PURPOSE:
Expandable, metallic stents provide a new modality of palliation for patients with noncurable metastatic colorectal adenocarcinoma. This study was designed to compare the use of expandable metallic stents as a palliative measure to traditional open surgical management, with particular reference to length of stay, and survival.
METHODS:
Patients admitted between 1997 and 2002 with left-sided (splenic flexure and distal), colorectal adenocarcinoma and nonresectable metastatic disease (Stage 4) were treated with expandable metal stents or open surgery (resection, bypass, or stoma). The group of patients having stents inserted were compared with regard to perioperative outcome and survival to those having open surgical procedures.
RESULTS:
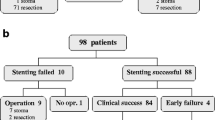
Twenty-two of 25 patients had colonic stents successfully inserted and 19 patients underwent open surgery. The two groups were comparable: stent: median age, 66 (range, 37–88) years; 13 males; and open operation: median age, 68 (range, 51–85) years; 12 males. The tumors were primary in 22 stents procedures and 18 open operations. The site of obstruction was: splenic flexure, 2 stent vs. 0 open operation; descending colon, 2 stent vs. 2 open operation; sigmoid colon, 12 stent vs. 6 open operation; rectum, 9 stent vs. 11 open operation. The American Society of Anesthesiologists (ASA) class was: ASA 1, 0 stent vs. 0 open operation; ASA 2, 6 stent vs. 9 open operation; ASA 3, 15 stent vs. 7 open operation; ASA 4, 4 stent vs. 3 open operation. The open operations were laparotomy only (n = 2), bypass (n = 1), stoma (n = 7), resection with anastomosis (n = 4), resection without anastomosis (n = 5). The complications after open operation were urinary (n = 2), stroke (n = 1), cardiac (n = 2), respiratory (n = 2), deep vein thrombosis (n = 1), anastomotic leak (n = 1). There were no stent-related complications. The mean length of stay was significantly shorter in the stent group (4 vs. 10.4 days; P < 0.0001). There was no difference in survival between the two groups (median survival: stent group, 7.5 months; open operation, 3.9 months; log-rank P value = 0.2156).
CONCLUSIONS:
Patients treated with stents are discharged earlier than after open surgery. Stents do not affect survival. Expandable metal stents provide an acceptable alternative and may be better than traditional open surgical techniques.


Similar content being viewed by others
REFERENCES
American Joint Committee on Cancer. AJCC cancer staging manual. 5th ed. Philadelphia: Lippincott-Raven, 1997.
SK Liu JM Church IC Lavery VW Fazio (1997) ArticleTitleOperation in patients with incurable colon cancer - is it worthwhile? Dis Colon Rectum 40 11–4 Occurrence Handle1:STN:280:ByiB38jpvFI%3D Occurrence Handle9102251
J Môkelô K Haukipuro S Laitinen MI Kairaluoma (1990) ArticleTitlePalliative operations for colorectal cancer Dis Colon Rectum 33 846–50 Occurrence Handle1698594
J Joffe PH Gordon (1981) ArticleTitlePalliative resection for colorectal carcinoma Dis Colon Rectum 24 355–60 Occurrence Handle1:STN:280:Bi6B28%2FhvVA%3D Occurrence Handle6167412
WH Isbister (2002) ArticleTitleAudit of definitive colorectal surgery in patients with early and advanced colorectal cancer ANZ J Surg 72 271–4 Occurrence Handle11982513
SA Rosen JF Buell A Yoshida et al. (2000) ArticleTitleInitial presentation with stage IV colorectal cancer. How aggressive should we be? Arch Surg 135 530–5 Occurrence Handle1:STN:280:DC%2BD3c3msFGmtA%3D%3D Occurrence Handle10807276
CR Scoggins IM Meszoely CD Blanke RD Beauchamp SD Leach (1999) ArticleTitleNonoperative management of primary colorectal cancer in patients with stage IV disease Ann Surg Oncol 6 651–7 Occurrence Handle1:STN:280:DC%2BD3c%2FitlGjtA%3D%3D Occurrence Handle10560850
