Abstract
Objective
To develop a model to predict annual hospital costs for patients with established renal failure, taking into account the effect of patient and treatment characteristics of potential relevance for conducting an economic evaluation, such as age, comorbidities and time on treatment. The analysis focuses on factors leading to variations in inpatient and outpatient costs and excludes fixed costs associated with dialysis, transplant surgery and high cost drugs.
Methods
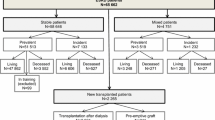
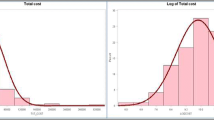
Annual costs of inpatient and outpatient hospital episodes for patients starting renal replacement therapy in England were obtained from a large retrospective dataset. Multiple imputation was performed to estimate missing costs due to administrative censoring. Two-part models were developed using logistic regression to first predict the probability of incurring any hospital costs before fitting generalised linear models to estimate the level of cost in patients with positive costs. Separate models were developed to predict inpatient and outpatient costs for each treatment modality.
Results
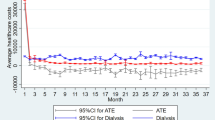
Data on hospital costs were available for 15,869 incident dialysis patients and 4511 incident transplant patients. The two-part models showed a decreasing trend in costs with increasing number of years on treatment, with the exception of dialysis outpatient costs. Age did not have a consistent effect on hospital costs; however, comorbidities such as diabetes and peripheral vascular disease were strong predictors of higher hospital costs in all four models.
Conclusion
Analysis of patient-level data can result in a deeper understanding of factors associated with variations in hospital costs and can improve the accuracy with which costs are estimated in the context of economic evaluations.
Similar content being viewed by others
References
Tonelli, M., Wiebe, N., Knoll, G., Bello, A., Browne, S., Jadhav, D., Klarenbach, S., Gill, J.: Systematic review: kidney transplantation compared with dialysis in clinically relevant outcomes. Am. J. Transplant. 11(10), 2093–2109 (2011)
Department of Health. The National Service Framework for renal services. Part one: dialysis and transplantation (2004), https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/199001/National_Service_Framework_for_Renal_Services_Part_One_-_Dialysis_and_Transplantation.pdf. Accessed 16 July 2014
Rao, A., Steenkamp, R., Caskey, F.: UK Renal Registry 16th annual report. Chapter 5. Comorbidities and current smoking status amongst patients starting renal replacement therapy in England, Wales and Northern Ireland from 2011 to 2012. Nephron. Clin. Pract 125, 99–110 (2013)
Metcalfe, W., Khan, I.H., Prescott, G.J., Simpson, K., Macleod, A.M.: Hospitalization in the first year of renal replacement therapy for end-stage renal disease. QJM 96(12), 899–909 (2003)
Hospital episode statistics, http://www.hscic.gov.uk/hes. Accessed 2 April 2015
Fotheringham, J., Fogarty, D., Jacques, R., ElNahas, M., Campbell, M.: Chapter 13. The linkage of incident renal replacement therapy patients in England (2002–2006) to hospital episodes and national mortality data: improved demography and hospitalisation data in patients undergoing renal replacement therapy. Nephron. Clin. Pract 120(Suppl 1), c247–c260 (2012)
UK Renal Registry, https://www.renalreg.org/datasets/the-uk-renal-registry-dataset/. Accessed 2 April 2015
Department of Health. Confirmation of payment by results (PbR) arrangements for 2011-12, 2011-12 tariff information spreadsheet. http://webarchive.nationalarchives.gov.uk/20130507170152/https:/www.gov.uk/government/publications/confirmation-of-payment-by-results-pbr-arrangements-for-2011-12. Accessed 21 January 2014
Mullahy, J.: Much ado about two: reconsidering retransformation and the two-part model in health econometrics. J. Health. Econ. 17(3), 247–281 (1998)
Dunn, G., Mirandola, M., Amaddeo, F., Tansella, M.: Describing, explaining or predicting mental health care costs: a guide to regression models. Methodological review. Br. J. Psychiatry 183, 398–404 (2003)
Buntin, M.B., Zaslavsky, A.M.: Too much ado about two-part models and transformation? Comparing methods of modeling Medicare expenditures. J. Health. Econ. 23(3), 525–542 (2004)
Barber, J., Thompson, S.: Multiple regression of cost data: use of generalised linear models. J. Health Serv. Res. Policy 9(4), 197–204 (2004)
Hardin, J.W.H., J.M.: Generalized linear models and extensions, 2nd ed. Stata Press, Lakeway Drive, Texas (2007)
