This study tracked a radiology department’s conversion from utilization of a Kodak Amber analog system to a Kodak DirectView DR 5100 digital system. Through the use of ProModel® Optimization Suite, a workflow simulation software package, significant quantitative information was derived from workflow process data measured before and after the change to a digital system. Once the digital room was fully operational and the radiology staff comfortable with the new system, average patient examination time was reduced from 9.24 to 5.28 min, indicating that a higher patient throughput could be achieved. Compared to the analog system, chest examination time for modality specific activities was reduced by 43%. The percentage of repeat examinations experienced with the digital system also decreased to 8% vs. the level of 9.5% experienced with the analog system. The study indicated that it is possible to quantitatively study clinical workflow and productivity by using commercially available software.
Similar content being viewed by others
Introduction
Radiology departments have had to adapt to a changing and shrinking workforce over the last decade. Measuring and improving productivity by studying a department’s workflow has become critical to optimizing a department’s operations.1–7 Although film/screen productivity has been quite well documented8,9, the digital radiology (DR) environment has not, especially for those departments transitioning to a non-PACS (picture archiving and communication system) setting.10–16 It has become important to departments to understand their workflow and to measure, quantify, and optimize their productivity.2,17–20
Christie Hospital NHS Trust, located in Manchester, England, was studied during its transition from an analog operation to a digital (non-PACs) one. Christie Hospital is a specialty center committed to providing the best treatment care for patients with cancer. There are four general projection radiology rooms, staffed by seven consultant radiologists and three specialist registrars. The radiology department was completely analog until late 2003, at which time a Kodak DirectView DR 5100 System replaced the Kodak Amber Imaging System, which was a dedicated chest analog unit. This study reports on the benefits gained by this department by comparing chest examination analog operations vs. results obtained from its digital operations.
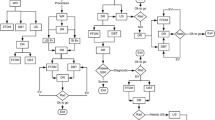
Understanding a radiology department’s workflow is usually conducted in a brute-force fashion; that is, by taking a stopwatch and physically timing each step of the clinical examination process. This process can be viewed as taking a snapshot of the radiologic technologist’s daily activities revolving around a patient examination including the room preparation prior to an examination, the examination itself, and the discharge of the patient from the radiology department. After careful observation of radiology departments at three sites in the United States and four sites in Europe, process flow maps for analog and DR workflows were generated. Workflows across the sites were found to be quite consistent.
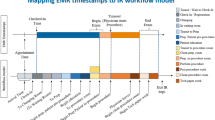
Activities can be classified as either modality- or nonmodality-specific. Modality-specific activities are those that can be directly impacted by the imaging modality that is selected. Examples of modality-specific activities include picking up cassettes (analog), placing patient ID information on a film (analog), or accepting a screen image before proceeding with an examination (digital). Nonmodality-specific activities include those that occur regardless of the imaging modality in use. Examples of nonmodality-specific activities include escorting a patient from the waiting area, waiting while the patient changes into a gown, and discharging the patient from the department.
Obviously, activity time can be impacted by various patient demographics including patient age and mobility, as well as examination type, and number of images required per examination. To reduce the variability inherent in the examination process, the general type of radiology examinations were tracked for chest examinations of ambulatory patients only. Other examination types, such as examinations involving wheelchair or bedridden patients, were not documented.
Materials and Methods
As part of a larger study conducted in 2003, standard work around site process and data gathering activities were developed. In June 2003, a team from Eastman Kodak Company’s Health Group, Digital Capture SPG, went to Christie Hospital as part of a study to look at radiology department workflows. The Christie operation was a 100% analog operation at that time. Most chest examinations were performed with the use of an aged Kodak Amber analog system. Detailed quantitative and qualitative information about the site and its operations was gathered during the team’s visit.
A Kodak directView DR 5100 unit (Fig. 1) was installed at the Christie Hospital during the fourth quarter of 2003. In July 2004, a second team returned to Christie to study the utilization of the DR 5100 unit. In addition to the quantitative activity information (Table 1), qualitative information was again gathered. The quantitative data were statistically evaluated.
