Abstract
Purpose
To evaluate factors related to myopia progression in children wearing either orthokeratology (OK) lenses or single-vision spectacles (SVS) for 2 years.
Study design
Pooled-analysis retrospective intervention study.
Methods
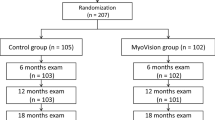
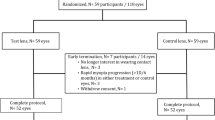
This study involved 105 school-aged children wearing SVS who participated in the multi-center Myovision Study and 89 school-aged children wearing one of 3 OK lens types [Menicon Z Night (M, n = 27), αORTHO®-K (A, n = 32), and Emerald™ (E, n = 30)]. In the OK-lens patients, last examination was performed at ≥ 3-weeks post lens-wear discontinuation. Of the subjects, 102 SVS-Group and 79 OK-Group (M: n = 24, A: n = 28, and E: n = 27) children completed all examinations. A relationship between refractive error (RE) change and 7 factors (correction methods, baseline age, baseline RE, baseline axial length, gender, right or left eye, and follow-up period) was derived by multiple regression modeling. Via those same methods, we investigated the relationship between RE change and 7 factors including 3 OK-lens corrections.
Results
Related influence factors were correction method (0.85 D myopia reduction in the OK Group, P < 0.001), baseline age (0.16 D myopia reduction in older-age patients, P < 0.001), and baseline RE (0.12 D myopia reduction per 1 D myopia, P = 0.01). No relationship was found between RE change and OK-lens type. No serious adverse events occurred.
Conclusion
Regardless of OK lens design, myopia progression in school-aged children was suppressed. The effect was examined not only via axial-length elongation but also RE change, and the myopia control effect by OK lenses was found to be 0.85 D over the 2-year period.




Similar content being viewed by others
References
Holden BA, Fricke TR, Wilson DA, Jong M, Naidoo KS, Sankaridurg P, et al. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology. 2016;123:1036–42.
Pan CW, Klein BE, Cotch MF, Shrager S, Klein R, Folsom A, et al. Racial variations in the prevalence of refractive errors in the United States: the multi-ethnic study of atherosclerosis. Am J Ophthalmol. 2013;155:1129–38.
Morgan I, Rose K. How genetic is school myopia? Prog Retin Eye Res. 2005;24:1–38.
Morita H, Ideta H, Ito K, Yonemoto J, Sasaki K, Tanaka S. Causative factors of retinal detachment in macular holes. Retina. 1991;11:281–4.
Resnikoff S, Pascolini D, Mariotti SP, Pokharel GP. Global magnitude of visual impairment caused by uncorrected refractive errors in 2004. Bull World Health Organ. 2008;86:63–70.
Tan NW, Saw SM, Lam DS, Cheng HM, Rajan U, Chew SJ. Temporal variations in myopia progression in Singaporean children within an academic year. Optom Vis Sci. 2000;77:465–72.
Fan DS, Lam DS, Lam RF, Lau JT, Chong KS, Cheung EY, et al. Prevalence, incidence, and progression of myopia of school children in Hong Kong. Invest Ophthalmol Vis Sci. 2004;45:1071–5.
Donovan L, Sankaridurg P, Ho A, Naduvilathet T, Smith EL 3rd, Holden BA. Myopia progression rates in urban children wearing single-vision spectacles. Optom Vis Sci. 2012;89:27–32.
Grzybowski A, Kanclerz P, Tsubota K, Lanca C, Saw SM. A review on the epidemiology of myopia in school children worldwide. BMC Ophthalmol. 2020;14:27.
Smith EL 3rd, Kee CS, Ramamirtham R, Qiao-Grider Y, Hung LF. Peripheral vision can influence eye growth and refractive development in infant monkeys. Invest Ophthalmol Vis Sci. 2005;46:3965–72.
Smith EL 3rd, Ramamirtham R, Qiao-Grider Y, Hung LF, Huang J, Kee CS, et al. Effects of foveal ablation on emmetropization and form-deprivation myopia. Invest Ophthalmol Vis Sci. 2007;48:3914–22.
Huang J, Hung LF, Ramamirtham R, Blasdel TL, Humbird TL, Bockhorst KH, et al. Effects of from deprivation on peripheral refractions and ocular shape in infant rhesus monkeys (Macaca mulatta). Invest Ophthalmol Vis Sci. 2009;50:4033–44.
