Abstract
The coronavirus 2019 pandemic, induced by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has strongly altered healthcare systems and the economy worldwide. The lack of knowledge on this virus has led to the implementation of uncertain strategies and measures to fight the pandemic. Here, we review environmental factors that control viral transmission, such as air, temperature, humidity, food, water and sewage, insects, inanimate surfaces, hand hygiene, and social distancing. The main route of viral transmission is the respiratory tract through aerosols. Masks and social distancing are effective in ceasing air transmission. Proper cleaning of surfaces and hand disinfection are required, especially in healthcare units. Food should be handled properly, and food handlers should work based on hygienic protocols. Water and sewage transmission, and transmission through insects appear less important than other environmental factors.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In the last decades, the appearance of viral infections with pandemic potential as severe acute respiratory syndrome coronavirus 1 (SARS-CoV-1), Middle East respiratory syndrome coronavirus (MERS), influenza, and ebola posed a significant threat to human life. The outbreak of the SARS-CoV-2 led to millions of deaths all over the world and worsened the financial crisis. The SARS-CoV-2 virus belongs to coronaviruses and is a single-stranded positive-sense RNA virus that causes the coronavirus disease 2019 infection (COVID-19 Eslami and Jalili 2020).
The infection may lead to multi-system failure with evidence suggesting that SARS-CoV-2-mediated endothelial injury, thus, can be considered not only a respiratory but also a vascular disease. Over the past few months and with the appearance of novel scientific knowledge from research, new therapeutic methods have been proposed and tested for managing the disease (“COVID-19 and vascular disease,” 2020; Siddiqi et al. 2021).
Infected patients may be presented even in the early stage of disease with symptoms such as fever, cough, myalgia, fatigue, generalized weakness, sputum production, headache, sore throat, and dyspnea. Less commonly, patients may present with gastrointestinal tract symptoms such as diarrhea, vomiting, hemoptysis, and dizziness. Several cases may present with anosmia and ageusia (Han et al. 2020a, b; Huang et al. 2020; Vaira et al. 2020).
Indeed, asymptomatic carriers who may transfer the virus worsen the epidemiological picture and render the prophylaxis from infected individuals more difficult. Personal protective equipment such as masks, respirators, gloves, gowns, and body covers for the healthcare workers in combination with social isolation still is the most critical measurements for preventing the infection. In detail, their use may contribute to the prevention of the invasion of virus particles into the system of an individual, which is most critical for healthcare workers. Hand hygiene and disinfection of surfaces still play a significant role in the level of prophylaxis (Mahmood et al. 2020).
Except for personal protective equipment, we should focus on some environmental factors such as temperature, humidity, food, water, sewage, air, insects, inanimate surfaces, and hand hygiene which may also contribute to the transmission of the infection. The role of these factors should be investigated to understand their importance and help to reduce the transmission of the virus and subsequently to combat the COVID-19 outbreak (Eslami and Jalili 2020).
There are four ways of transmission of infectious diseases: (1) direct contact with infected individuals, (2) indirect contact via fomites, (3) droplet transmission, and (4) airborne transmission via aerosolized particles (Leung 2021). Heating, ventilation, and air conditioning systems are used as primary infection disease control measures; nevertheless, in case of improper use, they may contribute to the airborne transmission of infections (Correia et al. 2020).
We already know that winter is a more favorable season for infections as influenza virus compared to summer. That is why it is observed that the cases of people infected decrease in the summer months. The role of weather alterations, temperature, and relative humidity in correlation with SARS-CoV-2 transmission should be investigated carefully (Mathur et al., 2014). This article aims to the presentation of the environmental factors which play the most significant for the transmission of infections and scrutinize the extent of their role in the transmission of the SARS-CoV-2 virus (Eslami and Jalili 2020).
Review methodology
The relevant articles were searched on August 2021 on PubMed and Google Scholar using the search terms “SARS-CoV-2,” AND “coronavirus,” OR “environmental factors,” OR “temperature,” OR “humidity,” OR “personal protective equipment,” OR “SARS,” OR “MERS” in the title and abstract. All the screened publications were classified and analyzed.
The eligible articles were from the last two years, which provided information about the research topic. Some reports from the past were also selected, which concerned other viruses of the same and different families, to what extent the environmental factors affect their survival, and ways to combat them as social distancing, personal protective equipment, and proper hygiene and cleaning methods.
The current research focuses on gathering all the new data from the beginning of the pandemic and summarizing novel information about the most effective ways to combat the spread of viral transmission (Fig. 1).
