Abstract
Aim
This article takes a closer look at the decision-making process to recommend a new vaccine in the light of the Finnish experience.
Subject and methods
The criteria for evidence-based knowledge are examined in order to consider how public health decision-making in the area of immunisation evolves over time and from one context to the other on the basis of three of the more recent childhood vaccines (Haemophilus influenzae type b (Hib), seven-valent pneumococcal conjugate (PCV-7), and Human Papilloma Virus (HPV)).
Results
In the case of Hib vaccine, epidemiological research concerning both direct and indirect population protection was the driving force for implementation. By contrast, PCV-7 universal vaccination was not implemented on the basis of unfavourable cost-effectiveness evaluation. However, as this evaluation took place very early on, the cost-effectiveness analysis did not consider any indirect herd effects. Regarding the HPV vaccine, it is at present considered that cervical cancer will be better prevented by enhancing the already successful PAP smear screening programme.
Conclusion
Surveillance and research are valuable tools for modern vaccine programme design. Market forces and advocacy groups strongly drive the development and implementation of new vaccines, meaning that impartial and evidence-based decision-making is essential to vaccine introduction into national programmes. At the same time, economic analyses are occupying an increasingly important place in this decision-making. Vaccine costs are not necessarily compared to government expenditure on illness and disease. From a moral point of view, it should not be forgotten that children ought to have the right to best available health.
Similar content being viewed by others
Introduction
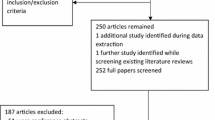
National vaccination programmes in European Union member states vary considerably regarding antigenic composition and schedule as Lopalco (Lopalco, 2008) and Schmitt (Schmitt et al. 2003) have already pointed out. There are several explanations for this. Historical reasons combine with reasons related to the country’s specific health-care delivery system and funding mechanisms; these, in turn, are influenced by current common knowledge of vaccinology arising from both national and international evidence and scientific reports. There are major variations on how such knowledge and evidence are taken into consideration and used in the context of programme design and decision-making. In Finland, national vaccination programme-related research and surveillance are co-ordinated within the national public health system and form a firm platform on which vaccine programme-related decisions are made (Fig. 1).
Ideally, those in charge of developing a national vaccination programme need to think of the right questions to ask and communicate them to those in charge of and financing research and surveillance.
It is essential to choose the right methodology when wishing to come up with programmatically useful answers. Well set up and sufficiently sensitive surveillance systems with sufficiently specific case definitions along with targeted epidemiological studies shed light on whether the disease can be considered a public health problem. Vaccine immunology studies guide in finding optimal doses and schedules provided serological correlates of protection exist; they also alert to possible interferences if several vaccines are combined or given simultaneously. They also give an understanding on the reactogenicity of the product. Vaccine efficacy trials are usually required for regulatory and licensure purposes. Vaccine effectiveness studies thereafter will provide answers as to whether the disease actually is vaccine preventable in the intended target groups. Vaccine safety is thoroughly addressed in clinical trials for licensure. However, rare adverse events are often identified only after a large number of doses has been administered, i.e., subsequent to widespread use of the vaccine. Thus, reports on adverse events and record linkage studies impart additional important safety knowledge. The need to know well in advance the impact of different vaccination scenarios has promoted the development and use of advanced tools of mathematical modelling. Simulation models can provide insights in silica as to whether wide-scale vaccination could have adverse and/or positive indirect effects on the population level in the long run. An increasingly important line of modelling is provided by health economics when considering whether vaccination could be cost-effective in a given setting.
The key questions a vaccine programme designer needs to ask are:
-
Is the disease a public health problem?
-
Is the disease vaccine preventable?
-
How does the vaccine work?
-
Is the vaccine safe?
-
Could wide-scale vaccinations have adverse or positive indirect effects on the population level?
-
Would vaccination be cost-effective?
