Abstract
Background
Probabilistic decision analysis is a means of reflecting the uncertainty parameter in models and of presenting it in a comprehensible manner to decision-makers.
Materials and methods
A cost-effectiveness model was constructed to compare the cementless and cemented total hip prostheses implanted at our department in terms of lifetime costs and quality-adjusted life-years (QALY). Revision rates were obtained from the Orthopaedic Prosthesis Register of the Laboratory of Medical Technology, Istituti Ortopedici Rizzoli, Bologna, Italy.
Results
The risk of early revision (at 5 years of follow-up) for cementless and cemented prostheses was 1.6% and 1.4%, respectively, resulting in equal QALY for the two implant types. Analysis of mean cost and QALY indicated that use of either implant is not associated with cost savings.
Discussion
Management with cementless or cemented total hip prostheses in a theoretical cohort of 70-year-old patients with fracture of the femoral neck or arthritis involving the hip is not significantly different according to the probabilistic results from the model.
Similar content being viewed by others
Introduction
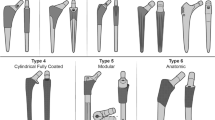
Excellent long-term clinical and radiographic outcomes have been reported for total hip arthroplasty (THA) using traditional cementless and cemented prostheses [1, 2]. Hip prosthesis technology is continually evolving, with new designs and fixation methods being proposed and introduced [3]. Orthopaedic innovation in THA technology has been referred to as a “trial and error culture” [3]. In Italy, where over 150 different implant models are used, there is no nationally coordinated monitoring of new THA devices and their use [4]. A growing number of prostheses is available, with little or no scientific evidence that the newer implants are any better than the established ones [5].
Randomized controlled trials are the gold standard for demonstrating the clinical benefits of new technologies. However, detecting small differences in failure rates among implants requires randomizing large numbers of patients and following them for extended periods (15–20 years, or longer). These studies are difficult to perform due to practical considerations of time and cost. In contrast, decision-analysis techniques offer the potential to analyze the performance of a new technology prior to the availability of long-term clinical outcome data. Furthermore, the results from a well-designed decision analysis study can guide further clinical and laboratory research based on the variables that have the greatest influence on cost-effectiveness. Finally, a cost effectiveness framework can also be readily updated as new information on cost-and clinical effectiveness emerges from randomized trials and cohort studies [6].
The primary objectives of this study were to establish a framework within which to evaluate the cost-effectiveness of cementless and cemented implants and to analyze how device cost and revision rates affect the model.
Patients and methods
A Markov decision model was used to analyze a theoretical cohort of 70-year-old patients with unsuccessful management of femoral neck fracture or arthritis involving the hip [7]. Seventy years is the average age of THA recipients according to the report of the Regional Orthopaedic Prosthesis (RIPO) register of the Laboratory of Medical Technology, Istituti Ortopedici Rizzoli, Bologna. The clinical scenario modelled in the study is shown in Fig. 1.
Outcomes and utilities were measured as quality-adjusted life-years (QALY), and costs were measured in 2006 euros from the database of our institution. All costs and outcomes incurred after time zero were discounted at a yearly rate of 3% for consistency with current cost-effectiveness analysis practices in medicine [8]. The model (Fig. 2) was constructed using a decision-analysis software (TreeAge Pro 2004; TreeAge Software, Williamstown, USA).
The following general assumptions were made in model construction [9]: patients with successful cemented or cementless implants the same utility, or QALY value, after the initial postoperative period; the mortality rates of patients who survived THA do not differ from the age-adjusted mortality rates of patients who did not undergo THA; revision of either a cemented or a cementless device is by total replacement and has the same cost and functional outcomes; and, patients undergo a single revision and remain in the “well with revision” state until death. The specific parameter values used in the decision model are shown in 1.
Data from the RIPO register, recording 23966 THAs, were used to estimate the probability of revision of cemented and cementless implants [10]. The probability of infection after implantation of a total cemented or cementless prosthesis was set at 0.044% for the base case [11]. All patients who had an infection were presumed to have had a revision procedure.
The age-specific probability of death from causes unrelated to THA was made equal to the probability of death at each specific age, as determined from the 2001 United States Life Tables [12]. The probability of perioperative death for patients undergoing THA was estimated from the study of Chang and co-workers [11], who calculated rates of 0.34% for primary THA and of 1.2% for revision THA. In this study, the probability of perioperative death after a primary cemented THA was assumed to be the same as after cementless THA for the base case.
The utilities used in the model were based on quality well-being index scores [13] reported in the literature [11]. A longitudinal cohort study of 1356 patients demonstrated quality well-being index scores of 0.92 in arthritis patients aged 75–84 years and of 0.80 after revision surgery compared with 0.71 in patients without arthritis in the same age group [14]. The final utility values used for the base case in the model are shown in 1.
