Abstract
Serotonin is involved in several central nervous system functions including pain threshold, mood regulation and drug reward. Overuse of acute medications is commonly identified as a causative factor for medication overuse headache (MOH). Apparently, MOH shares with other kinds of drug addiction some common neurobiological pathways. The objective of this study is to assess the role of serotonin metabolism genes in the genetic liability to MOH. We performed a genetic association study using polymorphisms of five serotonin metabolism-related genes: serotonin transporter (5HTT), serotonin receptor 1A (5-HT1A), serotonin receptor 1B (5-HT1B), serotonin receptor 2A (5-HT2A) and serotonin receptor 6 (5HT6) genes. We compared 138 patients with MOH with a control sample of 117 individuals without headache and without drug overuse, and with 101 patients with migraine without aura but without drug overuse (MO). The genotypic and allelic distributions of all polymorphisms investigated did not differ among the three groups. In conclusion, our study does not provide evidence that the 5HTT, 5-HT1A, 5HT1B, 5HT2A and 5HT6 gene polymorphisms play a role in the genetic predisposition to MOH.
Similar content being viewed by others
Introduction
Chronic headache (CH), a group of headaches occurring daily or almost daily, is a major clinical concern and a common health risk. Overuse of acute medications, being present in more than 80% of CH patients seen in tertiary headache centres, is commonly identified as the most important risk factors for CH and a causative factor for medication overuse headache (MOH) [1].
Apparently, MOH shares with other kinds of drug addiction some common neurobiological pathways, including those that modulate reward, novelty seeking, behavioural control and response to stress [2]. Liability to drug dependence has been traced to polymorphisms in genes regulating monoaminergic transmission [3]. In particular, several serotonin metabolism-related polymorphisms have been associated with addiction, psychiatric disorders and migraine headache.
Few studies have focused on the genetics of CHs. Russell et al. [4] found that first-degree relatives of probands with chronic tension-type headache (CTTH) had a 2.1- to 3.9-fold significantly increased risk of CTTH with respect to the general population. We found that CH sufferers had significantly higher positive family history for CH compared to episodic headache sufferers. In particular, patients with CH associated with drug overuse had more frequently family history of drug overuse and substance abuse [5]. The significantly increased familial risk for CH, drug overuse and substance abuse suggests that genetic factors are involved in the process of headache chronification.
Homozygosis for the short allele of the 5-HTTLPR (S/S genotype), a polymorphism in the serotonin transporter gene regulatory region, has been found to be associated with an increased frequency of attacks in migraine patients compared with those with l/S or l/l genotype [6]. Park et al. [7] studied patients with CTTH with and without analgesic overuse, demonstrating an excess frequency of the 5-HTTLPR short allele (S/S genotype) in the analgesic overuse group. We performed a genetic association study of serotonin metabolism-related genes in three population groups: one affected with MOH, one with episodic migraine without aura and without drug abuse (MO) and one control population without headache and without drug abuse.
We analysed polymorphisms in five serotonin metabolism-related genes: the serotonin transporter (5HTT), serotonin receptor 1A (5-HT1A), serotonin receptor 1B (5-HT1B), serotonin receptor 2A (5-HT2A) and serotonin receptor 6 (5HT6) genes. The 5HTT gene codes for a protein responsible for the reuptake of serotonin from the extracellular space and has an important role in determining the magnitude and duration of serotonin activity on its pre- and post-synaptic receptors. The 5-HT1A, 5HT1B, 5HT2A and 5HT6 genes code for different serotonin receptors.
Patient and methods
Description of analysed populations
A total of 138 unrelated patients affected with MOH aged 22–81 were compared with a control population of 117 unrelated individuals without headache and without drug overuse, and to a population of 101 patients with episodic migraine without aura without drug overuse (MO). All patients were referred to the Neurological Department of the University of Bologna and to the Headache Centre of the University of Modena and Reggio-Emilia, two Italian tertiary Headache Centres. To reduce stratification bias, the populations studied came from the same region in North-Eastern Italy, Emilia-Romagna, and all were of Caucasian origin. The control population was composed of healthy laboratory staff and neurological patients without migraine. All controls and MO individual had to be over age 40, in order to reduce ascertainment bias related to age of onset of migraine headache. The institutional review board of the Department of Neurological Sciences of the University of Bologna Medical School approved the project and each patient gave informed consent to the study.
