Abstract
Calcitonin gene-related peptide (CGRP) is known to increase during acute attack of migraine and tension type headache (TTH). However, its concentration during inter-ictal period is not known. This may help us to understand the pathophysiology of these headaches. The objectives of this study are to find out the concentration of CGRP in plasma during inter-ictal period among migraineurs and TTH and to compare it with control group through cross-sectional study from headache clinic of a tertiary centre. Study sample comprised of three groups: migraineurs, TTH subjects as well as a healthy control group. Fifty subjects in each group were included after screening for the respective inclusion criteria and exclusion criteria. None of the subjects was blood relatives of other subject. Their venous blood was drawn and plasma was separated to be kept at −70°C. CGRP was analysed with commercially available ELISA kit. Data were analysed with the help of SPSS V 11.0 for Windows. Chi-square, independent sample t test and one-way ANOVA with post hoc Tukey and univariate regression were performed. Plasma CGRP concentration was not different among three diagnostic groups (F = 0.78; P = 0.49). Similarly, plasma CGRP concentration was not different among episodic TTH and chronic TTH groups (t = 0.32; P = 0.97) and comparison of episodic and chronic migraine groups also revealed similar results in this study (1.14 vs. 0.94 ng/ml; P = 0.23). The presence of aura did not affect the inter-ictal CGRP levels among migraineurs (F = 0.16; P = 0.85). In conclusion, this study suggests that migraine and TTH could be episodic disorders and subjects have comparable CGRP levels during inter-ictal period.
Similar content being viewed by others
Introduction
Calcitonin gene-related peptide (CGRP) is located in the trigeminal nuclei and it is released during headache in the circulation [1, 2]. A number of studies had considered CGRP to be central in the pathogenesis of migraine as well as tension type headache (TTH) [3–6].
Its role in migraine is suggested by five kind of evidences: (a) higher level of plasma CGRP during spontaneous headache as compared to controls [7]; (b) increment in plasma CGRP level during experimental migraine attacks [8]; (c) lowering of plasma CGRP level with anti-migraine drugs [9]; (d) reports describing the relief in migraine with CGRP antagonists [10, 11]; and (e) initiation of migraine among migraineurs after human alpha CGRP infusion [12]. Some studies tried to correlate the clinical symptoms of migraine with plasma CGRP level and found that its level correlates with the intensity and duration of headache and touches the base-line after an attack is over [7, 13]. Thus, these studies suggest that migraine is essentially an episodic disorder. However, electrophysiological data suggest that brain remains hyper-excitable even in between the migraine episodes and it predisposes a person to have migraine attacks further [14]. Based on this assumption, some studies assessed plasma CGRP level in between episodes and came out with the conflicting reports [6, 13, 15–17].
Similar studies in chronic TTH subjects failed to find increase in plasma CGRP levels and only one study suggested that TTH subjects with pulsating pain harbour higher CGRP concentration in plasma during pain [18, 19]. To our knowledge, such studies were never attempted in episodic TTH subjects.
In addition, previous studies included only two groups, i.e., either of the headache and a control group. At least, to best of our knowledge, vis-à-vis comparison of plasma CGRP level between migraine and TTH subjects is not available. As a result, its role in both the conditions cannot be compared directly. Secondly, many of these studies are silent regarding the confounding factors that may affect CGRP levels, e.g., obesity, intake of fatty meal, exercise, etc., in relation to the blood sample collection [20–22].
CGRP antagonists are considered useful for acute attack of migraine only and literature is not available regarding their use in TTH [5]. However, if the CGRP levels remain elevated outside the headache in migraineurs as well as TTH sufferers, it is possible that these drugs may be used for the prophylactic therapy also.
Hence, the present study was planned to assess the plasma level of CGRP outside headache episode in migraineurs as well as TTH subjects and control group after exclusion of all possible confounding factors.