Research driving vaccine implementation–the example of the Hib vaccine
In Finland, vaccine research has been an essential part of programme design for decades. The development of a Haemophilus influenzae type b (Hib) conjugate vaccine serves as a good demonstration case. Studies and clinical trials were carried out in Finland as early as in the 1980s–1990s (Eskola et al. 1992a, b). The baseline surveillance study among children under 5 years of age identified the incidence of Hib disease (52/100,000) as well as its clinical spectrum. The majority of cases presented as meningitis and epiglottitis (Takala et al. 1989). The baseline study was utilised to fine-tune the laboratory infrastructure required to initiate a nationwide phase III individual randomised controlled trial, which eventually demonstrated not only the high direct clinical efficacy of the diphtheria toxoid conjugated Hib vaccine (Eskola et al. 1990), but also the indirect protective impact of the vaccine, a ground-breaking observation (Eskola et al. 1996) (Fig. 2). The latter property of the vaccine was due to the reduction of the oropharyngeal carriage of the bacterium (Takala et al. 1989) and was soon evident given the decrease in disease incidence among those not vaccinated. In conjunction with the efficacy trial, several phase II immunogenicity studies were conducted in order to better understand the immunological properties and functional mechanisms of the various Hib vaccines.
In 1993, after the completion of the series of efficacy studies during which most Finnish infants had received Hib vaccine according to age, the Hib vaccine was introduced into the national immunisation programme, i.e., given to all children in Finland from 3 months of age onwards. This decision was made in the absence of any formal cost-efficacy calculations and without major disputes among stakeholders.
A clinical trial did not secure implementation into the programme–the example of pneumococcal conjugate vaccine
The enhanced surveillance system of invasive childhood diseases established for carrying out the Hib vaccine studies provided a firm network and basis of national knowledge on other causative bacterial agents among children (Saarinen et al. 1995). The gate keeping and development of the notification system were transferred from the Medical Board to the National Public Health Institute (Kansanterveyslaitos, KTL), which was charged with establishing a computer-based national communicable disease registry. For pneumococcus, special surveillance studies aimed at understanding pneumonia (Jokinen et al. 1993) and acute otitis media (Kilpi et al. 2001) complemented the data arising from the national surveillance system. It became evident that with the relatively low incidence rates of invasive pneumococcal disease among children (Eskola et al. 1992a, b), a phase III clinical trial with the endpoint of invasive pneumococcal disease would be an immense nationwide undertaking. Instead, the researchers agreed on a smaller pre-licensure trial with originally three new pneumococcal conjugate vaccines to be carried out to address a clinically less severe endpoint: otitis media. In Finland otitis media actually caused a much greater public health disease burden. This trial established the mean serotype-specific efficacy of 57% of the two candidate vaccines licensed (Eskola et al. 2001; Kilpi et al. 2003) and also provided important information on the disease burden itself. After the trial, however, seven-valent pneumococcal conjugate vaccine (PCV-7) did not make it to the national programme. Why not? How did this happen? Most professionals and lay persons alike were perplexed. What had changed between the 1990s and 2000?
From expert advice to policy formation-What changed between the 1990s and 2000?
At the turn of the present century several new paediatric vaccines became available on the market. Of these, both the rotavirus vaccine and pneumococcal conjugates were studied in Finland as part of the manufacturers phase III licensure trials (Eskola et al. 2001; Kilpi et al. 2005; Joensuu et al. 1997). It was no longer self-evident, however, that all these efficacious vaccines could be adopted by the national programme without going through a process of formal consideration, completely detached from the investigators’ own interests. Also, the higher cost of the vaccines called for a thorough economic analysis. In face of the increasing public and professional demand that health policies and guidelines of all kinds be based as much as possible on scientifically sound evidence, this without doubt also applied to the introduction of any new vaccine.