All patients and normal subjects were diagnosed by headache expert physician after direct interview according to the revised diagnostic criteria of the International Headache Society classification (ICHD-II) [8]. At the time of the visit a headache specialist performed a semi-structured history-taking interview and a neurological examination. Patients were asked about headache characteristics at onset and at the time of the inclusion in the study. Headache frequency and drug overuse were evaluated by means of headache diaries filled in for at least 3 months previous to inclusion. All patients and controls were investigated about family history for headache and for substance abuse. Substance use disorders and comorbidity for mood and anxiety disorders were diagnosed by mean of semi-structured interviews by trained doctors and reported according to Axis I of the DSM-IV criteria.
Genetic analysis
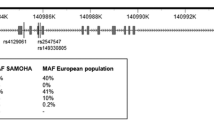
We studied the following DNA polymorphisms: a variable number of tandem repeats (VNTR) of 17-base-pair (bp) repeats located in the second intron of 5HTT localised on chromosome 17q12 (STin 2 polymorphism: STin 2.8, STin 2.9, STin 2.10, STin 2.11, STin 2.12) [9]; a transition A → G at nucleotide 82 of 5-HT1A located on chromosome 5q11.2-q13, which leads to an amino acid exchange (Ile → Val) in position 28 of the receptor protein [10]; a T → C transition in position 102 in exon 1 of 5-HT2A that does not alter the amino acid composition (chromosome 13q14-21) [11]; a silent G → C substitution at position 861 in the coding sequence, and a T → G transition at position −261of 5-HT1B (chromosome 6q13-q15) [12], and a silent C → T transition in position 267 of the coding region of the 5HT6 localised in 1p35-36 [13].
Molecular techniques for DNA extraction and amplification were those previously reported [14]. Due to technical difficulties (DNA exhaustion, PCR failure), the number of individuals examined in the different samples varied (see tables).
Statistical analysis
Chi-square analysis was used to test for deviations of genotype frequencies from Hardy–Weinberg expectations for both biallelic systems and STin 2 polymorphism for which only three alleles have been observed in our sample (STin 2.8, STin 2.9 and STin 2.12). Genotypic and allelic frequencies among the different groups were compared using the log-linear analysis for categorical data in two-dimensional tables or Fisher’s exact test. The test of non-random association of alleles at different loci (linkage disequilibrium estimate) was performed by Arlequin Software, Ver 3.0. Multivariate logistic regression was used to test for interaction between polymorphisms. The level of significance was chosen as P < 0.05. When necessary, P values were subject to Bonferroni’s correction for multiple comparisons.
Results
Clinical features of MOH patients are reported in Table 1.
All the polymorphisms analysed were in Hardy–Weinberg equilibrium except for the STin 2 polymorphism in the MOH group (χ2 = 10.03, P = 0.018). The 5HT1B (G861C) was in linkage disequilibrium with the 5-HT1B (C-261T) polymorphism (χ2 = 19.70, P = 0.00057).
The genotypic and allelic distributions of SNPs at the 5HT1B, 5HT2A and STin 2 in 5HTT did not differ among the three groups at the exact test of population differentiation as shown in Tables 2, 3 and 4.
Concerning the 5HT1A (A82G) polymorphism we found an indication of a genetic difference in the MOH compared to the MO group both for genotypic and for allelic distribution (P = 0.039 and P = 0.049, respectively) mainly as a result of an under-representation of allele G in the MOH group (Table 5). However, the results were not significant after the Bonferroni’s correction.
For the (C267T) polymorphism in the 5HT6 receptor gene, we found a significant allelic difference in MOH compared with control group (P = 0.033) mainly because of an overrepresentation of allele C in the MOH group, but we found no differences between MO and MOH (Table 6). In this case too, the P value became non-significant after Bonferroni’s correction. A multivariate analysis did not show interactions between the analysed polymorphisms.
Discussion
In this genetic association study, we analysed polymorphisms of five genes involved in the serotonergic pathways in patients with CH and drug overuse compared with a control population of individuals without headache and without drug overuse, and to a sample of patients with migraine headache without overuse. As in our previous study [15], these multiple comparisons were meant to search for genetic traits specifically associated with drug overuse in headache patients and to separate these from possibly different liabilities to headache pain.
No differences were found for allelic or genotypic distributions of the polymorphisms at the 5HTT, 5HT1B, 5HT2A, 5HT1A and 5HT6 genes. The STin 2 polymorphism was not in Hardy–Weinberg equilibrium in the MOH group but the size of the samples and its triallelic distribution could account for this finding. The 5HT1B (G861C) polymorphism was in linkage disequilibrium with the 5-HT1B (C-261T) polymorphism, indicating that both alleles are likely part of an extended haplotype.
