Abstract
Background
Research has shown that a small proportion of patients account for the majority of health care spending. The objective of this analysis was to determine the amount and proportion of preventable acute care spending among high-cost patients.
Methods
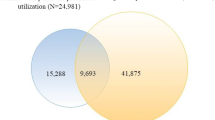
We examined a population-based sample of all adult high-cost patients using linked administrative health care data housed at ICES in Toronto, Ontario. High-cost patients were defined as those in and above the 90th percentile of the cost distribution. Preventable acute care (emergency department visits and hospitalisations) was defined using validated algorithms. We estimated costs of preventable and non-preventable acute care for high- and non-high-cost patients by category of visit/condition. We replicated our analysis for persistent high-cost patients and high-cost patients under 65 years and those 65 years and older.
Results
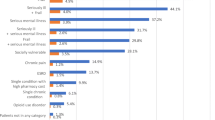
We found that 10% of all acute care spending among high-cost patients was considered preventable; this figure was higher for non-high-cost patients (25%). The proportion of preventable acute care spending was higher for persistent high-cost patients (14%) and those 65 years and older (12%). Among ED visits, the largest portion of preventable care spending was for primary care treatable conditions; for hospitalisations, the highest proportions of preventable care spending were for COPD, bacterial pneumonia and urinary tract infections.
Conclusions
Although high-cost patients account for a substantial proportion of health care costs, there seems to be limited scope to prevent acute care spending among this patient population. Nonetheless, care coordination and improved access to primary care, and disease prevention may prevent some acute care.
Similar content being viewed by others
References
Riley, G.F.: Long-term trends in the concentration of Medicare spending. Health Aff. (Millwood) 26(3), 808–816 (2007)
de Oliveira, C., Cheng, J., Vigod, S., Rehm, J., Kurdyak, P.: Patients with high mental health costs incur over 30 percent more costs than other high cost patients. Health Aff. (Millwood) 35(1), 36–43 (2016)
Smulowitz, P.B., Lipton, R., Wharam, J.F., et al.: Emergency department utilization after the implementation of Massachusetts health reform. Ann. Emerg. Med. 58(3), 225–234 (2011)
Ballard, D.W., Price, M., Fung, V., et al.: Validation of an algorithm for categorizing the severity of hospital emergency department visits. Med. Care 48(1), 58–63 (2010)
Niefeld, M.R., Braunstein, J.B., Wu, A.W., Saudek, C.D., Weller, W.E., Anderson, G.F.: Preventable hospitalization among elderly Medicare beneficiaries with type 2 diabetes. Diabetes Care 26(5), 1344–1349 (2003)
Billings, J., Anderson, G.M., Newman, L.S.: Recent findings on preventable hospitalizations. Health Aff. (Millwood) 15(3), 239–249 (1996)
Oster, A., Bindman, A.B.: Emergency department visits for ambulatory care sensitive conditions: insights into preventable hospitalizations. Med. Care 41(2), 198–207 (2003)
Braunstein, J.B., Anderson, G.F., Gerstenblith, G., et al.: Noncardiac comorbidity increases preventable hospitalizations and mortality among Medicare beneficiaries with chronic heart failure. J. Am. Coll. Cardiol. 42(7), 1226–1233 (2003)
Joynt, K.E., Gawande, A.A., Orav, E.J., Jha, A.K.: Contribution of preventable acute care spending to total spending for high-cost Medicare patients. JAMA 309(24), 2572–2578 (2013)
Graven, P.F., Meath, T.H.A., Mendelson, A., Chan, B.K.S., Dorr, D.A., McConnell, K.J.: Preventable acute care spending for high-cost patients across payer types. J. Health Care Financ. 42(3), 1–22 (2016)
Ronksley, P.E., Kobewka, D.M., McKay, J.A., et al.: Clinical characteristics and preventable acute care spending among a high cost inpatient population. BMC Health Serv. Res. 16, 165 (2016)
Wodchis, W.P., Bushmeneva. K., Nikitovic, M., McKillop, I.: Guidelines on person-level costing using administrative databases in Ontario [Internet]. Health System Performance Research Network, Toronto. (Working paper vol. 1). http://www.hsprn.ca/uploads/files/Guidelines_on_PersonLevel_Costing_May_2013.pdf (2013). Accessed 10 Nov 2015
Wodchis, W.P., Austin, P.C., Henry, D.A.: A 3-year study of high-cost users of health care. CMAJ 188, 182–188 (2016)
Wagner, N.Y.U.:. NYU ED algorithm: background. https://wagner.nyu.edu/faculty/billings/nyued-background (2000). Accessed 09 Aug 2017
Wharam, J.F., Landon, B.E., Galbraith, A.A., Kleinman, K.P., Soumerai, S.B., Ross-Degnan, D.: Emergency department use and subsequent hospitalizations among members of a high-deductible health plan. JAMA 297(10), 1093–1102 (2007)
Johnston, K.J., Allen, L., Melanson, T.A., Pitts, S.R.: A “Patch” to the NYU emergency department visit algorithm. Health Serv. Res. 52(4), 1264–1276 (2017)
Billings, J., Parikh, N., Mijanovich, T.: Emergency department use: the New York Story. Issue Brief (Commonw Fund) 434, 1–12 (2000)
Lowe, R.A.: Updating the emergency department algorithm: one patch is not enough. Health Serv. Res. 52(4), 1257–1263 (2017)
Basu, J., Friedman, B., Burstin, H.: Primary care, HMO enrollment, and hospitalization for ambulatory care sensitive conditions: a new approach. Med. Care 40(12), 1260–1269 (2002)
Bindman, A.B., Grumbach, K., Osmond, D., et al.: Preventable hospitalizations and access to health care. JAMA 274(4), 305–311 (1995)
