetal head descent? Ultrasound Obstet Gynecol. 2010;36:493–9.
Torkildsen EA, Salvesen KÅ, Eggeboø TM. Agreement between two- and three-dimensional transperineal ultrasound methods in assessing fetal head descent in the first stage of labor. Ultrasound Obstet Gynecol. 2012;39:310–5.
Kalache KD, Dückelmann AM, Michaelis SA, et al. Transperineal ultrasound imaging in prolonged second stage of labor with occipitoanterior presenting fetuses: how well does the “angle of progression” predict the mode of delivery? Ultrasound Obstet Gynecol. 2009;33:326–30.
Torkildsen EA, Salvesen KÅ, Eggebø TM. Prediction of delivery mode with transperineal ultrasound in women with prolonged first stage of labor. Ultrasound Obstet Gynecol. 2011;37:702–8.
Eggebø TM, Hassan WA, Salvesen KA, et al. Sonographic prediction of vaginal delivery in prolonged labor: a two-center study. Ultrasound Obstet Gynecol. 2014;43:195–201.
American College of Obstetrics and Gynecology. Dystocia and augmentation of labor. ACOG practice bulletin no. 49. Obstet Gynecol. 2003;102:1445–54.
American College of Obstetrics and Gynecology. Operative vaginal delivery. Clinical management guidelines for obstetrician-gynecologists. Int J Gynaecol Obstet. 2001;74:69–76.
Japan Society of Obstetrics and Gynecology. Guideline for obstetrical practice in Japan 2014. Tokyo: Japan Society of Obstetrics and Gynecology; 2014. p. 225–31.
Rane SM, Guirgis RR, Higgins B, et al. The value of ultrasound in the prediction of successful induction of labor. Ultrasound Obstet Gynecol. 2004;24:538–49.
Henrich W, Dudenhausen J, Fuchs I, et al. Intrapartum translabial ultrasound (ITU): sonographic landmarks and correlation with successful vacuum extraction. Ultrasound Obstet Gynecol. 2006;28:753–60.
Gilboa Y, Kivilevitch Z, Spira M, et al. Head progression distance in prolonged second stage of labor: relationship with mode of delivery and fetal head station. Ultrasound Obstet Gynecol. 2013;41:436–41.
Ghi T, Youssef A, Maroni E, et al. Intrapartum transperineal ultrasound assessment of fetal head progression in active second stage of labor and mode of delivery. Ultrasound Obstet Gynecol. 2013;41:430–5.
Hassan SJ, Sundby J, Husseini A, et al. The paradox of vaginal examination practice during normal childbirth: palestinian women’s feelings, opinions, knowledge and experiences. Reprod Health. 2012;9:16.
Westover T, Knuppel RA. Modern management of clinical chorioamnionitis. Infect Dis Obstet Gynecol. 1995;3:123–32.
Barbera AF, Imani F, Becker T, et al. Anatomic relationship between the pubic symphysis and ischial spines and its clinical significance in the assessment of fetal head engagement and station during labor. Ultrasound Obstet Gynecol. 2009;33:320–5.
Bamberg C, Scheuermann S, Slowinski T, et al. Relationship between fetal head station established using an open magnetic resonance imaging scanner and the angle of progression determined by transperineal ultrasound. Ultrasound Obstet Gynecol. 2011;37:712–6.
Eggebø TM, Økland I, Heien C, et al. Can ultrasound measurements replace digitally assessed elements of the Bishop score? Acta Obstet Gynecol Scand. 2009;88:325–31.
Hassan WA, Eggebø T, Ferguson M, et al. The sonopartogram: a novel method for recording progress of labor by ultrasound. Ultrasound Obstet Gynecol. 2014;43:189–94.
Acknowledgments
We wish to thank Kaoru Goto, Kakunodate General Hospital; Hiromitsu Tsubaki, Ogachi Chuo Hospital; and the obstetric doctors and midwives for their assistance. In addition, we would like to thank Kouichi Kobayashi and Ken Sakamaki, Japan Community Health Care Organization, Tokyo Yamate Medical Center.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Saeko Kameyama, Akira Sato, Hiroshi Miura, Jin Kumagai, Naoki Sato, Dai Shimizu, Kenichi Makino, and Yukihiro Terada declare that they have no conflict of interest.
Human rights statements and informed consent
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1964 and later versions. Informed consent was obtained from all patients for being included in the study.
About this article
Cite this article
Kameyama, S., Sato, A., Miura, H. et al. Prediction of spontaneous vaginal delivery by transperineal ultrasound performed just after full cervical dilatation is determined. J Med Ultrasonics 43, 243–248 (2016). https://doi.org/10.1007/s10396-015-0681-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10396-015-0681-x