Main environmental factors in the transmission of the severe acute respiratory syndrome coronavirus (SARS-CoV-2) among the population: temperature, humidity, insects, air transmission (large droplets, tiny droplets, and droplet nuclei), infected surfaces, disinfection, and personal protective equipment (PPE)
Air transmission
The routes of virus transmission play a significant role in managing the outbreak. A virus can infect a person through direct contact with carriers, indirect contact via fomites, droplet transmission, and airborne transmission. Mainly, SARS-CoV-2 can be transmitted through three main routes: respiratory droplets, fomites, and aerosols. Coronaviruses can survive in aerosols. According to Aboubakr, the SARS-CoV-2 virus can be infectious in aerosols for 3 to 16 h. It has a diameter of 60–140 nm. Its form may be spherical, ellipsoid, or pleomorphic and belongs to the betacoronavirus category (Aboubakr et al. 2021).
One of the most important measures is social distancing. It has been suggested that people keep a minimum human-to-human distance of about 1, 5 to 2 m to minimize the risk of contagion. However, some studies support that the virus can be transmitted over 2 m from an infected individual. Social distancing and avoidance of overcrowded places play a significant role in decreasing virus transmission. People’s social habits should be adapted (Chen et al. 2021).
The primary way of getting infected is through droplets disseminated from the muco-salivary fluids as sneeze and cough. That highlights the need for facial masks use and other personal protective equipment. The diameter of droplets plays a significant role in airway transmission. According to the World Health Organization (WHO) and Centers for Disease Control and Prevention (CDC), droplets are higher than 5 μg in size, while desiccated droplets are lower than 5 µm in size (Correia et al. 2020; Jayaweera et al. 2020; Otter et al. 2016; Setti et al. 2020; Yang 2020).
Large droplets higher than 10 μg in size can be transferred from coughing and sneezing and fall to surfaces about 1–2 m from the infected person, while small particles lower than 5 µm that are blamed for airborne transmission may stay airborne for hours and can travel long distances (Correia et al. 2020; Jayaweera et al. 2020; Otter et al. 2016; Setti et al. 2020; Yang 2020).
Unfortunately, the ventilation systems commonly used daily-use standard filters with about higher than 1-micron pore diameter, which means that they are not effective against the virus. More efficient filters exist as high-efficiency particulate air (HEPA) is used in isolation rooms and intensive care units designed to meet specific requirements for managing infectious diseases. Airplane cabin ventilation systems also have HEPA filters. Indeed, in the past, ventilation systems transmitted contagious diseases such as measles, tuberculosis, chickenpox, influenza, smallpox, and SARS (Correia et al., 2020; Han et al., 2020a, b; Setti et al., 2020).
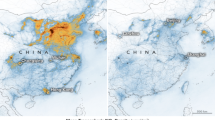
Nowadays, there is more knowledge about contagious diseases and prophylactic techniques that can be used to prevent their contamination. To date, due to overcrowded healthcare facilities, there is a higher possibility of pathogen-loaded droplets to be shed at hospitals and other healthcare units. Thus, as a result, the manifestation of the COVID-19 infection of an individual infected in a healthcare facility may be more severe due to the higher viral load. Undoubtedly, the stability of the SARS-CoV-2 virus in aerosol and surfaces is higher than that of SARS-CoV-1. According to a study, air pollution also seems to be related to increased risks of COVID-19 infection and mortality rates, especially in regions with poor air quality (Correia et al. 2020; Han et al. 2020a, b; Setti et al. 2020).
Temperature and humidity
In general, coronaviruses survive longer in lower temperatures and relative humidity environments. They have enveloped viruses, thus, more fragile, rendering them susceptible to heat. There is evidence that several cases of COVID-19 are related to cold and dry climates. It is of great significance to understand the effect of heat and relative humidity on the persistence of the virus (Aboubakr et al. 2021).
Heat causes the denaturation of the secondary structures of viral capsid proteins, while cold causes degradation in the nucleic acid (Laude, 1981; Lelie et al. 1987; Schlegel et al. 2001). According to Bhattacharjee, the prevalence of disease manifestation decreases as temperature increases (Bhattacharjee 2020; Eslami and Jalili 2020). The virus can survive at room temperature and relative humidity of 65% for a few days (Aboubakr et al. 2021).
