Abstract
Background
Implants based on the polyetheretherketon (PEEK) polymer have been developed in the last decade as an alternative to conventional metallic devices. PEEK devices may provide several advantages over the use of conventional orthopedic materials, including the lack of metal allergies, radiolucency, low artifacts on magnetic resonance imaging scans and the possibility of tailoring mechanical properties. The purpose of this study was to evaluate the clinical results at 12-month follow-up using a new plate made of carbon-fiber-reinforced polyetheretherketon for the treatment of distal radius fractures.
Materials and methods
We included 40 consecutive fractures of AO types B and C that remained displaced after an initial attempt at reduction. The fractures were classified according to the AO classification: 21 fractures were type C1, 9 were type C2, 2 were type C3, 2 were type B1 and 6 were type B2.
Results
At a 12-month follow-up no cases of hardware breakage or loss of the surgically achieved fracture reduction were documented. All fractures healed, and radiographic union was observed at an average of 6 weeks. The final Disabilities of Arm, Shoulder and Hand score was 6.0 points. The average grip strength, expressed as a percentage of the contralateral limb, was 92 %. Hardware removal was performed only in one case, for the occurrence of extensor tenosynovitis.
Conclusion
At early follow-up this device showed good clinical results and allowed maintenance of reduction in complex, AO fractures.
Type of study/level of evidence
Therapeutic IV.
Similar content being viewed by others
Introduction
Open reduction and internal fixation using pre-contoured plates has become a surgical treatment option for displaced, unstable and comminuted fractures of the distal radius. They provide immediate stable fixation allowing early mobilization, which can result in rapid recovery and improved regain of function [1, 2]. Fixed angle plates using locking-screw technology allow surgeons to manage complex periarticular fractures since they give distal stability by direct support of the subchondral bone and do not depend on distal screw purchase to maintain reduction [1].
Distal radius plating can be performed using a dorsal or volar approach; however, a higher rate of tendon irritation and rupture has been reported with the use of dorsal plates [3]. Implants based on the polyetheretherketon (PEEK) polymer have been developed in the last decade as an alternative to conventional metallic devices. PEEK devices may provide several advantages over the use of conventional orthopedic materials, including the lack of metal allergies, radiolucency, low artifact interference on magnetic resonance imaging scans and the possibility of tailoring mechanical properties [4]. In fact, compared with clinically used metallic implants, CFR-PEEK implants can be designed with more appropriate strength, toughness, or stiffness by the arrangement of reinforcing fiber volume and orientation, and can provide better fatigue resistance [5].
Although neat (unfilled) PEEK biomaterials can exhibit an elastic modulus ranging between 3 and 4 GPa, the modulus can be tailored to closely match cortical bone (18 GPa) or titanium alloy (110 GPa) by preparing carbon-fiber-reinforced (CFR) composites with varying fiber length and orientation [6]. Therefore, PEEK has a more similar stiffness to bone than titanium.
A recent study compared the CFR-PEEK dynamic compression plate, distal radius volar plate, proximal humeral plate, and tibial nail to commercially available devices regarding the biomechanical characteristics (by four-point bending, static torsion of the nail, and bending fatigue) and the wear/debris (by amount of the debris generated at the connection between the CFR-PEEK plate and titanium alloy screws). The authors concluded that CFR-PEEK and metal implants yielded similar biomechanical characteristics to other commercially available devices. In particular, the distal volar plate bending structural stiffness of the CFR-PEEK distal volar plate was 0.542 versus 0.376 N m2 for the DePuy’s DVR anatomic volar plate. All tested CFR-PEEK devices underwent one million fatigue cycles without failure. Moreover, the wear test showed that the accumulated debris on the 1 mm filters weighed very little, i.e. an average of 0.78 mg of the CF-PEEK material in comparison to 5.35 mg of the titanium sample [7].
Numerous studies documenting the successful clinical performance of CFR-PEEK in orthopedic, trauma and spinal surgery continue to emerge in the literature [8–10].
The research presented here represents the continuation of a previously reported study [11] with the aim to evaluate the clinical results at a 12-month follow-up, using the new DiPHOS-RM plate made of CFR-PEEK for the treatment of the distal radius fracture.