Kirkwood, B.R., Sterne, J.A.C.: Essential medical statistics, 2nd ed. Blackwell Publishing Oxford (2003)
Haller, M., Gutjahr, G., Kramar, R., Harnoncourt, F., Oberbauer, R.: Cost-effectiveness analysis of renal replacement therapy in Austria. Nephrol. Dial. Transplant. 26(9), 2988–2995 (2011)
Howard, K., Salkeld, G., White, S., McDonald, S., Chadban, S., Craig, J.C., Cass, A.: The cost-effectiveness of increasing kidney transplantation and home-based dialysis. Nephrology 14(1), 123–132 (2009)
Jassal, S.V., Krahn, M.D., Naglie, G., Zaltzman, J.S., Roscoe, J.M., Cole, E.H., Redelmeier, D.A.: Kidney transplantation in the elderly: a decision analysis. J. Am. Soc. Nephrol. 14(1), 187–196 (2003)
Kontodimopoulos, N., Niakas, D.: An estimate of lifelong costs and QALYs in renal replacement therapy based on patientsʼ life expectancy. Health Policy 86, 85–96 (2008)
de Wit, G.A., Ramsteijn, P.G., de Charro, F.T.: Economic evaluation of end stage renal disease treatment. Health Policy 44, 215–232 (1998)
Wong, G., Howard, K., Chapman, J.R., Chadban, S., Cross, N., Tong, A., Webster, A.C., Craig, J.C.: Comparative survival and economic benefits of deceased donor kidney transplantation and dialysis in people with varying ages and co-morbidities. PLoS one 7(1) (2012)
Briggs, A., Clark, T., Wolstenholme, J., Clarke, P.: Missing… presumed at random: cost-analysis of incomplete data. Health Econ. 12(5), 377–392 (2003)
Sterne, J.A., White, I.R., Carlin, J.B., Spratt, M., Royston, P., Kenward, M.G., Wood, A.M., Carpenter, J.R.: Multiple imputation for missing data in epidemiological and clinical research: potential and pitfalls. BMJ 338, b2393 (2009)
Bang, H.T., Tsiatis, A.A.: Estimating medical costs with censored data. Biometrika 87, 329–343 (2000)
Carides, G.W., Heyse, J.F., Iglewicz, B.: A regression-based method for estimating mean treatment cost in the presence of right-censoring. Biostatistics 1(3), 299–313 (2000)
Lin, D.Y., Feuer, E.J., Etzioni, R., Wax, Y.: Estimating medical costs from incomplete follow-up data. Biometrics 53(2), 419–434 (1997)
O’Hagan, A., Stevens, J.W.: On estimators of medical costs with censored data. J. Health Econ. 23(3), 615–625 (2004)
Young, T.A.: Estimating mean total costs in the presence of censoring: a comparative assessment of methods. Pharmacoeconomics 23(12), 1229–1242 (2005)
Acknowledgments
This article presents independent research commissioned by the National Institute for Health Research (NIHR) under the Programme Grant for Applied Research (RP-PG-0109-10116) entitled Access to Transplantation and Transplant Outcome Measures (ATTOM). The views expressed in this publication are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health. JF was funded by a Kidney Research UK Clinical Training Fellowship. The ATTOM Study Group comprises: J. Andrew Bradley, Clare Bradley, John Cairns, Heather Draper, Chris Dudley, John L. Forsythe, Damian G. Fogarty, Rachel J. Johnson, Geraldine Leydon, Wendy Metcalfe, Gabriel C. Oniscu, Rommel Ravanan, Paul Roderick, Charles R. Tomson and Christopher Watson. The authors are grateful to the UK Renal Registry and Hospital Episode Statistics for the linked dataset. Hospital Episode Statistics: Copyright 2014, re-used with the permission of the Health and Social Care Information Centre. All rights reserved.
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
A full list of members of the Access to Transplantation and Transplant Outcome Measures (ATTOM) Study Group is provided in the Acknowledgments.
Appendix: A worked example to predict hospital costs based on the final two-part model
Appendix: A worked example to predict hospital costs based on the final two-part model
To estimate annual inpatient costs for a 55-year-old male patient with diabetes who has been on haemodialysis for 3 years:
Part 1: probability of incurring any inpatient cost >£0
Taking the natural log of the odds ratios in Table 3, calculate log odds of incurring any inpatient cost
Calculate probability from log odds
Part 2: estimate level of inpatient cost based on coefficients in Table 5
Combine parts 1 and 2: multiply estimated level of inpatient cost by probability of incurring any cost
Rights and permissions
About this article
Cite this article
Li, B., Cairns, J., Fotheringham, J. et al. Predicting hospital costs for patients receiving renal replacement therapy to inform an economic evaluation. Eur J Health Econ 17, 659–668 (2016). https://doi.org/10.1007/s10198-015-0705-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10198-015-0705-x