Previously, the standard analog and DR workflows established from observations at multiple sites were used to create a modality-specific process flow model utilizing ProModel® Optimization Suite, a modeling software used for process simulation. ProModel® Optimization Suite can be used to assist in the analysis of evaluating, planning, or designing operational and strategic processes or process improvements. The software can accommodate up to 20 different statistical distribution types for modeling with great flexibility. The authors are not aware of any other study where workflow data were analyzed using modeling software.
Nonmodality-specific activities were not included in the model because major changes in procedures, site layout, or personnel could have a significant impact across sites as well as within a site. At Christie, it should be noted that no changes were observed in these areas between the two site visits. Data acquired during the two site visits were used to develop the comparison of average patient examination times, percent repeat data, and room utilization data.
Results
Statistical analysis of the data utilizing ProModel® Optimization Suite to model the modality-specific workflow indicated that the Christie Hospital chest examination workflow with the DR 5100 took 43% less time (on average) than the chest examination workflow utilizing the Amber analog system. The typical average patient time (modality-specific activities) for the DR 5100 was about 5 min compared to about 9 min for the analog process. Comparing percent room utilization, analog was approximately 66%, whereas digital was on the order of 38%, or in other words, utilization of the DR 5100 resulted in the chest room being available almost twice as much with the digital system as with the analog system. This implied that patient throughput could be increased—a fact supported by the anecdotal perception of the Christie technologists as reported in their answers to a qualitative questionnaire.
Also, in addition to the improvements in patient throughput, the examination repeat rate was reduced with the DR 5100 process to 8.0% from the 9.5% level that was experienced with the Amber unit.
Discussion
Initial workflow data were gathered across seven sites in May through June of 2003, according to a standard process developed during that timeframe. Despite common workflows across sites, there was a large amount of variability in the cross-site data that were gathered. It is believed that several factors contributed to the data variability, including varying utilization of standard operating procedures (SOPs), different site layouts, and radiologic technologist pace (impacted by age and experience). To minimize variability, it was decided that a before-and-after study needed to be executed on one single site. Christie Hospital was gracious enough to participate and allow our study team to visit during clinical hours.
By study design, no technologist-specific data were collected owing to concerns expressed by site management and the technologists. Hence, technologist variability was considered a noise factor in the data. At Christie, between the initial analog study and the follow-up digital study, there was neither technologist turnover nor observed changes in standard operating procedures and processes.
Patient variability was also present in this study, but differences in patient demographics at Christie were minimal. For both the 2003 and 2004 data, only data from ambulatory patients were included. Age was not a discriminatory factor, with the predominant age group being adult or aged. Additionally, by only looking at modality-specific activities in the simulation model, some of the activities that would be significantly impacted by age, for example, speed of changing clothes, speed of walking to the room, or speed of discharge, were excluded. Between the two studies, there was no observable shift in patient demographics. By focusing on chest exams, the potential for large variability associated with different types of exams, number of images per examination, and positioning and technique differences were eliminated.
Data collector information was collected as well. There were some significant differences between data collectors, in some cases, despite training and on-site data reviews. In 2003, there were four data collectors. Generally, three of the four collectors did not display statistical differences in their data. In those cases where significant differences were detected, data from the fourth data collector was removed. In 2004, there were only two data collectors. Although there were some statistical differences in some of the activities, the differences were not as great as in 2003, and no data were deleted based on data collector.
ProModel® Optimization Suite
ProModel® Optimization Suite from ProModel Corporation (www.ProModel.com) is a workflow simulation package. Activities in a workflow or process are used to create a model. Means, standard deviations, and distributions are loaded for each activity. The software executes a Monte Carlo run for a prescribed number of patients by utilizing the loaded data. The standard used for this study was 30 patients per day, 20 days, for a total throughput of 600 patients per run and approximately 1,300 images.