Materials and methods
We performed a prospective study including all patients who were treated for unstable distal radius fracture with a volar fixed angle plate DiPHOS-RM produced by Lima Corporate (Villanova di San Daniele Del Friuli, Udine, Italy), during a period of 7 months (between March 2012 and September 2012). We included all the consecutive fractures of AO types B and C that remained displaced after an initial attempt at reduction. Fractures of AO type A were not included since they were treated nonsurgically. The patients were 16 men and 24 women with an average age of 65 years at the time of injury (range 26–82). The mechanisms of injury were simple falls on outstretched hands in 22 cases, motor vehicle accidents in 7 cases and sports injuries in another 11 cases. The fractures were classified according to the AO classification: 21 fractures were type C1, 9 were type C2, 2 were type C3, 2 were type B1 and 6 were type B2.
A preoperative computed tomography scan was carried out on all patients affected by type C fractures and in one patient a postoperative computed tomography scan was also obtained.
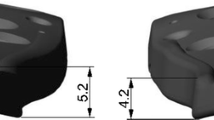
In this study, the researched plate (DiPHOS-RM, Lima corporate, Villanova di San Daniele, Italy) was manufactured by injection molding of CFR-PEEK and consists of two distal rows of holes for the 2.3 locking screws on the distal part of the plate, and three or more different holes for 3.5 locked screws on the diaphysis (Fig. 1).
The main differences between a CFR-PEEK plate and the most common materials in trauma implants (i.e. titanium plate) are the following:
-
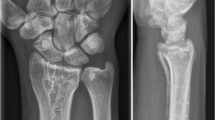
The CFR-PEEK is completely radiolucent, a property that allows direct evaluation of osseous callus formation because consolidation and mineralization is not obscured by the plate in both standard views. The position of the plate can be detected anyway in the radiographic controls thanks to tantalum markers positioned on the distal and proximal borders.
-
The specific design of the holes of the CFR-PEEK plate and of the head of the screw allows the insertion of the screws in multiple directions with high strength coupling.
-
The threaded coupling between the head of the screw and the plate holes in the titanium angular stability plates could cause cold welding, while coupling of screws and plate of different materials precludes cold welding.
-
The elastic modulus of CFR-PEEK is similar to the modulus of the cortical bone, an advantageous feature for an osteosynthesis device, in order to prevent reduction of bone quality adjacent to the plate [12].
In order to reach a strong angular stability between plate and screws, the right choice of material and production process (injection molding) combined with a specific geometry of the holes of the plate and of the thread of the head of the screws was made.
The self-threading screws were inserted using the specific screwdriver according to the surgical technique in order to completely insert the screw into the hole of the plate.
The operations were performed using Henry’s volar approach. The plate was placed directly on the radius after the reduction of the fracture, and the adequate positioning of plate and screws were confirmed by intraoperative fluoroscopy. Finally, the square pronator was sutured, allowing an almost complete coverage of the plate (Fig. 2).
a Preoperative 2- and 3-D CT scan showing a C1-type wrist fracture according to the AO classification. b Intraoperative view of distal radius fracture with the DiPHOS-RM implanted and the pronator quadratus re-attached. c X-ray evaluation performed 3 months after surgery showing good healing of the fracture
A below-elbow wrist splint was used for 2 weeks in all cases. At the end of the 2nd week, the sutures were removed and physiotherapy started.
As we usually do in our clinical practice, all patients were clinically and radiologically revised at 1, 2, and 3 months, and thereafter at 6-monthly intervals.
The clinical and radiological evaluation was performed by one of the authors and included analysis of passive range of motion (ROM), grip strength, functional outcome, radiological evaluation of fracture healing and reduction maintenance.
The X-ray assessment included standard antero-posterior and lateral projections of the injured wrist, and reduction maintenance was determined by assessing radial inclination, tilt, ulnar variance, step off, and gap. All measurements were performed on a picture archiving and communication system (PACS, software Fuji Synapse).