A study examined the relationship between the annual average temperature compensation and confirmed cases. It concerned Brazil, which has a tropical climate, and the average temperature there varies from 16.8 °C to 27.4 °C. The study results indicated that temperature had a negative linear relationship with the number of confirmed cases. Thus, lower temperatures lead to the rise of COVID-19 instances and vice versa (Prata et al. 2020).
Another study reports that the half-life of the virus at room temperature of 24 °C ranges from 6.3 to 18.6 h, while when the temperature was increased to 35 °C, it was reduced to about 8.9 h. Relative humidity should not be neglected because it is closely correlated with temperature. The study concluded that the virus could persist from hours to days in indoor environments; thus, fomite transmission may be promoted (Biryukov et al. 2020).
According to Biryukov, at a temperature of 54.5 °C, the virus half-life ranged from 10.8 ± 3.0 min and the infectivity decreased about 90% at 35.4 ± 9.0 min, which means that in an environment which can reach so high temperatures such as the interior cabins of parked vehicles most commonly during the summer periods the infectivity decreased in a period about 40 min (Biryukov et al. 2021). Wang reports that the inactivation of the virus is achieved in 30 min at 56 °C and suggests the use of solar heating as a strategy of disinfection, especially in enclosed spaces, which seems to be very promising (Wang et al. 2020).
Transmission of SARS-CoV-2 by insect vectors
A study was conducted and tested the potential for house flies (Musca domestica) to acquire, harbor, and transmit SARS-CoV-2 mechanically. In general, flies can disseminate microbial agents from waste-contaminated breeding habitats to human foods, which subsequently can be ingested by human hosts. The flies need to acquire the virus from a contaminated surface and afterward harbor it on their gut or body surfaces to transmit it mechanically. The study results indicated that flies do not play a significant role in transmitting SARS-CoV-2 to humans and animals (Balaraman et al. 2021a, b).
Another study examined the susceptibility of midge and mosquito vectors to SARS-CoV-2. The insects which were used for the survey ingested a bloodmeal containing SARS-CoV-2. It was tested whether mosquitoes are susceptible to SARS-CoV-2 by an oral route of infection, which was not previously evaluated. The study concluded that insects do not play an essential role in transmitting SARS-CoV-2 to humans (Balaraman et al. 2021a, b).
Food, food handlers, food packages, water, wastewater, inanimate surfaces, and transmission of COVID-19 infection
To evaluate the risk of contracting the COVID-19 infection from contaminated environments, researchers focused on monitoring the presence of the SARS-CoV-2 virus in food, water, wastewater, bio-solid waste, and sludge (Carraturo et al. 2020). The virus is transmitted from contaminated cold food or food packaging material through person-to-thing-to-person transmission (Han and Liu 2021).
The SARS-CoV-2 virus remains highly stable under refrigeration, at 4 °C, and under freezing conditions, ranging from − 10 to − 80 °C, on different kinds of food such as fish, meat, and poultry and the skin of swine, during 14–21 days. However, there is a lack of data for the long-term survival of the virus. The contamination may happen in any step from the beginning to the end of the food chain. Indeed, nine cases were reported where SARS-CoV-2 was detected from the healthcare authorities on frozen food even from the beginning of the pandemic in early July and mid-August 2020 in China. Refrigerated and frozen food is favorable to become long-range carriers of SARS-CoV-2, posing a systematic risk for human health (Eslami and Jalili 2020).
To reduce the risk of COVID-19 transmission in the food chain, particular guidelines should be followed by meat and poultry processing workers and employers, which include wearing face coverings, proper hand hygiene, and complete personal hygiene such as covering the nose and mouth by bending the elbow during sneezing or coughing and social distancing. Smart food packaging, biosensors, and nanosensors for food safety may help in future for the quality check of food during all the steps of the cold chain, especially in the case of outbreaks (Eslami and Jalili 2020; Han et al. 2020a, b).
The inactivation rate of coronaviruses is usually higher in comparison with other viruses. The SARS-CoV-2 virus cannot survive at temperatures higher than 20 °C, and its presence in food cannot be detected for more than 72 h at a storage temperature of 4 °C. The survival of the SARS-CoV virus in biological specimens as feces, sputum, and serum is about 96 h. Still, it is less stable in urine, probably attributed to the presence of urea and different pH values. From the available data of April 2020, there were no cases reported of SARS-CoV or SARS-CoV-2 transmitted via sewages or sludge (Carraturo et al. 2020).