Methods
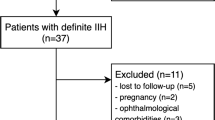
Fifty consecutive subjects suffering from migraine, 50 consecutive subjects of TTH and 50 consecutive controls meeting inclusion criteria were recruited from the headache clinic of a teaching hospital after screening for the exclusion criteria. The study was approved by the institutional ethics committee and informed consent was obtained from all the study subjects. Migraine and TTH were diagnosed according to the International Classification of Headache Disorders (ICHD-2) criteria [23]. The control group consisted of subjects who never had recurrent primary headaches and in whom family history was negative for primary headaches. All participants belong to the same ethnic group and had comparable socio-economic status. None of the subjects was genetically related to the other subjects included in the study.
Subjects with any of the following disorders were excluded from the study: major neurological disorders e.g., epilepsy, space occupying lesions, neurodegenerative disorders, substance use disorder (except tobacco), chronic daily headache (undiagnosed or mixed type), other co-morbid headache, taking prophylactic therapy for migraine and TTH for more than three weeks, consuming anti-oxidants or multivitamins for more than three weeks, and co-morbid psychiatric disorder.
Patient’s history of headache was taken in detail, followed by the clinical examination and wherever required, appropriate laboratory investigation to rule out secondary headache. Parallel information was also collected from a reliable family member regarding headaches of the sufferer. All the information were recorded on a semi-structured Performa.
Measurement of CCRP in plasma
Fasting venous blood (3 ml) was collected in a sterile EDTA vacutainer, at least 3 days after the attack of headache and the subjects were made to take rest for at least 2 h before drawing the blood. Sample was immediately centrifuged at 2,000 rpm for 3 min and plasma was transferred to another sterile clean vial to keep at −70°C till further use. CGRP assay was done with the help of Human α-CGRP ELISA kit (Peninsula Labs, LLC). After the test, absorbance was measured at 450 nm with the help of ELISA reader. Resultant readings were plotted against the standard curve to find out concentration of CGRP in each sample (ng/ml).
Statistical analysis
Analysis was done with the help of SPSS V 11.0 for Windows. Chi-square test was used to compare the non-parametric variables. To compare the CGRP levels between two groups, independent sample t test was used. One-way ANOVA with post hoc Tukey, wherever required, was applied to compare the CGRP levels among three groups. Univariate linear regression was used to find out the association between numerical variables.
Results
Three groups were identical with respect to average age (27.66 years among migraineurs; TTH group 27.6 years; control group 25.18 years). Both the headache groups had preponderance of females as compared to control group (82% among migraineurs; 100% in TTH group; 25% in control group; χ2 = 70.59, P < 0.001). Thus, it shows a skewed gender distribution, the reason for which are discussed below. BMI was not different among groups and none of the subjects fell into the category of “obese” (migraine 23.4; TTH 22.7; control 23.9; P > 0.05).
When other illness-related factors were analysed, it was found that migraine and TTH groups did not differ with regards to total duration of illness, duration since the illness has become disabling and duration of individual headache episode. However, migraineurs had less frequent headaches per month (10 vs. 22 episodes of TTH; P < 0.05) but headache took more time to reach the maximal severity among migraineurs (1.36 vs. 0.30 h in TTH patients; P < 0.05). Chronic TTH was present in 56% and chronic migraine in 14% subjects.
Plasma CGRP level was not affected by gender (t = −1.36; P = 0.17) though it was slightly higher among females. Similarly, CGRP level was not different among three diagnostic groups (F = 0.78; P = 0.49) and was minimally affected by age (R2 = 0.03, migraine; R2 = 0.25, TTH; R2 = 0.28, control group; P > 0.05). The CGRP level was comparable among sub-groups of migraineurs (Table 1). Similarly, plasma CGRP concentration was not different among episodic TTH and chronic TTH groups (t = 0.32; P = 0.97) and comparison of episodic and chronic migraine groups also revealed similar results in this study (1.14 vs. 0.94 ng/ml; P = 0.23).
