Purpose
There is no definite consensus on the management of intra-abdominal abscesses in adults. This retrospective study evaluated the use of antibiotic therapy and percutaneous image-guided drainage in adult patients with intra-abdominal abscesses.
Methods
A retrospective chart review of 114 patients with intra-abdominal abscesses was conducted. Data collected included patient demographics, presenting symptoms, radiographic interpretation, vital signs, antibiotic coverage, laboratory values, and details of the hospital course. Bivariate statistical tests were performed using the Wilcoxon rank-sum test, chi-squared test, or Fisher's exact test, where appropriate.
Results
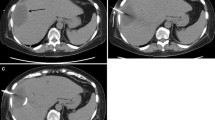
Sixty-seven of 114 patients (59 percent) had intra-abdominal abscesses resulting from appendicitis, diverticulitis in 30 patients (26 percent), postoperative in 13 patients (11 percent), and undetermined in 4 patients (4 percent). Three patients (3 percent; 95 percent confidence interval, 1–8 percent) failed conservative management and underwent urgent operation. Sixty-one (54 percent; 95 percent confidence interval, 44–63 percent) patients improved with intravenous antibiotic therapy alone. Fifty patients (44 percent; 95 percent confidence interval, 35–54 percent) underwent image-guided percutaneous drainage after 48 to 72 hours of antibiotic therapy. Patients who improved on antibiotics alone had average abscess diameter of 4 cm, whereas patients who underwent percutaneous drainage had average diameter of 6.5 cm (P < 0.0001). Maximal temperature at time of admission was 100.8°F for antibiotic group and 101.2°F for percutaneous drainage group (P = 0.0067).
Conclusions
The majority of the patients with intra-abdominal abscesses improved with antibiotic therapy alone. Those patients with an abscess diameter >6.5 cm and temperature at admission >101.2°F have higher likelihood of failing conservative therapy with antibiotics alone and requiring percutaneous drainage.

Similar content being viewed by others
References
WA Altemeier WR Culbertson WD Fullen CD Shook (1973) ArticleTitleIntra-abdominal abscess Am J Surg 125 70–79 Occurrence Handle10.1016/0002-9610(73)90010-X Occurrence Handle1:STN:280:DyaE3s%2FnsVyjtQ%3D%3D Occurrence Handle4566907
SG Gerzof AH Robbins WC Johnson DH Birkett DC Nabseth (1981) ArticleTitlePercutaneous catheter drainage of abdominal abscesses: a five-year experience N Engl J Med 305 653–657 Occurrence Handle1:STN:280:DyaL3M3ntVGruw%3D%3D Occurrence Handle7266601 Occurrence Handle10.1056/NEJM198109173051201
WC Johnson SG Gerzof AH Robbins DC Nabseth (1981) ArticleTitleTreatment of abdominal abscess: comparative evaluation of operative drainage versus percutaneous catheter drainage guided by computed tomography or ultrasound Ann Surg 194 510–520 Occurrence Handle1:STN:280:DyaL38%2Fit1Gguw%3D%3D Occurrence Handle7283510
A Hemming NL Davis RE Robins (1991) ArticleTitleSurgical versus percutaneous drainage of intra-abdominal abscesses Am J Surg 161 593–595 Occurrence Handle10.1016/0002-9610(91)90907-U Occurrence Handle1:STN:280:DyaK3M3jtl2qug%3D%3D Occurrence Handle2031543
DM Bamberger (1996) ArticleTitleOutcome of medical treatment of bacterial abscesses without therapeutic drainage: a review of cases reported in the literature Clin Infect Dis 23 604–607