Normal distributions were assumed for the times associated with each workflow activity, with means and standard deviations equal to their sample estimates. For each activity in the 2003 data, several distributions were fitted and evaluated for lack of fit. Generally, normal distributions provided the best fit. Table 2 illustrates the data from both the analog and digital analysis.
Analysis of Average Run Times
It is statistically interesting to note that noneof the individual activities were significantlydifferent (except for the repeat rate) as a result of the large variability present. It is important to remember that the analog workflow had additional activities such as “pick up cassettes” and “id film” that the digital flow did not have. Conversely, the digital flow had an additional activity of “quality check on printed film” that the analog flow did not have because Christie printed 100% of its images. Given the different examination repeat rates, these differences had a significant impact on the average time. It bears repeating that the average patient examination times reported below pertain only to those modality-specific activities contained in the models—actual patient examination times would generally be longer because they would contain activities such as escorting the patient, changing, walking to and from the examination room, and waiting.
Ninety-five percent confidence intervals (CI) were determined for the mean and standard deviations of each activity (Table 3). Runs were made at the mean levels and at the high and low levels (axial points) of the CIs for the mean and the standard deviation. In doing so, the intent was to capture the variability existing in the individual activities at the extreme possibilities of performance. An evaluation of the extremes allowed a statement to be made regarding the differential significance between the overall analog and digital processes when the modality specific activities were combined into the total workflow.
A plot of the data confirmed that even at the extreme points, there were no overlap of the data generated from the axial points, as shown in Figures 2 and 3. This provided confidence that there was a difference in the average patient examination times between the analog and digital modality-specific workflows, given the simulation conditions and individual activity data discussed above. On average, the typical average patient time for modality-specific activities for the DR 5100 was 5.28 vs. 9.24 min for the analog process, which is a 43% reduction in time as a result of using the digital system. Comparing percent room utilization, the analog room was utilized 65.9% of the time in order to see all of the patients, whereas when using the digital system, the same number of patients resulted in the room being utilized only 37.9% of the time. The lower room utilization for a fixed number of patients implies that a higher patient throughput can be achieved with the digital system.
Conclusions
It was possible to model radiological workflow and, hence, productivity with a commercially available software package. ProModel® Optimization Suite, using several statistical probability functions, was successfully used in understanding the clinical transitional process from analog to digital. Workflow productivity at Christie Hospital was shown to increase as a result of a decrease in the time required for an examination; from 9.24 min for an analog examination down to 5.28 min for a digital examination. For a fixed number of patients, room utilization decreased from 65.9% in the analog case to 37.9% in the digital environment. Further productivity and workflow studies are required to further refine the modeling concept.
References
BI Reiner EL Siegel JA Carrino (2002) ArticleTitleSCAR Radiologic Technologist Survey: analysis of the impact of digital technologies on productivity J Digit Imaging 15 IssueID3 132–140 Occurrence Handle12481227 Occurrence Handle10.1007/s10278-002-0021-8