The costs of cementless and cemented THA were estimated from a payer perspective using average hospital costs for prosthetic implants in 2006 euros.
The two treatment strategies were evaluated with the model by calculating the incremental cost-effectiveness ratio. Medical interventions with an incremental cost-effectiveness ratio less than 50,000 per QALY were deemed to be reasonably cost-effective and this value was used in threshold analysis. Both future costs and future utilities, or QALY, were discounted at 3% for consistency with current practices in cost-effectiveness analysis [8].
Results
Several different devices (Samo Duofit, Wright Medical, Stryker, Zimmer, Hit Medica, Plus Orthopedics, Adler Ortho) are regularly implanted at our Orthopaedics Department. The mean costs of cemented and cementless devices listed above were € 1146 and € 3206.44, respectively (average difference, € 2060.44); the mean procedure cost of revision THA was € 3249.75 (1).
With a threshold value of € 50,000, cementless THA becomes more effective (but not more cost-effective) and costly (but less effective) than cemented THA (2). However, neither procedure was clearly dominated by the other (Fig. 3).
The model is sensitive to revision rates, implant costs, perioperative mortality and infection rates, and utility values. Analysis of 5-year follow-up data reported in the RIPO register revealed that, with a 1.4% annual probability of revision, cementless prostheses becomes less costly. With an incremental cost-effectiveness ratio above € 50,000 per QALY threshold, cemented implants do not become cost-inefficient. If the probability of revision of cemented THA is held constant, cementless implants do not become less costly. In fact, even if the annual revision rate of total cementless prostheses were 0% (i.e. no revisions), the cost of each additional QALY gained by choosing a cementless device is greater than $ 50,000 per QALY, the commonly accepted threshold for cost-effective interventions. This suggests that, under our assumptions, cementless THA may not be more cost-effective, regardless of its revision rates.
The results demonstrate that the mortality associated with cemented THA would have to exceed the rate commonly associated with cementless THA to become the more cost-effective option in this patient population. Similarly, the infection rates associated with cemented implants would need to be higher than the rate associated with cementless devices to be the more cost-effective strategy.
Discussion
Over 150 different types of prosthesis are currently used in Italy, with significant price differences. Although reasons for implant choice may include knowledge of prosthesis survival and function, Baxter and Bevan [3] suggested that manufacturers exert a degree of influence over surgeons’ preferences, with some orthopaedics departments being supplied by a single manufacturer. The costs associated with a range of prosthesis prices are made explicit in this paper.
The cost-effectiveness profile of cemented prostheses was found to be similar to that of cementless implants for the surgical management of hip arthritis and femoral neck fractures in a theoretical elderly population based on RIPO report data. The average cost difference was € 2060.44 in 2006 euros, without differences in QALY.
The main conclusions based on the assumptions adopted in this study are that device cost and revision rates are the main costs driving total expected costs. Based on the data used in the model, cementless prostheses appear to be less costly than cemented ones over 5 years, but not less cost-effective when an incremental cost effectiveness ratio of less than € 50,000 per QALY was adopted. In our theoretical 70-year-old patients, a low-price prosthesis is generally less costly than a high-price one, even with a very low revision rate.
One possible limitation of this study is the use of 5-year prosthesis survival data. The survival rate of many implants diminishes (sometimes dramatically) over time. Increases in revision rates to levels above those assumed will increase total expected costs. Cost rankings will also be changed if rates of revision change relative to each other.
We did not investigate the effects of different devices on patients’ quality of life. An interesting area for future research would be to compare prosthesis survival and quality of life data.
Another potential limitation of our study is that we only considered implant cost, which is the most easily quantifiable cost for which accurate data could be obtained. Future models should take into account the impact of all societal costs, including direct, indirect and non-medical costs, on the cost-utility of THA.
We also recognize that chronological age is an imperfect surrogate for physiological age and activity level, which may be more appropriate criteria on which to base a decision-analysis model. However, most investigators who have evaluated predictors of wear rates and implant survival following THA have used chronological age as a proxy for activity level [15].
It is increasingly recognized that decision-analytic models are useful frameworks for cost-effectiveness analysis for decision making. This is because all decisions about health technologies inevitably face uncertainties about the evidence base [16, 17].
National Institute for Clinical Excellence (NICE) guidelines have emphasized the central role of decision models in health technology assessment. In fact, all analyses used in NICE decision making have to include probabilistic sensitivity analysis [18].
The cost-effectiveness acceptability curves indicate the probability of a given intervention being the more (most) cost effective given the valuation of a unit of health outcome [19].