Y Heloury M Baron S Bourgoin O Wetzel C Lejus V Plattner (1995) ArticleTitleMedical treatment of postappendectomy intraperitoneal abscesses in children Eur J Pediatr Surg 5 149–151 Occurrence Handle1:STN:280:DyaK28%2FlsFKgsw%3D%3D Occurrence Handle7547800 Occurrence Handle10.1055/s-2008-1066191
BO Okoye B Rampersad A Marantos LJ Abernethy PD Losty DA Lloyd (1998) ArticleTitleAbscess after appendectomy in children: the role of conservative management Br J Surg 85 1111–1113 Occurrence Handle10.1046/j.1365-2168.1998.00782.x Occurrence Handle1:STN:280:DyaK1czot1Wjug%3D%3D Occurrence Handle9718008
MJ Lee HC Lee W Young JC Sheu PY Chang NL Wang (1998) ArticleTitleConservative treatment of intra-abdominal abscess in children Zhonghua Min Guo Xiao Er Ke Yi Xue Hui Za Zhi 39 301–305 Occurrence Handle1:STN:280:DyaK1M%2FktFSjug%3D%3D Occurrence Handle9823674
ED Ralph (1984) ArticleTitleSuccessful antimicrobial therapy of hepatic, intra-abdominal and intra-pelvic abscesses Can Med Assoc J 131 605–607 Occurrence Handle1:STN:280:DyaL2M%2FgtFKksg%3D%3D Occurrence Handle6383589
P Ambrosetti J Robert JA Witzig et al. (1992) ArticleTitleIncidence, outcome, and proposed management of isolated abscesses complicating acute left-sided colonic diverticulitis: a prospective study of 140 patients Dis Colon Rectum 35 1072–1076 Occurrence Handle10.1007/BF02252998 Occurrence Handle1:STN:280:DyaK3s%2FkvVCntA%3D%3D Occurrence Handle1425052
S Benoist Y Panis V Pannegeon et al. (2004) ArticleTitleCan failure of percutaneous drainage of postoperative abdominal abscesses be predicted? Am J Surg 184 148–153 Occurrence Handle10.1016/S0002-9610(02)00912-1
MM Maher DA Gervais MK Kalra et al. (2004) ArticleTitleThe inaccessible or undrainable abscess: how to drain it Radiographics 24 717–735 Occurrence Handle15143224
MR Dixon JS Haukoos IU Park et al. (2003) ArticleTitleAn assessment of the severity of recurrent appendicitis Am J Surg 186 718–722 Occurrence Handle10.1016/j.amjsurg.2003.08.016 Occurrence Handle14672785
WD Wong SD Wexner A Lowry et al. (2000) ArticleTitlePractice parameters for the treatment of sigmoid diverticulitis—supporting documentation. The Standards Task Force. The American Society of Colon and Rectal Surgeons Dis Colon Rectum 43 290–297 Occurrence Handle10.1007/BF02258291 Occurrence Handle1:STN:280:DC%2BD3c7psFantA%3D%3D Occurrence Handle10733108
AJ Minardi LW Johnson JK Sehon GB Zibari JC McDonald (2001) ArticleTitleDiverticulitis in the young patient Am Surg 67 458–461 Occurrence Handle11379649
PV Vignati JP Welch JL Cohen (1995) ArticleTitleLong-term management of diverticulitis in young patients Dis Colon Rectum 38 627–629 Occurrence Handle10.1007/BF02054123 Occurrence Handle1:STN:280:DyaK2M3pt1yhug%3D%3D Occurrence Handle7774475
DA Gervais CH Ho MJ O'Neill RS Arellano PF Hahn PR Mueller (2004) ArticleTitleRecurrent abdominal and pelvic abscesses: incidence, results of repeated percutaneous drainage, and underlying causes of 956 drainages Am J Roentgenol 182 463–466
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Kumar, R.R., Kim, J.T., Haukoos, J.S. et al. Factors Affecting the Successful Management of Intra-Abdominal Abscesses With Antibiotics and the Need for Percutaneous Drainage. Dis Colon Rectum 49, 183–189 (2006). https://doi.org/10.1007/s10350-005-0274-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10350-005-0274-7