Abstract
Background and aim
Endoscopic submucosal dissection (ESD) for early gastrointestinal (GI) cancers is widely performed as a standard treatment in Japan. Given the increasing life expectancy worldwide, it is naturally regarded that the rate of elderly patients diagnosed with early GI cancer has increased. Available guidelines do not specifically outline how to manage endoscopic therapy for the elderly. The aim of this study was to assess the safety and usefulness of ESD for superficial esophageal squamous cell carcinoma (SESCC) in elderly patients.
Methods
We retrospectively investigated 393 consecutive patients, who underwent 426 ESD for 444 SESCCs from January 2011 to August 2016 at our institution. For this study, patients were divided into 2 groups based on their age; ≥ 80 years (Group aged ≥ 80 years, n = 42) and < 80 years (group aged < 80 years, n = 351). Patient demographics, sedation methods, technical outcomes, adverse events, sedatives, dosages given, overall survival, and disease-specific survival were then examined.
Results
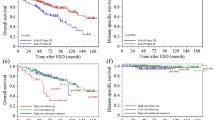
The ESD procedure time was significantly longer for group aged ≥ 80 years than for group aged < 80 years (110 min [range 29–260] vs 85 min [24–504], p = 0.006); however, there was no significant differences between other technical items and adverse events. The 3-year overall survival and disease-specific survival were favorable in both groups.
Conclusions
Esophageal ESD for elderly patients aged ≥ 80 years can be safely performed. Mid-term outcome was favorable. Our study suggests that esophageal ESD might be a useful treatment for SESCCs.


Similar content being viewed by others
References
Gotoda T, Iwasaki M, Kusano C, et al. Endoscopic resection of early gastric cancer treated by guideline and expanded National Cancer Centre criteria. Br J Surg. 2010;97:868–71.
Oda I, Gotoda T, Hamanaka H, et al. Endoscopic submucosal dissection for early gastric cancer: technical feasibility, operation time and complications from a large consecutive series. Dig Endosc. 2005;17:54–8.
Fujishiro M, Kodashima S, Goto O, et al. Endoscopic submucosal dissection for esophageal squamous cell neoplasms. Dig Endosc. 2009;21:109–15.
Saito Y, Kawano H, Takeuchi Y, et al. Current status of colorectal endoscopic submucosal dissection in Japan and other Asian countries: Progressing towards technical standardization. Dig Endosc. 2012;24:67–72.
Gotoda T. Endoscopic resection of early gastric cancer. Gastric Cancer. 2007;10:1–11.
Nonaka S, Oda I, Nakaya T, et al. Clinical impact of a strategy involving endoscopic submucosal dissection for early gastric cancer: determining the optimal pathway. Gastric Cancer. 2011;14:56–62.
Ishihara R, Ishii H, Uedo N, et al. Comparison of EMR and endoscopic submucosal dissection for en bloc resection of early esophageal cancers in Japan. Gastrointest Endosc. 2008;68:1066–72.
Fonkalsrud L, Hwang JH, Khashab MA, et al. Guidelines for sedation and anesthesia in GI endoscopy. Gastrointest Endosc. 2018;87:327–37.
Evans JA, Early DS, Chandraskhara V, et al. The role of endoscopy in the assessment and treatment of esophageal cancer. Gastrointest Endosc. 2013;77:328–44.
Dumonceau JM, Riphaus A, Beilenhoff U, et al. European curriculum for sedation training in gastrointestinal endoscopy: position statement of the European Society of Gastrointestinal Endoscopy (ESGE) and European Society of Gastroenterology and Endoscopy Nurses and Associates (ESGENA). Endoscopy. 2013;45:496–504.
Pimentel-Nunes P, Dinis-Ribeiro M, Ponchon T, et al. Endoscopic submucosal dissection: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy. 2015;47:829–54.
Early DS, Lightdale JR, Vargo JJ, et al. Guidelines for sedation and anesthesia in GI endoscopy. Gastrointest Endosc. 2018;87:327–37.
Sekiguchi M, Oda I, Suzuki H, et al. Clinical outcomes and prognostic factors ingastric cancer patients aged ≥ 85 years undergoing endoscopic submucosal dissection. Gastrointest Endosc. 2017;85:963–72.
Higuchi K, Tanabe S, Azuma M, et al. A phase II study of endoscopic submucosal dissection for superficial esophageal neoplasms (KDOG0901). Gastrointest Endosc. 2013;78:704–10.