Discussion
First, whether the blood was drawn from jugular vein or ante-cubital vein was a major issue for us. Since, migraine is primarily a cephalic neurovascular disorder, it was expected that CGRP concentration should be higher in the jugular blood than the peripheral blood. Previous studies have suggested that CGRP is increased in the internal as well as external jugular venous blood during headache [7, 18]. Whether the concentration is also increased in the peripheral blood is still debatable. One body of evidence suggests that level of CGRP in the external jugular blood and peripheral blood is significantly different on non-headache days, but not on the headache days in patients [18]. However, another evidence points out that neuropeptide concentration increases in the peripheral blood on the headache days in patients, however, the concentration is comparable between migraineurs and control group on non-headache days [13]. At the same time, another study found that CGRP concentration in external jugular blood was comparable to the concentration in ante-cubital blood not only during the ictal period but also during the inter-ictal period [17]. Thus, in light of conflicting evidences, it is difficult to discern whether CGRP concentration is different between the blood drawn from these two sources. Moreover, jugular blood goes to right atrium of heart and then to the whole body, hence, it was expected that the CGRP would be present in blood collected from the ante-cubital vein. In addition, the antecubital vein is more easily accessible and sample recruitment is convenient if we collect blood from this site instead of puncturing any of the jugular veins. Since the EIA kit used in this study has good sensitivity (range 0–25 ng/ml), we decided to draw the blood sample from ante-cubital vein.
Present study shows that plasma CGRP concentration is not elevated in migraineurs or TTH sufferers as compared to control group during the inter-episodic period. Previous studies regarding plasma CGRP level measured in the inter-episodic period among migraineurs and TTH subjects had shown contradictory results. Where on one hand, Gallai et al. [13] and Tvedskov et al. [17] did not find increased CGRP levels in the plasma during inter-episodic period, on the other hand, Ashina et al. [15] suggested that CGRP level remains elevated in migraineurs outside headache period as compared to controls. During inter-ictal period, the elevated CGRP was reported not only in the blood but also in the saliva of migraineurs [6, 16]. Nitrate induced experimental migraine attacks have shown an increase in the plasma CGRP during headache phase and its normalization with the spontaneous cessation of pain as well as in those patients who responded to the triptan therapy suggesting the causative role of CGRP in migraine [8, 9]. In light of these evidences, the differences in the results could be due to the differences in the subject selection, source of blood sample (cubital vs. jugular as discussed above), timing of blood sample collection after the last headache and other factors that affect CGRP levels. If samples are drawn very early in the attack, CGRP may not be elevated as it reaches to its peak 1.5 h of onset from migraine and normalizes by 6 h [7]. It must also be considered that CGRP is not specific to migraine and as already mentioned, other factors, viz., obesity, intake of fatty meals and amount of exercise may affect the CGRP levels [21, 22]. Almost all these studies are silent regarding these factors. Other possibility is that migraine is truly an episodic disorder, since blood flow studies suggest normal cerebral blood flow outside migraine episodes and CGRP concentration in plasma falls to normal after spontaneous as well as triptan induced termination of migraine attacks [8, 9, 24]. Comparable concentration of CGRP in chronic migraineurs in the present study further confirms this notion.