Time of union was determined according to both radiological and clinical parameters. Radiological criteria included: bridging of the fracture site by bone, callus or trabeculae; bridging of the fracture seen at the cortices; and obliteration of the fracture line or cortical continuity. Clinical criteria were represented by the patient’s ability to bear weight on the injured limb and perform activities of daily living, and the presence of pain at the fracture site upon palpation and physical stress.
Clinical results were assessed with physician-directed outcome tools and with subjective questionnaires after surgery.
Grip strength was measured with a Jamar dynamometer (Asimov Engineering Corp, Santa Monica, CA), and wrist ROM using a goniometer. Functional outcome was performed with the Disabilities of Arm, Shoulder and Hand (DASH) questionnaire. This instrument quantifies disabilities related to the upper extremity with a score ranging from 0 points (no disability) to 100 points (maximum disability) [13]. Possible early or late complications were assessed and recorded at each follow-up evaluation.
Results
At a 12-month follow-up all the patients included were clinically and radiologically reviewed.
Thirty-four patients who were in employment at the time of injury were able to return to work within 14 weeks of injury. All fractures healed, and radiographic union was observed at an average of 6 weeks (range 4–8 weeks). No cases of loss of the surgically achieved fracture reduction were documented. The clinical evaluation and outcome scores data at the final follow-up are reported in Table 1. In particular, the average wrist range of motion was: 65° in flexion (range 45°–80°), 55° in extension (range 40°–65°), 21.5° in radial deviation (range 5°–35°), 33.5° in ulnar deviation (range 30°–45°), 75° in supination (range 65°–90°), and 79° in pronation (range 60°–90°). The final DASH score was 6 points (range 3–16). The average grip strength, expressed as percentage of respective contralateral limb, was 92 %. No cases of hardware failure, loss of position or alignment of fixed-angle locking screws, nervous complications, infection or allergy to the plate were observed in our cohort of patients. In one case, a 55-year-old male, clinical signs of extensor tendons synovitis were reported 6 months after surgery. The diagnosis of extensor tenosynovitis was primarily based on the symptoms of pain, swelling, tenderness, and dorsal crepitus. Radiographs revealed an excessive length of one screw of the distal branch of the plate, after which the plate and the screws were removed. Intraoperative hardware osseointegration was found to be limited, facilitating, therefore, removal of the plate.
Discussion
The primary aim in the management of unstable distal radius fractures is to obtain restoration of bony anatomy with stable internal fixation [14]. Secondary to its ability to provide stable internal fixation of a distal radius fracture, volar locking plate technology has gained significant popularity [15].
Numerous studies have reported outcomes in the good to excellent range on patient-rated scoring systems and with a relatively low rate of complications using volar plating as a treatment for unstable distal radius fractures [16–21].
In the present study the overall clinical results obtained with the use of the new DiPHOS-RM plate at 12-month follow-up are consistent with the recent literature findings using conventional metal plates [16–21].
However, the CFR-PEEK structure of the DiPHOS-RM plate has potential advantages that may support its introduction into clinical practice.
Compared with traditional implants, such as stainless steel, Co–Cr–Mo, and Ti6A14 V alloy stainless steel or titanium plates, PEEK polymer has a modulus and strengths similar to normal bone, avoiding the strong rigidity property of titanium or stainless steel plates [12, 22].
Typically, metals used in orthopedic surgery have a large elastic modulus (approximately 6–20 times greater than that of the surrounding bone) [23–25], causing impaired load force transmission at the implant–tissue interface.
Thus, according to Wolff’s law, the device may sustain far higher stresses than the bone to which it is rigidly fixed, thereby shielding the bone for stresses. Because bone requires the stimulus of mechanical stress to maintain its structure, the bone adjacent to the high modulus device becomes porotic and weaker [26, 27].
Another advantage of using a PEEK plate with metal screws is that the potential phenomenon of cold welding is eliminated. Moreover, this new plate allows in its distal part both the insertion of fixed-angle screws or distally locked screws at variable angles and with an angular range of 15° by deciding whether or not to use the provided guide. Finally, the major advantage of the DiPHOS-RM plate is its radiolucency. This characteristic allows direct visualization of osseous callus formation, allowing monitoring of the healing of the fracture, thereby improving clinical assessment and accuracy.