In 2000, a national advisory committee for vaccination (Kansallinen rokotusasiantuntijaryhmä, KRAR) was formed that commissioned vaccine-specific expert groups to help evaluate the scientific evidence on the basis of which the new vaccine was to be introduced (Fig. 3) (Rapola 2007). To standardise these expert evaluations, KRAR agreed on a “four-step” approach. In order to be considered for financing from the national health budget, the following four criteria had to be met:
-
(1)
Public health benefit, i.e., there should be a considerable disease burden, and vaccination should be expected to alleviate this burden;
-
(2)
Vaccine safety on the individual level, i.e., the risks of vaccination to an individual should be minimal and outweighed by the expected health benefits;
-
(3)
Vaccine safety on the population level, i.e., wide-scale vaccination should not have major adverse effects on the population in short or long term;
-
(4)
Cost-effectiveness, i.e., the intervention should be sufficiently cost-effective from the societal point of view as the universal vaccination programme is completely shouldered by the Finnish government.
Despite the licensure trials having been carried out in the country, PCV-7 was scrutinised according to the “four-step” approach. For the evaluation task, the vaccine expert group accessed local disease burden data via the national communicable disease registry and combined it with trial-related data on both burden and efficacy (Table 1). Based on the 2000 costing figures, in an annual birth cohort of 55,000 infants, the cost effectiveness analysis indicated when considering the direct effects alone, investing 12.0 million € would save annually 6.3 million € in medical and 2.0 million € in productivity and other costs. Therefore, investing 1 million € in a vaccination programme would return 0.53 million € in medical costs and 0.70 million € in societal costs. In the base case, vaccination would cost society 134,986 € per life year saved (LYS). To achieve cost savings from a health-care provider (societal) perspective, the price of PCV-7 should be 50% (70%) of the price used in the base case. In other words, PCV-7 did not avert enough cases and deaths in comparison to the predicted costs when given as a four-dose schedule, assuming similar vaccine efficacy point prevalence values as in the US trials for invasive disease and otitis complications and in the Finnish trials for acute otitis media-related events (Salo et al. 2005).
The cost-effectiveness analysis at that time did not take into consideration the possibility of the serotype replacement phenomenon or the indirect herd protection of PCV-7 in averting disease in the non-vaccinated age groups (Anonymous, 2005) as very little data beyond the proof of reduction of upper respiratory carriage of pneumococcus (Dagan et al. 1996) was then available. As a result of an early, and in retrospect a very conservative evaluation, PCV-7 was not introduced into the Finnish immunisation programme on the universal level; it was recommended to be given to risk group children only (Nohynek et al. 2005). A new evaluation including potential herd effects and replacement phenomenon, and calculating impact in quality-adjusted life years (QALY) in addition to LYS, is nearing completion, after which the earlier negative decision will soon be revisited.
What will happen in the future–the example of Human Papilloma Virus-vaccine in preventing cervical cancer
Similarly to the PCV-7 evaluation, several other vaccine antigens have been considered for introduction, reduction or campaign for a limited time period. Table 2 summarises the recent changes in the Finnish national immunisation programme and ongoing evaluations initiated by KRAR since 2000. Since the first PCV-7 evaluation, three other vaccines have gone through the critical four-step process. The cost effectiveness evaluation for all these three, i.e., TBE, influenza and rota vaccines, utilising local disease burden and health-care costing data has been favourable (Salo et al. 2006, 2007), unlike in many other European countries, and accordingly, they have been or will be introduced into the national programme.
It goes without saying that evidence-based decision making is here to stay. From 2001 to 2005, the annual national budget for vaccines doubled from 5 to 10 million euros. With all the expected changes (Table 2, i.e., introduction of influenza, rota, varicella, pneumococcus and human papilloma virus vaccines), the budget would increase more than four-fold, up to 43 million euros.