Ono S, Fujishiro M, Niimi K, et al. Long-term outcomes of endoscopic submucosal dissection for superficial esophageal squamous cell neoplasms. Gastrointest Endosc. 2009;70:860–6.
Vargo JJ, DeLegge MH, Feld AD, et al. Multisociety sedation curriculum for gastrointestinal endoscopy. American Association for Study of Liver Diseases; American College of Gastroenterology; American Gastroenterological Association Institute; American Society for Gastrointestinal Endoscopy; Society for Gastroenterology Nurses and Associates. Gastrointest Endosc. 2012;76:e1–25.
Japan Esophageal Society. Japanese classification of esophageal cancer, 11th edition: Part I. Esophagus. 2017;14:1–36.
Japan Esophageal Society. Japanese classification of esophageal cancer, 11th edition: Part II and III. Esophagus. 2017;14:37–65.
Kuwano H, Nishimura Y, Oyama T, et al. Guidelines for diagnosis and treatment of carcinoma of the esophagus April 2012 edited by the Japan Esophageal Society. Esophagus. 2015;12:1–30.
Shimizu Y, Takahashi M, Yoshida T, et al. Endoscopic resection (endoscopic mucosal resection/ endoscopic submucosal dissection) for superficial esophageal squamous cell carcinoma: current status of various techniques. Dig Endosc. 2013;25:13–9.
Gambus PL, Jensen EW, Jospin M, et al. Modeling the effect of propofol and remifentanil combinations for sedation-analgesia in endoscopic procedures using an adaptive neuro fuzzy inference system (ANFIS). Anesth Analg. 2011;112:331–9.
Gillham MJ, Hutchinson RC, Carter R, et al. Patient-maintained sedation for ERCP with a target-controlled infusion of propofol: a pilot study. Gastrointest Endosc. 2001;54:14–7.
Peng C, Shen S, Xu G, et al. Efficacy and Safety of endoscopic submucosal dissection for elderly patients with superficial squamous esophageal neoplasms. United Eur Gastroenterol J. 2016;4:242–9.
Song BG, Min YW, Lee JH, et al. Efficacy and Safety of endoscopic submucosal dissection in elderly patients with esophageal squamous cell carcinoma. Surg Endosc. 2017;31:3905–11.
Noh JH, Gong EJ, Kim DH et al. Endoscopic Submucosal dissection for superficial esophageal neoplasms in elderly patients: a single-center, large-scale, retrospective study. Geriatr Gerontol Int. 2020, pp. 1–6 (online ahead of print).
Horiuchi A, Nakayama Y, Tanaka N, et al. Propofol sedation for endoscopic procedures in patients 90 years of age and older. Digestion. 2008;78:20–3.
Jopling MW, Qiu J. Capnography sensor use is associated with reduction of adverse outcomes during gastrointestinal endoscopic procedures with sedation administration. BMC Anesthesiol. 2017;17:157.
Sasaki T, Tanabe S, Azuma M, et al. Propofol sedation with bispectral index monitoring is useful for endoscopic submucosal dissection: a randomized prospective phase II clinical trial. Endoscopy. 2012;44:584–9.
Nakajo I, Abe K, Oda S, et al. Impact of the Charlson Comorbidity Index on the treatment strategy and survival in elderly patients after non-curative endoscopic submucosal dissection for esophageal squamous cell carcinoma: a multicenter retrospective study. J Gastroenterol. 2019;54:871–80.
Onochi K, Shiga H, Takahashi S, et al. Risk factors linking esophageal squamous cell carcinoma with head and neck cancer or gastric cancer. J Clin Gastroenterol. 2019;53:e164–e170170.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical Statement
This study adhered to the ethical principles of the Declaration of Helsinki and was approved by the institutional review board of our institution.
Conflict of interest
The authors declare no conflicts of interest related to this publication.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.

10388_2020_750_MOESM1_ESM.jpg
Figure 3 Metachronous cancer of the esophagus and head & neck. There is no significant difference between group aged ?80 years and group aged <80 years using Kaplan–Meier estimates (JPG 74 kb)
Rights and permissions
About this article
Cite this article
Miyamoto, Y., Nonaka, S., Oda, I. et al. Safety and usefulness of endoscopic submucosal dissection for early esophageal cancers in elderly patients aged 80 years or older. Esophagus 18, 81–89 (2021). https://doi.org/10.1007/s10388-020-00750-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10388-020-00750-9