Therefore, specific indications for this new radiolucent plate can be represented by fractures with significant metaphyseal comminution and in cases of nascent malunion where a distal radius osteotomy with bone grafting is usually performed to correct the wrong angle.
In our cohort of patients we haven’t found any complications related to the new material of the implant, but particular care and attention is necessary while inserting the screws, as the holes of the plate are not threaded. The penetration of the screw into the hole of the plate creates a thread, allowing locking of the screws, but no more than three changes of angle is possible before the thread is ruined.
In our cohort of patients, no cases of hardware breakage, loss of the surgically achieved fracture reduction, or allergy to the plate were documented at a 12-month follow-up. The hardware was removed only in one case (5 %) for the occurrence of extensor tenosynovitis after a screw penetrated the dorsal radius cortex.
In this research we observed a limited osseointegration of this hardware, probably allowing, when necessary, an easier removal of the plate with respect to the other routinely used materials.
Compared with stainless steel or titanium plates, the cost of production of this implant is higher but the commercial price is in line with that of the metal systems.
Our first experience of using the new DiPHOS-RM plate seems favorable: in fact the plate proved to be a reliable method with good clinical and functional results at a 12-month follow-up. In addition, its distal double-row screw system and its far positioning within the distal radius epiphysis resulted in a reliable support for the articular surface, allowing maintenance of reduction even in cases of comminuted intra-articular fractures (i.e. C-type).
Future studies with a larger sample size are needed to evaluate the long-term clinical results and occurrence of possible complications at a longer follow-up using this new CFR-PEEK plate.
References
Orbay J (2005) Volar plate fixation of distal radius fractures. Hand Clin 21:347–354
Soong M, van Leerdam R, Guitton TG, Got C, Katarincic J, Ring D (2011) Fracture of the distal radius: risk factor for complication after locked volar plate fixation. J Hand Surg Am 36:3–9. doi:10.1016/j.jhsa.2010.09.033
Wei J, Yang TB, Luo W, Qin JB, Kong FJ (2013) Complications following dorsal versus volar plate fixation of distal radius fracture: a meta-analysis. J Int Med Res 41:265–275. doi:10.1177/0300060513476438
Baidya KP, Ramakrishna S, Rahman M, Ritchie A (2001) Quantitative radiographic analysis of fiber reinforced polymer composites. J Biomater Appl 15:279–289
Akay M, Aslan N (1995) An estimation of fatigue life for a carbon fibre/poly ether ether ketone hip joint prosthesis. Proc Inst Mech Eng [H] 209:93–103
Skinner HB (1998) Composite technology for total hip arthroplasty. Clin Orthop Relat Res 235:224–236
Steinberg EL, Rath E, Shlaifer A, Chechik O, Maman E, Salai M (2013) Carbon fiber reinforced PEEK Optima—a composite material biomechanical properties and wear/debris characteristics of CF-PEEK composites for orthopedic trauma implants. J Mech Behav Biomed Mater 17:221–228. doi:10.1016/j.jmbbm.2012.09.013
Rhee PC, Shin AY (2013) The rate of successful four-corner arthrodesis with a locking, dorsal circular polyether-ether-ketone (PEEK-Optima) plate. J Hand Surg Eur 38:767–773. doi:10.1177/1753193413475962
Nakahara I, Takao M, Bandoh S, Bertollo N, Walsh WR, Sugano N (2013) In vivo implant fixation of carbon fiber-reinforced PEEK hip prostheses in an ovine model. J Orthop Res 31:485–492. doi:10.1002/jor.22251
Kasliwal MK, O’Toole JE (2014) Clinical experience using polyetheretherketone (PEEK) intervertebral structural cage for anterior cervical corpectomy and fusion. J Clin Neurosci 21:217–220. doi:10.1016/j.jocn.2013.03.018
Tarallo L, Mugnai R, Adani R, Catani F (2013) A new volar plate DiPHOS-RM for fixation of distal radius fracture: preliminary report. Tech Hand Up Extrem Surg 17:41–45. doi:10.1097/BTH.0b013e31827700bc