Choo JD, Caroline PJ, Harlin DD, Papas EB, Holden BA. Morphologic changes in cat epithelium following continuous wear of orthokeratology lenses: a pilot study. Cont Lens Anterior Eye. 2008;31:29–37.
González-Méijome JM, Faria-Ribeiro MA, Lopes-Ferreira DP, Fernandes P, Carracedo G, Queiros A. Changes in peripheral refractive profile after orthokeratology for different degrees of myopia. Curr Eye Res. 2016;41:199–207.
Sankaridurg P, Holden B, Smith E 3rd, Naduvilath T, Chen X, de la Jara PL, et al. Decrease in rate of myopia progression with contact lenses to reduce relative peripheral hyperopia: one-year results. Invest Ophthalmol Vis Sci. 2011;52:9362–7.
Hiraoka T, Kakita T, Okamoto F, Oshika T. Influence of ocular wavefront aberrations on axial length elongation in myopic children treated with overnight orthokeratology. Ophthalmology. 2015;122:93–100.
Kang P, Gifford P, McNamara P, Wu J, Yeo S, Vong B, et al. Peripheral refraction in different ethnicities. Invest Ophthalmol Vis Sci. 2010;51:6059–65.
Scheiman M, Gwiazda J, Zhang Q, Deng L, Fern K, Manny RE, and the COMET Group, et al. Longitudinal changes in corneal curvature and its relationship to axial length in the Correction of Myopia Evaluation Trial (COMET) cohort. J Optom. 2016;9:13–21.
Kakita T, Hiraoka T, Oshika T. Influence of overnight orthokeratology on axial elongation in childhood myopia. Invest Ophthalmol Vis Sci. 2011;52:2170–4.
Hiraoka T, Kakita T, Okamoto F, Takahashi H, Oshika T. Long-term effect of overnight orthokeratology on axial length elongation in childhood myopia: a 5-year follow-up study. Invest Ophthalmol Vis Sci. 2012;53:3913–9.
Cho P, Cheung SW. Retardation of myopia in orthokeratology (ROMIO) study: a randomized controlled trial. Invest Opthalmol Vis Sci. 2012;53:7077–85.
Cho P, Cheung SW, Edwards M. The longitudinal orthokeratology research in children (LORIC) in Hong Kong. A pilot study on refractive changes and myopic control. Curr Eye Res. 2005;30:71–80.
Santodomingo-Rubido J, Villa-Collar C, Gilmartin B, Gutiérrez-Ortega R. Myopia control with orthokeratology contact lenses in Spain: refractive and biometric changes. Invest Ophthalmol Vis Sci. 2012;53:5060–5.
Chen C, Cheung SW, Cho P. Myopia control using toric orthokeratology (TO-SEE study). Invest Ophthalmol Vis Sci. 2013;54:6510–7.
Huang J, Wen D, Wang Q, McAlinden C, Flitcroft I, Chen H, et al. Efficacy comparison of 16 interventions for myopia control in children: A network meta-analysis. Ophthalmology. 2016;123:697–708.
Walline JJ, Lindsley KB, Vedula SS, Cotter SA, Mutti DO, Twelker JD. Interventions to slow progression of myopia in children. Cochrane Database Syst Rev. 2011. https://doi.org/10.1002/14651858.CD004916.pub3.
Maekawa H, Hieda O, Nakamura Y, Koizumi N, Kinoshita S. Examination of the correction effect of orthokeratology to suppress the progression of myopia in Japanese schoolchildren. Jpn J Vis Sci. 2016;37:83–7.
Kanda H, Oshika T, Hiraoka T, Hasebe S, Ohno-Matsui K, Ishiko S, et al. Effect of spectacle lenses designed to reduce relative peripheral hyperopia on myopia progression in Japanese children: a 2-year multicenter randomized controlled trial. Jpn J Ophthalmol. 2018;62:537–43.
Saw SM, Chua WH, Gazzard G, Koh D, Tan DT, Stone RA. Eye growth changes in myopic children in Singapore. Br J Ophthalmol. 2005;89:1489–94.
Donovan L, Sankaridurg P, Ho A, Naduvilath T, Smith EL 3rd, Holden BA. Myopia progression rates in urban children wearing single-vision spectacles. Optom Vis Sci. 2012;89:27–32.
Hyman L, Gwiazda J, Hussein M, Norton TT, Wang Y, Marsh-Tootle W, et al. Relationship of age, sex, and ethnicity with myopia progression and axial elongation in the correction of myopia evaluation trial. Arch Ophthalmol. 2005;123:977–87.