BI Reiner EL Siegel JA Carrino (2002) ArticleTitleSCAR Radiologic Technologist Survey: analysis of technologist workforce and staffing J Digit Imaging 15 IssueID3 121–131 Occurrence Handle12481226 Occurrence Handle10.1007/s10278-002-0020-9
BI Reiner EL Siegel (2002) ArticleTitleChanges in technologist productivity with implementation of an enterprise-wide PACS J Digit Imaging 15 22–26 Occurrence Handle12134211 Occurrence Handle10.1007/s10278-002-0999-y
BI Reiner EL Siegel FJ Hooper et al. (1998) ArticleTitleEffect of film-based versus filmless operation on the productivity of CT technologists Radiology 207 481–485 Occurrence Handle9577498 Occurrence Handle1:STN:280:DyaK1c3jvVemuw%3D%3D
BI Reiner EL Siegel (2002) ArticleTitleTechnologist productivity in the performance of general radiographic examinations: Comparison of film-based versus filmless operations AJR 179 33–37 Occurrence Handle12076899
BI Reiner EL Siegel (1999) NoChapterTitle EL Siegel RM Kolodner (Eds) PACS and productivity Springer-Verlag New York, NY 103–112
BI Reiner EL Siegel K Siddiqui (2003) ArticleTitleEvolution of the digital revolution: a radiologist perspective J Digit Imaging 16 IssueID4 324–330 Occurrence Handle14747936 Occurrence Handle10.1007/s10278-003-1743-y
DW MacEwan (1982) ArticleTitleRadiology workload system for diagnostic radiology: productivity environment studies J Can Assoc Radiol 33 182–196
KP Andriole (2002) ArticleTitleProductivity and cost assessment of computed radiography, digital radiography, and screen-film for outpatient chest examinations J Digit Imaging 15 IssueID3 161–169 Occurrence Handle12532253 Occurrence Handle10.1007/s10278-002-0026-3
ML Janower (1988) ArticleTitleProductivity standards for technologists: how to use them Radiology 166 276–277 Occurrence Handle3336694 Occurrence Handle1:STN:280:DyaL1c%2FpvVWhsQ%3D%3D
LL Hanwell JM Conway (1996) Utilization of Imaging Staff: Measuring Productivity American Healthcare Radiology Administrators Sudbury, MA 1–30
EL Wiegel JN Diaconis S Pomerantz et al. (1995) ArticleTitleMaking filmless radiology work J Digit Imaging 8 151–155 Occurrence Handle10.1007/BF03168713
WM Tellis KP Andriole CS Jovais DE Avrin (2002) ArticleTitleRIS minus PACS equals film J Digit Imaging 15 IssueIDSuppl 1 20–26 Occurrence Handle12105693 Occurrence Handle10.1007/s10278-002-5037-6
KP Andriole DM Luth RG Gould (2002) ArticleTitleWorkflow assessment of digital versus computed radiography and screen-film in the outpatient environment J Digit Imaging 5 IssueIDSuppl 1 124–126 Occurrence Handle10.1007/s10278-002-5079-9
Andriole KP, Luth DM, Gould RG: Workflow comparison of DR and Screen-film dedicated chest systems. SPIE, Medical Imaging 2001: Physics of Medical Imaging, San Diego, February 17–22, 2001
GA May DD Deer D Dackiewicz (2000) ArticleTitleImpact of digital radiography on clinical workflow J Digit Imaging 13 IssueIDSuppl 1 76–78 Occurrence Handle10847368 Occurrence Handle1:STN:280:DC%2BD3cvotVOksQ%3D%3D Occurrence Handle10.1007/BF03167630
BI Reiner EL Siegel JA Carrino (2002) ArticleTitleWorkflow optimization: current trends and future directions J Digit Imaging 15 141–152 Occurrence Handle12481228 Occurrence Handle10.1007/s10278-002-0022-7
RM Barnes (1966) Motion and Time Study: Design and Measurement of Work Wiley New York, NY
EL Siegel BI Reiner (2002) NoChapterTitle K Dreyer (Eds) Image Workflow Springer Verlag New York, NY 161–190
BI Reiner EL Siegel (2002) ArticleTitleTechnologists’ productivity when using PACS: comparison of film-based versus filmless radiography AJR 179 33–37 Occurrence Handle12076899
Acknowledgments
Kodak would like to acknowledge the assistance given to the Kodak team by Fran Maders and the Radiographers at the Christie Hospital. Their time, effort, and continuous support of this study are greatly appreciated.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License ( https://creativecommons.org/licenses/by-nc/2.0 ), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Wideman, C., Gallet, J. Analog to Digital Workflow Improvement: A Quantitative Study. J Digit Imaging 19 (Suppl 1), 29–34 (2006). https://doi.org/10.1007/s10278-006-0770-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10278-006-0770-x