GJ Harris AJ Senagore IC Lavery JM Church VW Fazio (2002) ArticleTitleFactors affecting survival after palliative resection of colorectal carcinoma Colorectal Dis 4 31–5 Occurrence Handle12780652
SD Fitzgerald WE Longo GL Daniel AM Vernava SuffixIII (1993) ArticleTitleAdvanced colorectal neoplasia in the high-risk elderly patient: is surgical resection justified? Dis Colon Rectum 36 161–6 Occurrence Handle1:STN:280:ByyC2crnvVA%3D Occurrence Handle8425420
IM Leitman JD Sullivan D Brams JJ DeCrosse (1992) ArticleTitleMultivariate analysis of morbidity and mortality from the initial surgical management of obstructing carcinoma of the colon Surg Gynecol Obstet 174 513–8 Occurrence Handle1:STN:280:By2B2sbovFY%3D Occurrence Handle1595029
F Camúñez A Echenagusia G Simó F Turégano J Vázquez I Barreiro-Meiro (2000) ArticleTitleMalignant colorectal obstruction treated by means of self-expanding metallic stents: effectiveness before surgery and in palliation Radiology 216 492–7
MA Gregorio ParticleDe A Mainer E Tejero et al. (1998) ArticleTitleAcute colorectal obstruction: stent placement for palliative treatment – results of a multicenter study Radiology 209 117–20 Occurrence Handle9769821
SJ Cole P Boorman H Osman N Sathananthan MC Parker (2000) ArticleTitleEndoluminal stenting for relief of colonic obstruction is safe and effective Colorectal Dis 2 282–7
R Fernández Lobato I Pinto L Paul E Tejero C Montes (1999) ArticleTitleFernández L et al. Self-expanding prostheses as a palliative method in treating advanced colorectal cancer Int Surg 84 159–62 Occurrence Handle1:STN:280:DyaK1MzjsVOktg%3D%3D Occurrence Handle10408289
UP Khot A Wenk Lang K Murali MC Parker (2002) ArticleTitleSystematic review of the efficacy and safety of colorectal stents Br J Surg 89 1096–102 Occurrence Handle10.1046/j.1365-2168.2002.02148.x Occurrence Handle1:STN:280:DC%2BD38vjsVWjug%3D%3D Occurrence Handle12190673
AS Keats (1978) ArticleTitleThe ASA classification of physical status: a recapitulation Anesthesiology 49 233–6 Occurrence Handle1:STN:280:CSaD3Mbjslw%3D Occurrence Handle697075
FA Frizelle (1995) Postoperative fatigue [master’s thesis]. University of Otago: Dunedin New Zealand
J Boey TK Choi J Wong GB Ong (1981) ArticleTitleCarcinoma of the colon and rectum with liver involvement Surg Gynecol Obstet 153 864–8 Occurrence Handle1:STN:280:Bi2D283islw%3D Occurrence Handle6171042
LP Díaz IP Pabón RF Lobato CM López (1999) ArticleTitlePalliative treatment of malignant colorectal strictures with metallic stents Cardiovasc Intervent Radiol 22 29–36 Occurrence Handle10.1007/s002709900325 Occurrence Handle9929542
WR Johnson FT McDermott E Pihl BJ Milne AB Price ES Hughes (1981) ArticleTitlePalliative operative management in rectal carcinoma Dis Colon Rectum 24 606–9 Occurrence Handle1:STN:280:Bi2D1MvntVI%3D Occurrence Handle6172244
BM Jaffe WL Donegan F Watson JS Spratt (1968) ArticleTitleFactors influencing survival in patients with untreated hepatic metastases Surg Gynecol Obstet 127 1–11 Occurrence Handle1:STN:280:CCeA3M%2FptFM%3D Occurrence Handle5657778
B Cady DO Monson NW Swinton (1970) ArticleTitleSurvival of patients after colonic resection for carcinoma with simultaneous liver metastases Surg Gynecol Obstet 131 697–700 Occurrence Handle1:STN:280:CS%2BB1M%2FitVE%3D Occurrence Handle5458530
S Bengmark L Hafström (1969) ArticleTitleThe natural history of primary and secondary malignant tumours of the liver. I. The prognosis for patients with hepatic metastases from colonic and rectal carcinoma by laparotomy Cancer 1 198–202
HJ Wanebo C Semoglou F Attiyeh MJ Stearns (1978) ArticleTitleSurgical management of patients with primary operable colorectal cancer and synchronous liver metastases Am J Surg 135 81–5 Occurrence Handle1:STN:280:CSeC3c7hsVw%3D Occurrence Handle623377