Decision-makers increasingly seek to identify those patients for whom a technology is most cost-effective; probabilistic sensitivity analysis provides a way of showing the additional uncertainty associated with splitting patients into subgroups. Perhaps most importantly, probabilistic sensitivity analysis can be extended to undertake value of information analysis to inform priority-setting and the design of future research [20].
Finally, it should be noted that the purpose of decision-analysis studies is not to influence individual clinical decisions for individual patients, but rather to provide a framework to help clinicians, patients, hospitals, payers, and health policy makers to evaluate the relative cost and relative clinical effectiveness of new healthcare technologies such as alternative bearing surfaces.
References
Berry DJ, Harmsen WS, Cabanela ME, Morrey BF (2002) Twenty-five-year survivorship of two thousand consecutive primary Charnley total hip replacements: factors affecting survivorship of acetabular and femoral components. J Bone Joint Surg Am 84:171–177
Soderman P, Malchau H, Herberts P (2000) Outcome after total hip arthroplasty: Part I: General health evaluation in relation to definition of failure in the Swedish National Total Hip Arthroplasty register. Acta Orthop Scand 71:354–359
Baxter K, Bevan G (1999) An economic model to estimate the relative costs over 20 years of different hip prostheses. J Epidemiol Community Health 53:542–547
Revisione sistematica sulle protesi d’anca: affidabilità dell’impianto. National Program for Guidelines (PNLG), Rome, no. 8 (revised, 2007). Available from http://www.globeweb.org/documenti/pdf/PNLG_Protesi_anca.pdf (Accessed on May 1, 2007)
Murray DW, Carr AJ, Bulstrode CJ (1995) Which primary total hip replacement? J Bone Joint Surg Br 77:520–527
Bernstein J (1997) Current concepts review — decision analysis. J Bone Joint Surg Arm 79:1404–1414
Hunink MG, Glasziou P, Siegel JE et al (2001) Decision making in health and medicine: integrating evidence and values. Cambridge University, Cambridge
Gold MR, Siegel JE, Russell LB, Weinstein MC (1996) Cost-effectiveness in health and medicine. Oxford University, New York
Slover J, Espehaug B, Havelin LI et al (2006) Cost-effectiveness of unicompartmental and total knee arthroplasty in elderly low-demand patients. A Markov decision analysis. J Bone Joint Surg Am 88(11):2348–2355
Registro dell’Implantologia Protesica Ortopedica Laboratory for Medical Technology, Rizzoli Orthopedics Institute: Available from https://ripo.cineca.it/pdf/049_2005.pdf (Accessed on May 1, 2007)
Chang RW, Pellisier JM, Hazen GB (1996) A cost-effectiveness analysis of total hip arthroplasty for osteoarthritis of the hip. JAMA 275(11):858–865
Arias E (2004) United States life tables, 2001. Natl Vital Stat Rep 52:1–38
Coons SJ, Rao S, Keininger DL, Hays RD (2000) A comparative review of generic quality-of-life instruments. Pharmacoeconomics 17:13–35
Fryback DG, Dasbach EJ, Klein R et al (1993) The Beaver Dam Health Outcomes Study: initial catalog of health-state quality factors. Med Decis Making 13:89–102
Bozic KJ, Morshed S, Silverstein MD et al (2006) Use of cost-effectiveness analysis to evaluate new technologies in orthopaedics: the case of alternative bearing surfaces in total hip arthroplasty. J Bone Joint Surg Am 88(4):706–714
Claxton K, Sculpher M, Drummond M (2002) A rational frame-work for decision making by the National Institute for Clinical Excellence. Lancet 360:711–715
Hjelmgren J, Berggren F, Andersson F (2001) Health economic guidelines: similarities, differences and some implications. Value Health 4(3):225–250
National Institute for Clinical Excellence. Guide to the methods of technology appraisal. Available from http://www.nice.org.uk/nicemedia/pdf/Guidance_on_the_selection_of_hip_prostheses.pdf (Accessed on May 1, 2007)
Briggs AH (1999) A Bayesian approach to stochastic cost-effectiveness analysis. Health Econ 8:257–262
Claxton K, Posnett J (1996) An economic approach to clinical trial design and research priority-setting. Health Econ 5:513–524
Acknowledgements
We are grateful to Dr. Silvia Modena for reviewing the English.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 2.0 International License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Marinelli, M., Soccetti, A., Panfoli, N. et al. Cost-effectiveness of cemented versus cementless total hip arthroplasty. A Markov decision analysis based on implant cost. J Orthopaed Traumatol 9, 23–28 (2008). https://doi.org/10.1007/s10195-008-0100-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10195-008-0100-9