Whether the four-step approach is extensive and fair enough is a matter of present debate. Market forces strongly drive new childhood vaccines, keen on having them used by as many children as possible. When professionals are not in full agreement and decision-making processes slow down, the pharmaceutical industry targets common people raising disease and problem-specific awareness with their advertising campaigns and approaches of opinion leaders and politicians. Sometimes these initiatives can be quite imaginative, taking advantage of parental feelings of guilt and general concerns of health. On the other hand one should not forget that children should have the right to optimal health as declared by the United Nations Special Conference for Children in 2002.
An example of a heated debate on a new vaccine introduction is provided by the present situation of the Human Papilloma Virus (HPV) vaccines in Finland. According to the Finnish Cancer Registry, approximately 150 new cervical cancer cases are detected annually, mostly in women above 25 years of age. Simultaneously 60 deaths are caused by cervical cancer, 90% of which occur in women over 50 years of age. According to the present data, vaccinating girls above 12 years could reduce cervical cancer incidence after 20 years and deaths after 40 years of follow-up. With the experience of the rapid, world-record reduction of cervical cancer screening in Finland since the introduction of the PAP smear screening programme in year 1953 (Fig. 4), the present thinking on the national level is to intensify the already highly successful PAP smear screening. Intensifying screening especially in the younger age groups would most likely have a positive impact on these morbidity and mortality figures much faster than introducing an HPV vaccine, given the fact that the reported overall vaccine efficacy figures of HPV on cervical precancerous lesions caused by all HP viruses is only 27% in non-naïve individuals and that introduction of a vaccine would not bring about savings in the form of reducing screening costs. A multidisciplinary HPV expert group will be called upon to look into detail in these issues and suggest actions to be taken by the government and various stakeholders.
There are increasingly critical voices questioning to what extent economic analyses should be given weight in the decision-making processes. One of the arguments posed is a moral one: children should have the right to the best available health regardless of price. As a consequence, access to new vaccines is seen as part of the rights of a child that a nation should fulfil (Feudtner C and Marcuse E, 2001). Another opposing view is that rather than comparing present vaccination costs to previous ones, it would be more judicious to compare vaccination to other health interventions, especially those targeted to sick people. In 2005 the Finnish government paid approximately 200 € for vaccines per each Finnish child up to 18 years of age (Table 3). This is in striking contrast to the funds spent by the state to cover medical expenses linked to diseases. For example, according the National Health Insurance statistics, in 1 year alone, in 2005, for each of the 9% of Finns officially diagnosed with hyperlipidemia, the Finnish State paid 95–164 € in order to cover the costs of related medications (statins) alone. For such a comparison to be justified and seriously taken into account while resources are limited, a major shift of paradigm would need to take place. Are society and health-care professionals ready for it?
References
Anonymous (2005) Direct and indirect effects of routine vaccine vaccination in children with 7-valent pneumococcal conjugate vaccine on incidence of invasive pneumococcal disease–United States, 1998–2003. MMWR 54:893–897
Black S, Shinefield H, Fireman B et al (2000) Efficacy, safety and immunogenicity of heptavalent pneumococcal conjugate vaccine in children. Pediatr Infect Dis J 19:187–195
Dagan R, Melamed R, Muallem M et al (1996) Reduction of nasopharyngeal carriage of pneumococci during the second year of life by a heptavalent conjugate pneumococcal vaccine. J Infect Dis 1996 174:1271–1278