Jiang, H.J., Russo, C.A., Barrett, M.L.: Nationwide frequency and costs of potentially preventable hospitalizations. Agency for Healthcare Research & Quality, Rockville (2006). (HCUP Statistical Brief 72)
Agency for Healthcare Research and Quality. Prevention quality indicators overview. http://www.qualityindicators.ahrq.gov/modules/pqi_overview.aspx (2011). Accessed 10 Aug 2017
Antoniou, T., Zagorski, B., Loutfy, M.R., et al.: Validation of case-finding algorithms derived from administrative data for identifying adults living with human immunodeficiency virus infection. PLoS One 6(6), e21748 (2011)
Benchimol, E., Guttmann, A., Mack, D.R., et al.: Validation of international algorithms to identify adults with inflammatory bowel disease in health administrative data from Ontario, Canada. J. Clin. Epidemiol. 67(8), 887–896 (2014)
Gershon, A.S., Wang, C., Guan, J., et al.: Identifying patients with physician diagnosed asthma in health administrative databases. Can. Respir. J. 16(6), 183–188 (2009)
Gershon, A.S., Wang, C., Guan, J., et al.: Identifying individuals with physician diagnosed COPD in health administrative databases. COPD 6(5), 388–394 (2009)
Hux, J.E., Ivis, F., Flintoft, V., et al.: Diabetes in Ontario: determination of prevalence and incidence using a validated administrative data algorithm. Diabetes Care 25(3), 512–516 (2002)
Jaakkimainen, R.L., Bronskill, S.E., Tu, K., et al.: Identification of physician-diagnosed Alzheimer’s disease and related dementias in population-based administrative data: a validation study using family physicians’ electronic medical records. J. Alzheimer’s Dis. 54(1), 337–349 (2016)
Paul, Kurdyak, Elizabeth, Lin, Diane, Green, Simone, Vigod: Validation of a population-based algorithm to detect chronic psychotic illness. Can. J. Psychiatry 60(8), 362–368 (2015)
Moist, L.M., Fenton, S., Kim, J.S., et al.: Canadian Organ Replacement Register (CORR): reflecting the past and embracing the future. Can. J. Kidney Health Dis. 1, 26 (2014)
Prodhan, S., King, M.J., De, P., Gilbert, J.: Health services data: the Ontario Cancer Registry (a unique, linked, and automated population-based registry). In: Sobolev, B., Levy, A., Goring, S. (eds.) Data and Measures in Health Services Research. Springer, Boston (2016)
Schultz, S.E., Rothwell, D.M., Chen, Z., et al.: Identifying cases of congestive heart failure from administrative data: a validation study using primary care patient records. Chronic Dis. Inj. Can. 33(3), 160–166 (2013)
Tu, K., Chen, Z., Lipscombe, L.L., Canadian Hypertension Education Program Outcomes Research Taskforce: Prevalence and incidence of hypertension from 1995 to 2005: a population-based study. CMAJ 178(11), 1429–1435 (2008)
Widdifield, J., Bernatsky, S., Paterson, J.M., Tu, K., Ng, R., Thorne, J.C., et al.: Accuracy of Canadian Health administrative databases in identifying patients with rheumatoid arthritis: a validation study using the medical records of rheumatologists. Arthritis Care Res. (Hoboken) 65(10), 1582–1589 (2013)
The Johns Hopkins University Bloomberg School of Public Health. The Johns Hopkins ACG Case-Mix System Version 7.0 Release Notes (Systems Documentation). In: Weiner, J.P. (ed.) Johns Hopkins University, Baltimore (2005)
The consumer price index. Statistics Canada, Ottawa (ON) (2016). Cat. no. 62-001-X
Capp, R., Misky, G.J., Lindrooth, R.C., Honigman, B., Logan, H., Hardy, R., Nguyen, D.Q., Wiler, J.L.: Coordination program reduced acute care use and increased primary care visits among frequent emergency care users. Health Aff. (Millwood) 36(10), 1705–1711 (2017)
Blustein, J., Hanson, K., Shea, S.: Preventable hospitalizations and socioeconomic status. Health Aff. (Millwood) 17(2), 177–189 (1998)
Medford-Davis, L.N., Shah, R., Kennedy, D., Becker, E.: The role of mental health disease in potentially preventable hospitalizations: findings from a large state. Med. Care 56(1), 31–38 (2018)
Hensel, J.M., Taylor, V.H., Fung, K., Yang, R., Vigod, S.N.: Acute care use for ambulatory care-sensitive conditions in high-cost users of medical care with mental illness and addictions. Can. J. Psychiatry 63, 816 (2018)
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
This study was conducted with the support of Cancer Care Ontario through funding provided by the Government of Ontario. Parts of this material are based on data and information provided by Cancer Care Ontario (CCO). The opinions, results, view, and conclusions reported in this paper are those of the authors and do not necessarily reflect those of CCO. No endorsement by CCO is intended or should be inferred. This study was supported by ICES, which is funded by an annual grant from the Ontario Ministry of Health and Long-Term Care (MOHLTC). The opinions, results, and conclusions reported in this article are those of the authors and are independent from the funding sources. No endorsement by ICES or the Ontario MOHLTC is intended or should be inferred. Parts of this material are based on data and/or information compiled and provided by the Canadian Institute for Health Information (CIHI). However, the analyses, conclusions, opinions and statements expressed in the material are those of the author(s), and not necessarily those of CIHI.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
de Oliveira, C., Cheng, J. & Kurdyak, P. Determining preventable acute care spending among high-cost patients in a single-payer public health care system. Eur J Health Econ 20, 869–878 (2019). https://doi.org/10.1007/s10198-019-01051-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10198-019-01051-4