Whether CGRP is involved in the pathophysiology of TTH is still an enigma. Glyceryltrinitrate is known to induce TTH in CTTH sufferers upon infusion [25]. This GTN may cause increase in the CGRP levels in TTH patients similar to migraineurs [26]. Moreover, NOS inhibitors are known to prevent the GTN induced TTH in these patients [27]. Still, some studies failed to find increased CGRP levels in the plasma of the CTTH patients upon GTN infusion [3]. Ashina et al. [18] reported that plasma CGRP level in TTH subjects is comparable to that of controls and is independent of headache state. Hence, it appears that CGRP has a role in TTH and it interacts with nitrate or nitric oxide. But, the above statement does not necessitate that CGRP should be increased in peripheral blood in TTH subjects during headache. A number of observations explain why CGRP can be instrumental in TTH despite the fact that its concentration is not increased in peripheral blood. First, CGRP is present not only in the peripheral endings of trigeminal nerves close to dural vessels but also in the trigeminal nucleus itself [28–30]. Here, they are co-localized with the 5HT1D receptor, and CGRP may be instrumental in the central sensitization [30]. Second, CGRP receptors are found in the dural vascular smooth muscles as well as in the trigeminal ganglia. In the trigeminal nucleus, they are found on the satellite glial cells, where their activation induces the iNOS and consequently NO release. This, in turn, initiates inflammatory reaction in the ganglia that is responsible for central sensitization [1]. Third, after peripheral stimulation of the trigeminal nerve, the surrounding glia and trigeminal ganglion cells communicate through gap junctions. This opening of gap junction is not time bound and they either increase in number or remain opened for a long time after the stimulation of trigeminal nerve. Activation of any branch of trigeminal nerves increases SB100 and p53 not only in the cell body of respective fibres but also in the other two branches through paracrine communication. This can also induce sensitization. Here, it must be noted that central sensitization may be the underlying factor in development of chronic TTH [31]. In addition, CGRP differentially regulates the secretion of cytokines in trigeminal nerve which may be responsible for other symptoms associated with headache [2, 30]. In short, these arguments suggest that neuropeptide may be pathophysiologically important even when its concentration in peripheral blood is not increased. Considering all this, serum CGRP concentration may not be elevated in TTH no matter if it is episodic or chronic or, possibly like migraine, TTH could also be an episodic disorder.
Another important finding was the absence of difference between chronic TTH and episodic TTH subjects. This could be due to small sample size and further reduction when the sample was divided into chronic TTH and episodic TTH groups. Hence, type II errors could not be excluded. In addition, whether episodic TTH shares pathophysiological underpinnings with chronic TTH is yet to be discovered and literature show contradictory findings. Mazzotta et al. [32] found lower pain perception threshold in episodic TTH patients as compared to control group whilst Jensen et al. [33] reported that pain perception threshold does not differ between episodic and chronic TTH patients. To compound the situation, reviews available on this subject favour the occurrence of central sensitization in CTTH with peri-cranial tenderness whilst questioning its importance during episodic TTH [30–34]. Similarly, it is yet to be investigated if CGRP secretion and its plasma concentration are related to central sensitization. Such a study can throw more light on this issue as well as explain the conflicting results found in various studies. Results of the present study suggest that CGRP concentration is not elevated during inter-episodic period among migraineurs and TTH subjects questioning the utility of CGRP antagonists as prophylactic agents as we have proposed earlier.
The strength of the present study lies in the strict exclusion criteria. All the subjects included in this study were not having any other illness or other confounding factors as already discussed. Hence, the results of this study show the findings that represent the migraine and TTH exclusively. Second, most of the studies in the past followed clinical criteria for diagnosis of migraine and TTH which lead to inclusion of non-identical subjects. We followed the ICHD-2 criteria for diagnosis of migraine and TTH; hence, the selection bias could be excluded.
However, this study also had some methodological limitations. First, strict inclusion criteria in this study preclude from generalizing the results as subjects with such isolated illness are not very common in the clinics. Hence, results must be applied with caution in the general population. Second, sample size of the study was small relative to the prevalence of the illnesses in question owing to few technical factors. We suggest inclusion of a larger sample in the future studies. Third, the results of the study represent only cross-sectional examination during a specified period of illness. In future, sequential measurement may be made at different phases of the illness to elucidate the underlying pathophysiology in all groups included in this study. Fourth, the gender distribution was skewed and the study sample had preponderance of female gender. This could be due to two reasons: one, the migraine as well as TTH is more prevalent in females [35] and secondly, the illness included in the exclusion criteria is relatively less prevalent in females. Fifth, the female hormones may also affect the CGRP expression in dorsal root ganglia and pregnancy may influence the plasma CGRP level [36, 37]. However, whether the normal cycle affects the CGRP concentration is not known. We did not take into account this issue whilst recruitment and it could also have affected the results of study.
In essence, this study suggests that migraine and TTH are episodic disorders. Both may be pathophysiologically overlapping conditions, but further studies are required to throw more light on this issue.