Kurtz SM, Devine JN (2007) PEEK biomaterials in trauma, orthopedic, and spinal implants. Biomaterials 28:4845–4869
Hudak PL, Amadio PC, Bombardier C (1996) Development of an upper extremity outcome measure: the DASH (disabilities of the arm, shoulder and hand) [corrected]. The Upper Extremity Collaborative Group (UECG). Am J Ind Med 29:602–608
Tarallo L, Adani R, Mugnai R, Catani F (2011) The treatment of distal radius articular fractures of C1-C2 type DVR plate: analysis of 40 cases. Musculoskelet Surg 95:225–320. doi:10.1007/s12306-011-0140-9
Arora R, Lutz M, Hennerbichler A, Krappinger D, Espen D, Gabl M (2007) Complication following internal fixation of unstable distal radius fracture with palmar locking-plate. J Orthop Trauma 21:316–322
Gruber G, Zacherl M, Giessauf C, Glehr M, Fuerst F, Liebmann W, Gruber K, Bernhardt GA (2010) Quality of life after volar plate fixation of articular fractures of the distal part of the radius. J Bone Joint Surg Am 92:1170–1178. doi:10.2106/JBJS.I.00737
Arora R, Lutz M, Deml C, Krappinger D, Haug L, Gabl M (2011) A prospective randomized trial comparing nonoperative treatment with volar locking plate fixation for displaced and unstable distal radial fractures in patients sixty-five years of age and older. J Bone Joint Surg Am 93:2146–2153. doi:10.2106/JBJS.J.01597
Jupiter JB, Marent-Huber M, LCP Study Group (2009) Operative management of distal radial fractures with 2.4-millimeter locking plates: a multicenter prospective case series. J Bone Joint Surg Am 91:55–65. doi:10.2106/JBJS.G.01498
Kim JK, Park SD (2013) Outcomes after volar plate fixation of low-grade open and closed distal radius fractures are similar. Clin Orthop Relat Res 471:2030–2035. doi:10.1007/s11999-013-2798-9
Hershman SH, Immerman I, Bechtel C, Lekic N, Paksima N, Egol KA (2013) The effects of pronator quadratus repair on outcomes after volar plating of distal radius fractures. J Orthop Trauma 27:130–133. doi:10.1097/BOT.0b013e3182539333
Tosti R, Ilyas AM (2013) Prospective evaluation of pronator quadratus repair following volar plate fixation of distal radius fractures. J Hand Surg Am 38:1678–1684. doi:10.1016/j.jhsa.2013.06.006
Toth JM, Wang M, Estes BT, Scifert JL, Seim HB 3rd, Turner AS (2006) Polyetheretherketone as a biomaterial for spinal applications. Biomaterials 27:324–334
Kitamura E, Stegaroiu R, Nomura S, Miyakawa O (2004) Biomechanical aspects of marginal bone resorption around osseointegrated implants: considerations based on a three-dimensional finite element analysis. Clin Oral Implants Res 15:401–412
Rho JY, Ashman RB, Turner CH (1993) Young’s modulus of trabecular and cortical bone material: ultrasonic and microtensile measurements. J Biomech 26:111–119
Isidor F (2006) Influence of forces on peri-implant bone. Clin Oral Implants Res 17(Suppl. 2):8–18
Slätis P, Karaharju E, Holmström T, Ahonen J, Paavolainen P (1978) Structural changes in intact tubular bone after application of rigid plates with and without compression. J Bone Joint Surg Am 60:516–522
Huiskes R, Weinans H, van Rietbergen B (1992) The relationship between stress shielding and bone resorption around total hip stems and the effects of flexible materials. Clin Orthop 274:124–134
Conflict of interest
None.
Ethical standards
(1) The patients gave informed consent prior to being included in the study, (2) the study was authorized by the local ethical committee and was performed in accordance with the ethical standards of the 1964 Declaration of Helsinki as revised in 2000.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution License which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
About this article
Cite this article
Tarallo, L., Mugnai, R., Adani, R. et al. A new volar plate made of carbon-fiber-reinforced polyetheretherketon for distal radius fracture: analysis of 40 cases. J Orthopaed Traumatol 15, 277–283 (2014). https://doi.org/10.1007/s10195-014-0311-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10195-014-0311-1