According to the WHO, the risk of transmission of the virus through the feces of an infected individual is very low. However, the infection with COVID-19 can be manifested with diarrhea at a range of 2–10% of cases. Indeed, there are no reports of transmission of the virus via the fecal–oral route. The virus can be present in the water although there is no evidence that it can be transmitted through contaminated water and has not been detected in drinking water supplies. In general, water safety should be reinsured with several measures to protect water sources, filtration, and disinfection. There is no proof that SARS-CoV-2 can be transmitted via sewerage systems with or without wastewater treatment. However, wastewater should be treated specially in well-designed infrastructures (Khan et al. 2021; UNICEF 2020).
The survival duration of viruses on different kinds of materials varies. Coronaviruses can survive in other porous and non-porous materials such as metals, plastics, woven and non-woven fabrics, paper, wood, glass, stethoscopes, eggs, feathers, and soft toys. The survival time depends on the properties of different surfaces as the type of surface, temperature, relative humidity, and the specific strain of the virus. SARS-CoV-2 can survive from the human body, short periods from 2 h to 9 days, in optimized in vitro conditions (Carraturo et al. 2020; Kampf et al. 2020).
According to Khan, the virus’s existence varies from 2 h to 5 days, and the temperatures range from 20 to 25 °C. SARS-CoV-2 can be found on metals for a maximum period of 5 days. Both SARS-CoV and SARS-CoV-2 can attach to aerosols for 3 h. The presence of the virus in stainless steel and plastic is about three days. The virus was not detected after 4 h on copper and 24 h in cardboard, respectively (Khan et al. 2021).
The study results indicated that a higher viral load of SARS-CoV-2 could survive for a longer time. That happens because of two main reasons: The virus needs a host organism and the second is that the COVID-19 virus is an enveloped virus with a fragile outer membrane. Generally, enveloped viruses are less stable and susceptible to oxidants, such as chlorine. The virus can become labile, being inactivated with low concentrations of disinfectants. According to a CDC review, the effective inactivation of the virus could be achieved within 1 min using common disinfectants, such as 70% ethanol or sodium hypochlorite (Carraturo et al. 2020; Casanova et al. 2010; CDC 2019; Kampf et al. 2020; Wang et al. 2005).
The capacity of SARS-CoV-2 to survive in materials used as personal protective equipment such as gowns, gloves, scrubs, and N95 respirators has been evaluated in several studies. Healthcare workers face emerging risks posed by coronaviruses as SARS-CoV-2. The main factors that affect the viability of the virus in vitro seem to be significant for transmitting the virus on hospital surfaces (Carraturo et al. 2020).
There is a correlation between the type, volume of respiratory secretion, and the suspending medium with the titer and volume of the virus. The temperature and relative humidity of places like hospital wards can be easily adjusted. Thus, the tests performed in vitro in extreme temperatures and humidity may not be related to reality (Carraturo et al. 2020; Lai et al. 2005; Otter et al. 2016; Sizun et al. 2000).
Hand, eye hygiene, personal protective equipment, and social distancing
It is well known that prevention is better than cure. Massive vaccination programs are in progress, although the role of hand hygiene, personal protective equipment, and social distancing for the protection of infectious diseases remains inevitable. Undoubtedly, personal protective equipment cannot protect the transmission of the SARS-CoV-2 virus fully, but it can minimize it at a significant level (Dai et al. 2021; Eslami and Jalili 2020).
From the beginning of the pandemic, the already existing variants are alpha, beta, and gamma (Akter et al. 2021). However, as with other RNA viruses, SARS-CoV-2 has high mutation rates, which leads to the appearance of new variants that are more transmissible as delta and omicron variants of the virus highlight the continuous need for the indoor use of masks (Meo et al. 2021).
In detail, the delta variant became the dominant strain in August 2021 and is inevitably more transmissible than the alpha variant due to the mutations found mainly in the spike proteins. Since November 2021, a novel variant is called the omicron variant, which has novel epidemiological and biological characteristics (Meo et al. 2021).
Nevertheless, this variant is more contagious than previous variants of SARS-CoV-2. Meanwhile, the first data showed that the people infected with the omicron variant present with milder infection and are mainly young and middle-aged (Meo et al. 2021; Shiehzadegan et al. 2021; Wang and Han 2022).
The surgical mask protects the respiratory tract from droplets, while N95 (FFP3) protects the respiratory tract from droplet nuclei. At the beginning of the pandemic, and in the absence of a suitable treatment against the virus, the proper hygiene of hands and the use of personal protective equipment constituted a significant measure of prophylaxis. The contact of body parts can lead to self-inoculation of mucous membranes such as eyes, nose, mouth, and ears; thus, without proper hygiene, the spread of the virus is promoted (Otter et al. 2016).