Eskola J, Käyhty H, Takala AK, Peltola H, Rönnberg PR, Kela E, Pekkanen E, McVerry PH, Mäkelä PH (1990) A randomized, prospective field trial of a conjugate vaccine in the protection of infants and young children against invasive Haemophilus influenzae type b disease. N Engl J Med 323:1381–1387
Eskola J, Peltola H, Käyhty H, Takala AK, Mäkelä PH (1992a) Finnish efficacy trials with Haemophilus influenzae type b vaccines. J Infect Dis 165:S137–S138
Eskola J, Takala AK, Kela E, Pekkanen E, Kalliokoski R, Leinonen M (1992b) Epidemiology of invasive pneumococcal infections in children in Finland. JAMA 268:3323–3327
Eskola J (1996) Rev Med Microbiol 7:231–241
Eskola J, Kilpi T, Palmu A et al (2001) Efficacy of a pneumococcal conjugate vaccine against acute otitis media. N Engl J Med 344:403–409
Feudtner C, Marcuse EK (2001) Ethics and immunization policy: promoting dialogue to sustain consensus. Pediatrics 107:1158–1164
Joensuu J, Koskenniemi E, Pang X-L, Vesikari T (1997) Randomised placebo-controlled trial of rhesus-human reassortant rotavirus vaccine for prevention of severe rotavirus gastroenteritis. Lancet 350:1205–1209
Jokinen C, Heiskanen L, Juvonen H, Kallinen S, Karkola K, Korppi M, Kurki S, Rönnberg PR, Seppä A, Soimakallio S et al (1993) Incidence of community-acquired pneumonia in the population of four municipalities in eastern Finland. Am J Epidemiol 137:977–988
Kilpi T, Herva E, Kaijalainen T, Syrjänen R, Takala AK (2001) Bacteriology of acute otitis media in a cohort of Finnish children followed for the first two years of life. Pediatr Infect Dis J 20:654–662
Kilpi T, Ahman H, Jokinen J et al (2003) Protective efficacy of a second pneumococcal conjugate vaccine against pneumococcal acute otitis media in infants and children: randomized, controlled trial of a 7-valent pneumococcal polysaccharide-meningococcal outer membrane protein complex conjugate vaccine in 1666 children. Clin Infect Dis 37:1155–1164, Epub Oct 7
Nohynek H, Hulkko T, Rapola S, Strömberg N, Kilpi T (2005) Rokottajan käsikirja. Duodecim
Rapola S (2007) National immunization program in Finland. Int J Circumpolar Health 66:382–389
Saarinen M, Takala AK, Koskenniemi E et al (1995) Spectrum of 2,836 cases of invasive bacterial or fungal infections in children: results of prospective nationwide five-year surveillance in Finland. Finnish Pediatric Invasive Infection Study Group. Clin Infect Dis 21:1134–1144
Salo H, Sintonen H, Nuorti JP, Linna M, Nohynek H, Verho J, Kilpi T (2005) Economic evaluation of pneumococcal conjugate vaccination in Finland. Scand J Infect Dis 37:821–832
Salo H, Kilpi T, Sintonen H, Linna M, Peltola V, Heikkinen T (2006) Cost-effectiveness of influenza vaccination of healthy children. Vaccine 24:4934–4941, Epub 2006 Apr 7
Salo H, Ollgren J, Linna M, Sintonen H, Kilpi T (2007) Economic evaluation of rota virus vaccination in Finland. 15th European Conference on Public Health, Helsinki, October 2007
Schmitt HJ, Booy R, Weil-Olivier C, Van Damme P, Cohen R, Peltola H (2003) Child vaccination policies in Europe: a report from the Summits of Independent European Vaccination Experts. Lancet Infect Dis 3:103–108
Takala AK, Eskola J, Peltola H, Mäkelä PH (1989) Epidemiology of invasive Haemophilus influenzae type b disease among children in Finland before vaccination with Haemophilus influenzae type b conjugate vaccine. Pediatr Infect Dis J 8:297–302
Conflict of interest statement
The research team of the author has received research grants from Sanofi Pasteur, PATH and the European Commission DG Research. The author has served as technical expert and received honoraria from these tasks from GlaxoSmithKline, SBLvaccines and Wyeth as well as from governmental and international institutions.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Nohynek, H. The Finnish decision-making process to recommend a new vaccine: From vaccine research to vaccination policy. J Public Health 16, 275–280 (2008). https://doi.org/10.1007/s10389-008-0204-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10389-008-0204-y