On the basis of our data, these genes do not seem to be implicated in the genetic liability either to migraine or to MOH. These results confirm our previous negative genetic studies performed in a different set of patients in which we did not found any association between migraine and serotonin metabolism genes [16, 17]. However, to exclude definitively a role of the studied genes in the phenotype of MOH, a larger sample size is recommended.
Previous associations between the 5HTT (STin 2) polymorphism and migraine with and without aura [18, 19] were not confirmed in our population. However, we cannot exclude an involvement of other 5HTT gene polymorphisms, such as the 5-HTTLPR, in the genetic liability to migraine or MOH as previously reported [6, 7]. However, STin 2 was found to be in linkage disequilibrium with 5-HTTLPR in different populations, and the two polymorphisms have a combined effect on the rate of 5HTT mRNA transcription [20]. We chose to analyse the STin 2 polymorphism because it seems to influence the gene transcription in an allele-dependent manner and may thus modify neuronal transmission.
In conclusion, our study does not provide evidence that polymorphisms at the 5HTT, 5-HT1A, 5HT1B, 5HT2A and 5HT6 genes play a role in the genetic predisposition to MOH. However, we believe that our findings need confirmation in other genetically diverse populations. Genetic association studies are indeed susceptible to false positives due to genetic population diversity, population structure and to multiple tests performed. In fact, although many claims of associations have been published, the statistical support tended to be weak. For that reason we chose a conservative statistic. Another possible interpretation of our negative results could be that they showed a tendency to an association between the 5HT1A and 5HT6 genes and MOH. In particular, our data could indicate a tendency towards a protective effect of the G allele of the 5HT1A gene versus addiction in migraine patients, and an overrepresentation of allele C compared of allele T of the 5HT6 gene in MOH group. However, the statistical significance disappeared after correction for multiple comparisons. If such associations were nonetheless true, our results could be useful for future meta-analyses that could overcome the problem of a low statistical power. Finally, we belive that the putative pathogenetic and therapeutic relevance of the serotoninergic system in MOH deserves confirmation in other studies on other genes involved in the serotonin metabolism.
References
Diener HC, Limmroth V (2004) Medication-overuse headache: a worldwide problem. Lancet Neurol 3:475–483, 10.1016/S1474-4422(04)00824-5, 15261608
Calabresi P, Cupini ML (2005) Medication-overuse headache: similarities with drug addiction. Trends Pharmacol Sci 26:62–68, 10.1016/j.tips.2004.12.008, 1:CAS:528:DC%2BD2MXoslahtQ%3D%3D, 15681022
Goldman D, Oroszi G, Ducci F (2005) The genetics of addictions: uncovering the genes. Nat Rev Genet 6:521–532, 10.1038/nrg1635, 1:CAS:528:DC%2BD2MXlslWgurc%3D, 15995696
Russell MB, Ostergaard S, Bendtsen L, Olesen J (1999) Familial occurrence of chronic tension-type headache. Cephalalgia 19:207–210, 10.1046/j.1468-2982.1999.019004207.x, 1:STN:280:DyaK1MzgsVCmsA%3D%3D, 10376164
Cevoli S, Sancisi E, Grimaldi D, Pierangeli G, Zanigni S, Nicodemo M, Cortelli P, Montagna P (2009) Family history for chronic headache and drug overuse as a risk factor for headache chronification. Headache 49:412–418, 10.1111/j.1526-4610.2008.01257.x, 19267785
Kotani K, Shimomura T, Shimomura F, Ikawa S, Nanba E (2002) A polymorphism in the serotonin transporter gene regulatory region and frequency of migraine attacks. Headache 42:893–895, 10.1046/j.1526-4610.2002.02209.x, 12390616
Park JW, Kim JS, Kim YI, Lee KS (2005) Serotonergic activity contributes to analgesic overuse in chronic tension-type headache. Headache 45:1229–1235, 10.1111/j.1526-4610.2005.00247.x, 16178954