The recommendation of the WHO for hand hygiene suggests the use of an alcohol-based hand rub for 20–30 s using the appropriate technique in case of not visibly dirty hands, while, in case of visibly soiled hands, the use of soap and water for 40 − 60 s with the proper technique is suggested (Otter et al. 2016; UNICEF 2020; Yang 2020).
Gloves, gowns, and eye protection prevent the contact of the virus with mucous membranes and contamination of clothing or hands for subsequent nasal inoculation. The combination of personal protective equipment with hand disinfection reduces human-to-human transmission of the virus. The virus is transmitted through the air and from infected surfaces of individuals (Carraturo et al. 2020; Casanova et al. 2010; Mahmood et al. 2020).
Healthcare workers emphasize the importance of disinfection of hands and surfaces of both infected and healthy individuals, which minimizes self-contamination and protects against inoculation of mucosal surfaces. During an outbreak, the viral load of coronaviruses on inanimate surfaces is unknown. Thus, disinfection is suggested with bleach in a concentration of 0.1% for 1 min. Therefore, a dilution of 1:50 of the standard bleach is recommended. In the case of smaller surfaces, ethanol in the concentration of 70% is suggested (Carraturo et al. 2020; Casanova et al. 2010).
Particular attention should be paid to the risk of contamination of hands and clothing during personal protective equipment removal. Healthcare workers should take special courses to learn how to undress with the minimal risk of contamination. Protocols and guidelines should be used in healthcare facilities to ensure the best conditions for the patients and healthcare workers. However, individuals should not have the illusion that only hygiene measures can prevent the viral spread and visit overcrowded places, putting their health at significant risk (Australia 2020; Carraturo et al. 2020; Casanova et al. 2010; Chan et al. 2006; Eslami and Jalili 2020; Kampf et al. 2020; Medicine 2006; Otter et al. 2016; Sylwia Ufnalska and Eric Lichtfouse 2021a, b; Yang 2020).
When comparing indirect (contamination of inanimate surfaces) transmission with direct transmission, there is an uncertainty in the importance of indirect contact transmission compared to direct contact, droplet, and airborne routes. The extended use and reuse of personal protective equipment are not suggested. The survival capacity of the virus on personal protective equipment depends on the material. The reuse of personal protective equipment is only recommended when adequate supplies cannot be obtained (Australia 2020; Carraturo et al. 2020; Casanova et al. 2010; Chan et al. 2006; Eslami and Jalili 2020; Kampf et al. 2020; Medicine 2006; Otter et al. 2016; Sylwia Ufnalska and Eric Lichtfouse 2021a,b; Yang 2020).
Although many strategies have been applied to combat the spread of the virus, care should be given to the tending that we adapted from the beginning of the pandemic, to focus only on short-term methods to prevent further transmission and at the same time ignore the future results. For instance, possible allergies and skin irritation that may be caused by the daily use of disinfectants and masks should not be neglected (Australia 2020; Carraturo et al. 2020; Casanova et al. 2010; Chan et al. 2006; Eslami and Jalili 2020; Kampf et al. 2020; Medicine 2006; Otter et al. 2016; Sylwia Ufnalska and Eric Lichtfouse 2021a,b; Yang 2020).
Unfortunately, the probability of the appearance of novel pandemics is increased in future, and that is the main reason we urgently need effective strategies and measures. Humans should learn from the current pandemic to avoid crowded places, close-contact settings, and confined spaces. In the case of a new pandemic, measures should be taken earlier to prevent several deaths, especially those of people with comorbidities who are more vulnerable (Ufnalska and Lichtfouse, 2021a, b).
Conclusion
The environmental factors seem to play an essential role in spreading the infection with SARS-CoV-2. Although the knowledge and understanding of the virus evolved rapidly over the past few months, many things are still unknown. It is essential to understand the role of environmental factors such as temperature, humidity, food, water, sewage, air, insects, inanimate surfaces, and hand hygiene. Some of these factors can help combat the COVID-19 outbreak and future outbreaks.
It has been suggested that people should keep a distance of 2 m to minimize the risk of contagion due to airborne transmission of the virus. The knowledge that we have gained since the beginning of the pandemic indicates that social distancing is essential to combat the transmission of the virus. If not used properly, ventilation systems may promote viral spread.