Cho P, Cheung SW. Protective Role of orthokeratology in reducing risk of rapid axial elongation: A reanalysis of data from the ROMIO and TO-SEE studies. Invest Ophthalmol Vis Sci. 2017;58:1411–6.
Saw SM, Nieto FJ, Katz J, Schein OD, Levy B, Chew SJ. Factors related to the progression of myopia in Singaporean children. Optom Vis Sci. 2000;77:549–54.
Braun CI, Freidlin V, Sperduto RD, Milton RC, Strahlman ER. The progression of myopia in school age children: data from the Columbia Medical Plan. Ophthalmol Epidemiol. 1996;3:13–21.
Watanabe S, Yamashita T, Ohba N. A longitudinal study of cycloplegic refraction in a cohort of 350 Japanese schoolchildren. Cycloplegic refraction. Oph Phys Opt. 1999;19:22–9.
Zhong Y, Chen Z, Xue F, Miao H, Zhou X. Central and peripheral corneal power change in myopic orthokeratology and its relationship with 2-year axial length change. Invest Ophthalmol Vis Sci. 2015;56:4514–9.
Cho P, Chan B, Cheung SW, Mountford J. Do fenestrations affect the performance of orthokeratology lenses? Optom Vis Sci. 2012;89:401–10.
Lau JK, Vincent SJ, Cheung S-W, Cho P. Higher-order aberrations and axial elongation in myopic children treated with orthokeratology. Invest Ophthalmol Vis Sci. 2020;61(2):22.
Kang P, Swarbrick H. The influence of different OK lens designs on peripheral refraction. Optom Vis Sci. 2016;93:1112–9.
Kobayashi Y, Yanai R, Chikamoto N, Chikama T, Ueda K, Nishida T. Reversibility of effects of orthokeratology on visual acuity, refractive error, corneal topography, and contrast sensitivity. Eye Contact Lens. 2008;34:224–8.
Nakamura Y, Hieda O, Nakai Y, Kinoshita S. Myopia control with orthokeratology contact lens. J Jpn CL Soc. 2014;56:19–22.
Matsubara M, Kamei Y, Takeda S, Mukai K, Ishii Y, Ito S. Histologic and histochemical changes in rabbit cornea produced by an orthokeratology lens. Eye Contact Lens. 2004;30:198–204.
Cheung SW, Cho P. Long-term effect of orthokeratology on the anterior segment length. Cont Lens Anterior Eye. 2016;39:262–5.
Acknowledgements
The authors appreciate the members of Multi-Center Clinical Trial of the Myovision Study Group (T. Fujikado, H. Kanda, T. Oshika, T. Hiraoka, S. Hasebe, K. Ohno-Matsui, S. Ishiko, and H. Torii) who provided the control data. The authors wish to thank John Bush for reviewing the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
Y. Nakamura, None; O. Hieda, None; I. Yokota, None; S. Teramukai, None; C. Sotozono, Lecture fee (Otsuka, Santen, Senju, TOA); S. Kinoshita, Lecture fee (Otsuka, Santen, Senju, Kowa), Senju and the author own the patent for the use of ROCK inhibitor. CorneaGen and the author own the patent for the use of ROCK inhibitor. Santen and the author own the patent for glaucoma-related genes. Sysmex and the author are applicants for the patent for SJS-related genes.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Corresponding Author: Yo Nakamura
Supplementary Information
Below is the link to the electronic supplementary material.
10384_2021_854_MOESM2_ESM.tif
Supplementary file2 Supplementary Fig. 1a RE change over the 2-year study period in the OK Group only (subgroup analysis). There was no significant difference in RE change among the three different-type design OK lens groups (right eye: P = 0.47, left eye: P = 0.38, one-way ANOVA). Dot filled square box: Right eye, Slant line filled square box: Left eye. (TIF 81 kb)
10384_2021_854_MOESM3_ESM.tif
Supplementary file3 Supplementary Fig. 1b AL elongation over the 2-year study period in the OK Group only (subgroup analysis). There was no significant difference in AL elongation among the three different-type design OK lens groups (right eye: P = 0.65, left eye: P = 0.38, one-way ANOVA). Dot filled square box: Right eye, Slant line filled square box: Left eye. (TIF 80 kb)
About this article
Cite this article
Nakamura, Y., Hieda, O., Yokota, I. et al. Comparison of myopia progression between children wearing three types of orthokeratology lenses and children wearing single-vision spectacles. Jpn J Ophthalmol 65, 632–643 (2021). https://doi.org/10.1007/s10384-021-00854-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10384-021-00854-4