Headache Classification Committee, Olesen J, Bousser M-G, Diener H-C et al (2006) New appendix criteria open for a broader concept of chronic migraine. Cephalalgia 26:742–746, 10.1111/j.1468-2982.2006.01172.x, 1:STN:280:DC%2BD283mt1Gruw%3D%3D, 16686915
Yilmaz M, Erdal ME, Herken H, Cataloluk O, Barlas O, Bayazit YA (2001) Significance of serotonin transporter gene polymorphism in migraine. J Neurol Sci 186:27–30, 10.1016/S0022-510X(01)00491-9, 1:CAS:528:DC%2BD3MXksVGlt78%3D, 11412868
Serretti A, Lilli R, Lorenzi C, Lattuada E, Smeraldi E (2000) Serotonin-2C and serotonin-1A receptor genes are not associated with psychotic symptomatology of mood disorders. Am J Med Genet 96:161–166, 10.1002/(SICI)1096-8628(20000403)96:2<161::AID-AJMG7>3.0.CO;2-9, 1:STN:280:DC%2BD3cvitlynsw%3D%3D, 10893489
Erdal ME, Herken H, Yilmaz M, Bayazit YA (2001) Association of the T102C polymorphism of 5-HT2A receptor gene with aura in migraine. J Neurol Sci 188:99–101, 10.1016/S0022-510X(01)00556-1, 1:CAS:528:DC%2BD3MXls1ejurs%3D, 11489292
Nöthen ErdmannJ, Shimron-Abarbanell D, Proppin P (1994) Identification of genetic variation in the human serotonin 1D receptor gene. Biochem Biophys Res Commun 205:1194–1200, 10.1006/bbrc.1994.2792, 7802650
Vogt D, Shimron-Abarbanell H, Neidt J, Erdmann S, Cichon TG, Schulze DJ, Muller W, Maier M, Albus M, Borrmann-Hassenbach M, Knapp M, Rietschel P, Propping MM (2000) Nothen. Investigation of the human serotonin 6 (5-HT6) receptor gene in bipolar affective disorder and schizophrenia. Am J Med Genet 96:217–221, 10.1002/(SICI)1096-8628(20000403)96:2<217::AID-AJMG17>3.0.CO;2-0, 1:STN:280:DC%2BD3cvitlymsw%3D%3D, 10893499
Mochi M, Cevoli S, Cortelli P, Pierangeli G, Soriani S, Scapoli C, Montagna P (2003) A genetic association study of migraine with dopamine receptor 4, dopamine transporter and dopamine-beta-hydroxylase genes. Neurol Sci 23:301–305, 10.1007/s100720300005, 1:STN:280:DC%2BD3s7htFWqtQ%3D%3D, 12624717
Cevoli S, Mochi M, Scapoli C, Marzocchi N, Pierangeli G, Pini LA, Cortelli P, Montagna P (2006) A genetic association study of dopamine metabolism-related genes and chronic headache with drug abuse. Eur J Neurol 13:1009–1013, 10.1111/j.1468-1331.2006.01415.x, 1:STN:280:DC%2BD28rgs1OhtA%3D%3D, 16930369
Monari L, Mochi M, Valentino ML, Arnaldi C, Cortelli P, De Monte A, Pierangeli G, Prologo G, Scapoli C, Soriani S, Montagna P (1997) Searching for migraine gene: exclusion of 290 cM out of the whole human genome. Ital J Neurol Sci 18:277–282, 10.1007/BF02083304, 1:STN:280:DyaK1c%2FnsVegsw%3D%3D, 9412851
Montagna P (2008) The primary headaches: genetics, epigenetics and a behavioural genetic model. J Headache Pain 9:57–69, 10.1007/s10194-008-0026-x, 18345478
Ogilvie AD, Russell MB, Dhall P, Battersby S, Ulrich V, Smith CA, Goodwin GM, Harmar AJ, Olesen J (1998) Altered allelic distributions of the serotonin transporter gene in migraine without aura and migraine with aura. Cephalalgia 18:23–26, 10.1046/j.1468-2982.1998.1801023.x, 1:STN:280:DyaK1c3mtl2htA%3D%3D, 9601620
Park JW, Han SR, Yang DW, Kim YI, Lee KS (2006) Serotonin transporter protein polymorphism and harm avoidance personality in migraine without aura. Headache 46:991–996, 10.1111/j.1526-4610.2006.00439.x, 16732845
Ebstein RP (2006) The molecular genetic architecture of human personality: beyond self-report questionnaires. Mol Psychiatry 11:427–445, 10.1038/sj.mp.4001814, 1:CAS:528:DC%2BD28XjslKks74%3D, 16534505
Acknowledgments
The authors thank Dr Mirella Mochi for her scientific support and Ms Sabrina Farnè for technical assistance.
Conflict of interest statement
No conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License ( https://creativecommons.org/licenses/by-nc/2.0 ), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Cevoli, S., Marzocchi, N., Capellari, S. et al. Lack of association between five serotonin metabolism-related genes and medication overuse headache. J Headache Pain 11, 53–58 (2010). https://doi.org/10.1007/s10194-009-0168-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10194-009-0168-5