However, ventilation systems that use special filters (HEPA) as isolation rooms and cabins of airplanes exist. Increased temperature and relative humidity constitute unfavorable conditions for the survival of the virus. The survival duration of the virus on different kinds of materials differs and depends on various factors. It can also be found in frozen food; thus, disinfection and hygiene are essential because they reduce coronavirus load on surfaces.
Therefore, the rate of transmission is decreased. The use of personal protective equipment for prevention should not be neglected. They still constitute one of the most critical ways to prevent infectious diseases, especially for the healthcare workers in close contact with infected patients. The massive use of masks in the population is inevitable, especially in indoor environments. There is no doubt that we learn from our mistakes. Continuous research and scientific collaboration in future will shed new light on our understanding of COVID-19 and improve the strategies and techniques of the management of pandemics.
According to CDC, the SARS-CoV-2 causes more infections and spreads faster because it is about two times more contagious than early forms. The enhanced transmissibility of the delta variant may be attributed to higher stability on different surfaces or within droplets in the air, increased maximal viral load, and a higher probability of infection. The increased maximal viral load is probably the main factor for increased contamination of the delta variant.
References
Aboubakr HA, Sharafeldin TA, Goyal SM (2021) Stability of SARS-CoV-2 and other coronaviruses in the environment and on common touch surfaces and the influence of climatic conditions: a review. Transbound Emerg Dis 68(2):296–312. https://doi.org/10.1111/tbed.13707
Akter S, Zakia MA, Mofijur M, Ahmed SF, Vo D-VN, Khandaker G, Mahlia TMI (2021) SARS-CoV-2 variants and environmental effects of lockdowns, masks and vaccination: a review. Environ Chem Lett. https://doi.org/10.1007/s10311-021-01323-7
Australia AWr (2020) SARS-CoV-2 - water and sanitation. 3p.
Balaraman V, Drolet BS, Gaudreault NN, Wilson WC, Owens J, Bold D, Swanson DA, Jasperson DC, Noronha LE, Richt JA, Mitzel DN (2021a) Susceptibility of midge and mosquito vectors to SARS-CoV-2. J Med Entomol 58(4):1948–1951. https://doi.org/10.1093/jme/tjab013
Balaraman V, Drolet BS, Mitzel DN, Wilson WC, Owens J, Gaudreault NN, Meekins DA, Bold D, Trujillo JD, Noronha LE, Richt JA (2021b) Mechanical transmission of SARS-CoV-2 by house flies. Parasit Vectors 14(1):214. https://doi.org/10.1186/s13071-021-04703-8
Bhattacharjee (2020) Statistical investigation of relationship between spread of coronavirus disease (COVID-19) and environmental factors based on study of four mostly affected places of China and five mostly affected places of Italy. arXiv preprint.
Biryukov J, Boydston JA, Dunning RA, Yeager JJ, Wood S, Reese AL, Ferris A, Miller D, Weaver W, Zeitouni NE, Phillips A (2020) Increasing temperature and relative humidity accelerates inactivation of SARS-CoV-2 on surfaces. mSphere. https://doi.org/10.1128/mSphere.00441-20
Biryukov J, Boydston JA, Dunning RA, Yeager JJ, Wood S, Ferris A, Miller D, Weaver W, Zeitouni NE, Freeburger D, Dabisch P (2021) SARS-CoV-2 is rapidly inactivated at high temperature. Environ Chem Lett. https://doi.org/10.1007/s10311-021-01187-x
Carraturo F, Del Giudice C, Morelli M, Cerullo V, Libralato G, Galdiero E, Guida M (2020) Persistence of SARS-CoV-2 in the environment and COVID-19 transmission risk from environmental matrices and surfaces. Environ Pollut 265(Pt B):115010. https://doi.org/10.1016/j.envpol.2020.115010
Casanova L, Rutala WA, Weber DJ, Sobsey MD (2010) Coronavirus survival on healthcare PPE. Infect Control Hosp Epidemiol 31(5):560–561. https://doi.org/10.1086/652452