References
Li J, Vause CV, Durham PL (2008) Calcitonin gene-related peptide stimulation of nitric oxide synthesis and release from trigeminal ganglion glial cells. Brain Res 1196:22–32
Thalakoti S, Patil VV, Damodaram S, Vause CV, Langford LE, Freeman SE, Durham PL (2007) Neuron-glia signaling in trigeminal ganglion: implications for migraine pathology. Headache 47:1008–1023
Ashina M, Bendtsen L, Jensen R, Sakai F, Olesen J (2000) Possible mechanisms of glyceryl-trinitrate-induced immediate headache in patients with chronic tension-type headache. Cephalalgia 20:919–924
Doods H, Arndt K, Rudolf K, Just S (2007) CGRP antagonists: unravelling the role of CGRP in migraine. Trends Pharmacol Sci 28:580–587
Edvinsson L (2007) Novel migraine therapy with calcitonin gene-regulated peptide receptor antagonists. Expert Opin Ther Targets 11:1179–1188
Fusayasu E, Kowa H, Takeshima T, Nakaso K, Nakashima K (2007) Increased plasma substance P and CGRP levels, and high ACE activity in migraineurs during headache-free periods. Pain 128:209–214
Sarchielli P, Alberti A, Codini M, Floridi A, Gallai V (2000) Nitric oxide metabolites, prostaglandins and trigeminal vasoactive peptides in internal jugular vein blood during spontaneous migraine attacks. Cephalalgia 20:907–918
Juhasz G, Zsombok T, Modos EA, Olajos S, Jakab B, Nemeth J et al (2003) NO-induced migraine attack: strong increase in plasma calcitonin gene-related peptide (CGRP) concentration and negative correlation with platelet serotonin release. Pain 106:461–470
Juhasz G, Zsombok T, Jakab B, Nemeth J, Szolcsanyi J, Bagdy G (2005) Sumatriptan causes parallel decrease in plasma calcitonin gene-related peptide (CGRP) concentration and migraine headache during nitroglycerin induced migraine attack. Cephalalgia 25:179–183
Olesen J, Diener HC, Husstedt IW, Goadsby PJ, Hall D, Meier U et al (2004) Calcitonin gene-related peptide receptor antagonist BIBN 4096 BS for the acute treatment of migraine. N Engl J Med 350:1073–1075
Petersen KA, Lassen LH, Birk S, Lesko L, Olesen J (2005) BIBN4096BS antagonizes human alpha calcitonin gene related peptide-induced headache and extracerebral artery dilatation. Clin Pharmacol Ther 77:202–213
Lassen LH, Haderslev PA, Jacobsen VB, Iversen HK, Sperling B, Olesen J (2002) CGRP may play a causative role in migraine. Cephalalgia 22:54–61
Gallai V, Sarchielli P, Floridi A, Franceschini M, Codini M, Glioti G et al (1995) Vasoactive peptide levels in the plasma of young migraine patients with and without aura assessed both interictally and ictally. Cephalalgia 15:384–390
Coppola G, Pierelli F, Schoenen J (2007) Is the cerebral cortex hyperexcitable or hyperresponsive in migraine? Cephalalgia 27:1427–1439
Ashina M, Bendtsen L, Jensen R, Schifter S, Olesen J (2000) Evidence for increased plasma levels of calcitonin gene-related peptide in migraine outside of attacks. Pain 86:133–138
Bellamy JL, Cady RK, Durham PL (2006) Salivary levels of CGRP and VIP in rhinosinusitis and migraine patients. Headache 46:24–33
Tvedskov JF, Lipka K, Ashina M, Iversen HK, Schifter S, Olesen J (2005) No increase of calcitonin gene-related peptide in jugular blood during migraine. Ann Neurol 58:561–568
Ashina M, Bendtsen L, Jensen R, Schifter S, Jansen-Olesen I, Olesen J (2000) Plasma levels of calcitonin gene-related peptide in chronic tension-type headache. Neurology 55:1335–1340
Ashina M (2002) Calcitonin gene-related peptide in tension-type headache. Sci World J 2:1527–1531
Bigal ME, Lipton RB, Holland PR, Goadsby PJ (2007) Obesity, migraine, and chronic migraine: possible mechanisms of interaction. Neurology 68:1851–1861