CB Wood CR Gillis LH Blumgart (1976) ArticleTitleA retrospective study of the natural history of patients with liver metastases from colorectal cancer Clin Oncol 2 285–8 Occurrence Handle1:STN:280:CSiD1M%2FgsV0%3D Occurrence Handle1009711
G Bengtsson G Carlsson L Hafström P-E Jönsson (1981) ArticleTitleNatural history of patients with untreated liver metastases from colorectal cancer Am J Surg 141 586–9 Occurrence Handle1:STN:280:Bi6C1c7ls1I%3D Occurrence Handle7223955
M Palmer NJ Petrelli L Herrera (1989) ArticleTitleNo treatment option for liver metastases from colorectal adenocarcinoma Dis Colon Rectum 32 698–701 Occurrence Handle1:STN:280:BiaA38vovV0%3D Occurrence Handle2752858
EM Oxley H Ellis (1969) ArticleTitlePrognosis of carcinoma of the large bowel in the presence of liver metastases Br J Surg 56 149–52 Occurrence Handle1:STN:280:CCaC3Mzitlc%3D Occurrence Handle4179553
WE Longo GH Ballantyne AJ Bilchik IM Modlin (1988) ArticleTitleAdvanced rectal cancer. What is the best palliation? Dis Colon Rectum 31 842–7 Occurrence Handle1:STN:280:BiaD3s%2FhtFI%3D Occurrence Handle2460299
MR Moran DA Rothenberger CJ Lahr JG Buls SM Goldberg (1987) ArticleTitlePalliative resection for rectal cancer. Resection? Anastomosis? Arch Surg 122 640–3 Occurrence Handle1:STN:280:BiiB3M3ltFQ%3D Occurrence Handle2437881
RJ Baigrie AR Berry (1994) ArticleTitleManagement of advanced rectal cancer Br J Surg 81 343–52 Occurrence Handle1:STN:280:ByuB38fisVA%3D Occurrence Handle7513600
JW Milsom SH Kim KA Hammerhofer VW Fazio (2000) ArticleTitleLaparoscopic colorectal cancer surgery for palliation Dis Colon Rectum 43 1512–6 Occurrence Handle1:STN:280:DC%2BD3M%2Fkt1GjtA%3D%3D Occurrence Handle11089584
J Lumley R Stitz A Stevenson G Fielding A Luck (2002) ArticleTitleLaparoscopic colorectal surgery for cancer Dis Colon Rectum 45 867–72 Occurrence Handle10.1007/s10350-004-6318-6 Occurrence Handle12130871
F Feliciotti AM Paganini M Guerrieri A Sanctis R Campagnacci E Lezoche (2002) ArticleTitleresults of laparoscopic vs. open resections for colon cancer in patients with a minimum follow-up of 3 years Surg Endosc 16 1158–61 Occurrence Handle10.1007/s00464-001-8333-1 Occurrence Handle1:STN:280:DC%2BD38vjt1ehsA%3D%3D Occurrence Handle11984684
InstitutionalAuthorNameAnonymous (2002) ArticleTitleLaparoscopic versus open surgery for colorectal carcinoma: a prospective clinical trial involving 157 cases with a mean follow-up of 5 years. Surg Laparosc Endosc Percutan Tech 12 88–95
KL Leung RY Yiu PB Lai JF Lee KH Thung WY Lau (1999) ArticleTitleLaparoscopic-assisted resection of colorectal carcinoma: five year audit Dis Colon Rectum 42 327–32 Occurrence Handle1:STN:280:DyaK1M3jvValtQ%3D%3D Occurrence Handle10223751
JC Weeks H Helson S Gelber D Sargent G Schroeder (2002) ArticleTitleClinical Outcomes of Surgical Therapy (COST) Study Group. Short-term quality of life outcomes following laparoscopic-assisted colectomy vs open colectomy for colon cancer: a randomized trial JAMA 287 321–8 Occurrence Handle10.1001/jama.287.3.321 Occurrence Handle11790211
ACKNOWLEDGMENTS
The authors thank Dr. B. Dobbs for statistical analysis and Ms. Melanie Thornton for help with data collection.
Author information
Authors and Affiliations
Corresponding author
Additional information
Reprints are not available.
About this article
Cite this article
Carne, P., Frye, J., Robertson, G. et al. Stents or Open Operation for Palliation of Colorectal Cancer: A Retrospective, Cohort Study of Perioperative Outcome and Long-term Survival. Dis Colon Rectum 47, 1455–1461 (2004). https://doi.org/10.1007/s10350-004-0624-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10350-004-0624-x