CDC CoDaC (2019) Best practices for environmental cleaning in healthcare facilities: in resource-limited settings. Retrieved from Atlanta: (https://www.cdc.gov/hai/pdfs/resourcelimited/environmental-cleaning-508.pdf)
Chan PK, Tang JW, Hui DS (2006) SARS: clinical presentation, transmission, pathogenesis and treatment options. Clin Sci (lond) 110(2):193–204. https://doi.org/10.1042/CS20050188
Chen B, Jia P, Han J (2021) Role of indoor aerosols for COVID-19 viral transmission: a review. Environ Chem Lett 19(3):1953–1970. https://doi.org/10.1007/s10311-020-01174-8
Correia G, Rodrigues L, Gameiro da Silva M, Goncalves T (2020) Airborne route and bad use of ventilation systems as non-negligible factors in SARS-CoV-2 transmission. Med Hypotheses 141:109781. https://doi.org/10.1016/j.mehy.2020.109781
COVID-19 and vascular disease (2020) EBioMedicine, 58: 102966. doi:https://doi.org/10.1016/j.ebiom.2020.102966
Dai H, Han J, Lichtfouse E (2021) Smarter cures to combat COVID-19 and future pathogens: a review. Environ Chem Lett 19(4):2759–2771. https://doi.org/10.1007/s10311-021-01224-9
Eslami H, Jalili M (2020) The role of environmental factors to transmission of SARS-CoV-2 (COVID-19). AMB Express 10(1):92. https://doi.org/10.1186/s13568-020-01028-0
Han S, Liu X (2021) Can imported cold food cause COVID-19 recurrent outbreaks? A review. Environ Chem Lett. https://doi.org/10.1007/s10311-021-01312-w
Han C, Duan C, Zhang S, Spiegel B, Shi H, Wang W, Zhang L, Lin R, Liu J, Ding Z, Hou X (2020a) Digestive symptoms in COVID-19 patients with mild disease severity: clinical presentation, stool viral RNA testing, and outcomes. Am J Gastroenterol 115(6):916–923. https://doi.org/10.14309/ajg.0000000000000664
Han J, Zhang X, He S, Jia P (2020b) Can the coronavirus disease be transmitted from food? A review of evidence, risks, policies and knowledge gaps. Environ Chem Lett. https://doi.org/10.1007/s10311-020-01101-x
Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, Zhang L, Fan G, Xu J, Gu X, Cheng Z (2020) Clinical features of patients infected with 2019 novel coronavirus in Wuhan. China Lancet 395(10223):497–506. https://doi.org/10.1016/S0140-6736(20)30183-5
Jayaweera M, Perera H, Gunawardana B, Manatunge J (2020) Transmission of COVID-19 virus by droplets and aerosols: A critical review on the unresolved dichotomy. Environ Res 188:109819. https://doi.org/10.1016/j.envres.2020.109819
Kampf G, Todt D, Pfaender S, Steinmann E (2020) Persistence of coronaviruses on inanimate surfaces and their inactivation with biocidal agents. J Hosp Infect 104(3):246–251. https://doi.org/10.1016/j.jhin.2020.01.022
Khan AH, Tirth V, Fawzy M, Mahmoud AED, Khan NA, Ahmed S, Ali SS, Akram M, Hameed L, Islam S, Das G (2021) COVID-19 transmission, vulnerability, persistence and nanotherapy: a review. Environ Chem Lett. https://doi.org/10.1007/s10311-021-01229-4
Lai MY, Cheng PK, Lim WW (2005) Survival of severe acute respiratory syndrome coronavirus. Clin Infect Dis 41(7):e67-71. https://doi.org/10.1086/433186
Laude H (1981) Thermal inactivation studies of a coronavirus, transmissible gastroenteritis virus. J Gen Virol 56(Pt 2):235–240. https://doi.org/10.1099/0022-1317-56-2-235
Lelie PN, Reesink HW, Lucas CJ (1987) Inactivation of 12 viruses by heating steps applied during manufacture of a hepatitis B vaccine. J Med Virol 23(3):297–301. https://doi.org/10.1002/jmv.1890230313
Leung NHL (2021) Transmissibility and transmission of respiratory viruses. Nat Rev Microbiol 19(8):528–545. https://doi.org/10.1038/s41579-021-00535-6
Mahmood SU, Crimbly F, Khan S, Choudry E, Mehwish S (2020) Strategies for rational use of PPE (PPE) among healthcare providers during the COVID-19 crisis. Cureus 12(5):e8248. https://doi.org/10.7759/cureus.8248
Mathur MB, Patel RB, Gould M, Uyeki TM, Bhattacharya J, Xiao Y, Gillaspie Y, Chae C, Khazeni N (2014) Seasonal patterns in human A (H5N1) virus infection: analysis of global cases. PLoS ONE 9(9):e106171. https://doi.org/10.1371/journal.pone.0106171