Zelissen PM, Koppeschaar HP, Lips CJ, Hackeng WH (1991) Calcitonin gene-related peptide in human obesity. Peptides 12:861–863
Lind H, Brudin L, Lindholm L, Edvinsson L (1996) Different levels of sensory neuropeptides (calcitonin gene-related peptide and substance P) during and after exercise in man. Clin Physiol 16:73–82
Headache Classification Subcommittee of the International Headache Society (2004) The International Classification of Headache Disorders. Cephalalgia 24(Suppl 1):1–151
Bartolini M, Baruffaldi R, Paolino I, Silvestrini M (2005) Cerebral blood flow changes in the different phases of migraine. Funct Neurol 20:209–211
Ashina M, Bendtsen L, Jensen R, Olesen J (2000) Nitric oxide induced headache in patients with chronic tension-type headache. Brain 123:1830–1837
Akerman S, Williamson DJ, Kaube H, Goadsby PJ (2002) Nitric oxide synthase inhibitors can antagonize neurogenic and calcitonin gene-related peptide induced dilation of dural meningeal vessels. Br J Pharmacol 137:62–68
Ashina M, Lassen LH, Bendtsen L, Jensen R, Olesen J (1999) Effect of inhibition of nitric oxide synthase on chronic tension- type headache: a randomised crossover trial. Lancet 353:287–289
Jansen I, Uddman R, Ekman R, Olesen J, Ottosson A, Edvinsson L (1992) Distribution effects of neuropeptide Y, vasoactive intestinal peptide, substance P and calcitonin gene-related peptide in human middle meningeal arteries: comparison with cerebral and temporal arteries. Peptides 13:527–536
Jansen I, Uddman R, Hocherman M, Ekman R, Jensen K, Olesen J et al (1986) Localization and effects of neuropeptide Y, vasoactive intestinal polypeptide, substance P and calcitonin gene-related peptide in human temporal arteries. Ann Neurol 20:496–501
Smith D, Hill RG, Edvinsson L, Longmore J (2002) An immunocytochemical investigation of human trigeminal nucleus caudalis: CGRP, substance P and 5-HT1D-receptor immunoreactivities are expressed by trigeminal sensory fibers. Cephalalgia 22:424–431
Ashina M (2004) Neurobiology of chronic tension-type headache. Cephalalgia 24:161–172
Mazzotta G, Sarchielli P, Gaggioli A, Gallai V (1997) Study of pressure pain and cellular concentration of neurotransmitters related to nociception in episodic tension type headache patients. Headache 37:565–571
Jensen R, Rasmussen BK, Pedersen B, Olesen J (1993) Muscle tenderness and pressure pain thresholds in headache. A population study. Pain 52:193–199
Bendtsen L (2000) Central sensitization in tension type headache—possible pathophysiological mechanisms. Cephalalgia 20:486–508
Lance JW, Goadsby PJ (2005) Mechanism and management of headache. Elsevier, Philadelphia
Gangula PR, Lanlua P, Wimalawansa S, Supowit S, DiPette D, Yallampalli C (2000) Regulation of calcitonin gene-related peptide expression in dorsal root ganglia of rats by female sex steroid hormones. Biol Reprod 62:1033–1039
Stevenson JC, MacDonald DWR, Warren RC (1986) Increased concentration of calcitonin gene-related peptide during normal human pregnancy. Br Med J 293:1329–1330
Acknowledgments
We are thankful to the Zydus Cadila for helping us in procurement of kits and chemicals used in this study.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License ( https://creativecommons.org/licenses/by-nc/2.0 ), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Gupta, R., Ahmed, T., Banerjee, B. et al. Plasma calcitonin gene-related peptide concentration is comparable to control group among migraineurs and tension type headache subjects during inter-ictal period. J Headache Pain 10, 161–166 (2009). https://doi.org/10.1007/s10194-009-0110-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10194-009-0110-x