Medicine IO (2006) Reusability of facemasks during an influenza pandemic: facing the flu. The National Academies Press, Washington, DC
Meo SA, Meo AS, Al-Jassir FF, Klonoff DC (2021) Omicron SARS-CoV-2 new variant: global prevalence and biological and clinical characteristics. Eur Rev Med Pharmacol Sci 25(24):8012–8018. https://doi.org/10.26355/eurrev_202112_27652
Otter JA, Donskey C, Yezli S, Douthwaite S, Goldenberg SD, Weber DJ (2016) Transmission of SARS and MERS coronaviruses and influenza virus in healthcare settings: the possible role of dry surface contamination. J Hosp Infect 92(3):235–250. https://doi.org/10.1016/j.jhin.2015.08.027
Prata DN, Rodrigues W, Bermejo PH (2020) Temperature significantly changes COVID-19 transmission in (sub)tropical cities of Brazil. Sci Total Environ 729:138862. https://doi.org/10.1016/j.scitotenv.2020.138862
Schlegel A, Immelmann A, Kempf C (2001) Virus inactivation of plasma-derived proteins by pasteurization in the presence of guanidine hydrochloride. Transfusion 41(3):382–389. https://doi.org/10.1046/j.1537-2995.2001.41030382.x
Setti L, Passarini F, De Gennaro G, Barbieri P, Perrone MG, Borelli M, Palmisani J, Di Gilio A, Piscitelli P, Miani A (2020) Airborne transmission route of COVID-19: why 2 Meters/6 feet of inter-personal distance could not be enough. Int J Environ Res Public Health. https://doi.org/10.3390/ijerph17082932
Shiehzadegan S, Alaghemand N, Fox M, Venketaraman V (2021) Analysis of the Delta Variant B.1.617.2 COVID-19. Clin Pract 11(4):778–784. https://doi.org/10.3390/clinpract11040093
Siddiqi HK, Libby P, Ridker PM (2021) COVID-19 – a vascular disease. Trends Cardiovasc Med 31(1):1–5. https://doi.org/10.1016/j.tcm.2020.10.005
Sizun J, Yu MW, Talbot PJ (2000) Survival of human coronaviruses 229E and OC43 in suspension and after drying onsurfaces: a possible source of hospital-acquired infections. J Hosp Infect 46(1):55–60. https://doi.org/10.1053/jhin.2000.0795
Ufnalska S, Lichtfouse E (2021a) Unanswered issues related to the COVID-19 pandemic. Environ Chem Lett. https://doi.org/10.1007/s10311-021-01249-0
Ufnalska S, Lichtfouse E (2021b) Unanswered issues related to the COVID-19 pandemic. Environ Chem Lett 19(5):3523–3524. https://doi.org/10.1007/s10311-021-01249-0
UNICEF W (2020) Water, sanitation, hygiene and waste management for COVID-19: technical brief. from World Health Organization https://apps.who.int/iris/handle/10665/331305
Vaira LA, Salzano G, Deiana G, De Riu G (2020) Anosmia and ageusia: common findings in COVID-19 patients. Laryngoscope 130(7):1787. https://doi.org/10.1002/lary.28692
Wang C, Han J (2022) Will the COVID-19 pandemic end with the delta and omicron variants? Environ Chem Lett. https://doi.org/10.1007/s10311-021-01369-7
Wang XW, Li JS, Jin M, Zhen B, Kong QX, Song N, Xiao WJ, Yin J, Wei W, Wang GJ, Si BY, Li JW (2005) Study on the resistance of severe acute respiratory syndrome-associated coronavirus. J Virol Methods 126(1–2):171–177. https://doi.org/10.1016/j.jviromet.2005.02.005
Wang X, Sun S, Zhang B, Han J (2020) Solar heating to inactivate thermal-sensitive pathogenic microorganisms in vehicles: application to COVID-19. Environ Chem Lett. https://doi.org/10.1007/s10311-020-01132-4
Yang C (2020) Does hand hygiene reduce SARS-CoV-2 transmission? Graefes Arch Clin Exp Ophthalmol 258(5):1133–1134. https://doi.org/10.1007/s00417-020-04652-5
Acknowledgements
This research in Robert Penchovsky’s Laboratory is supported by a Grant KP-06-H31/18/13.12.2019 Awarded by the Bulgarian National Science Fund (BNSF).
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Valsamatzi-Panagiotou, A., Penchovsky, R. Environmental factors influencing the transmission of the coronavirus 2019: a review. Environ Chem Lett 20, 1603–1610 (2022). https://doi.org/10.1007/s10311-022-01418-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10311-022-01418-9