Abstract
This study investigates the importance of alcohol as a migraine trigger factor, the prevalence of alcohol consumers and the mechanism of headache provocation. A MEDLINE search from 1988 to October 2007 was performed for “headache and alcohol”, “headache and wine”, “migraine and alcohol” and “migraine and wine”. In retrospective studies, about one-third of the migraine patients reported alcohol as a migraine trigger, at least occasionally, but only 10% of the migraine patients reported alcohol as a migraine trigger frequently. Regional differences were reported, perhaps depending in part on alcohol habits. No differences were found between migraine and tension headache and different genders. However, prospective studies limit considerably the importance of alcohol as a trigger. Recent studies show that migraine patients consume less alcohol than controls. Red wine was reported to be the principal trigger of migraine, but other studies show that white wine or other drinks are more involved. Then, the discussion based on the different composition of the various alcoholic beverages, in order to discover the content of alcoholic drinks responsible for migraine attack, reflects this uncertainty. Biogenic amines, sulphites, flavonoid phenols, 5-hydroxytryptamine mechanisms and vasodilating effects are discussed. The fact that few headache patients cannot tolerate some alcoholic drinks does not justify the consideration that alcohol is a major trigger and the suggestion of abstinence. In fact, low doses of alcohol can have a beneficial effect on patients such as migraineurs, who were reported to have an increased risk of cardiovascular disease.
Similar content being viewed by others
Introduction
It is known since antiquity that wine could be a trigger for migraine. Perhaps the earliest reference to alcohol-provoked migraine can be found in the work of Celsus (25 B.C.–50 A.D.) who wrote “the pain… is contracted….by drinking wine” and more than six centuries later Paul of Aegina (625–690 A.D.) also included drinking of wine as the triggering factor of migraine [1].
The concept of dietary migraine (migraine provoked by some foods such as cheese, chocolate, citrus fruit, alcoholic beverages) has been with us for more than 200 years, since Fothergill’s first description in 1778 [1,2]. However, despite the original paper of Hanington [3] and the vigorous literature that follows, serious doubts exist as to whether the condition really exists as a clinical entity. The commonest initiator of an attack is alcoholic beverages and by far the largest and most notorious is red wine, at least in the United Kingdom [4], while in other countries, white wine (France, Italy) and champagne (France) are viewed as the major culprits [5, 6].
In the classification of the International Headache Society (IHS), two types of alcohol-induced headache were reported in secondary headaches (code 8.1.4): the immediate alcohol-induced headache, which develops within 3 h after ingestion of alcoholic beverages, and the delayed alcohol-induced headache (previously termed hangover headache), which develops after the blood alcohol level declines or reduces to zero [7]. In the comment, it was stated that few subjects develop the former type of headache, while the alcohol-delayed headache is one of the commonest type of headache, the day after alcohol consumption, provoked by ingestion of modest amount of alcoholic beverages in migraine sufferers, while non-migraineurs usually need a higher intake. The same classification stated that migraine could be aggravated (long term increase) by frequent intake of alcoholic beverages.
Generally, the studies on alcohol-induced headache have not carried out the distinction between the immediate and delayed alcohol-induced headache, which in migraine patients can be partially artificial and difficult to perform [8]. Some studies report that alcohol provokes headache within 30 min to 3 h; principally the red wine [9–11]. Others consider an evaluation period of 6 [12] or 24 h [13], while some affirm that headaches appear frequently the next morning/day [10, 14].
In fact migraine patients can have headaches triggered by alcoholic drinks such as wine within a few hours or the next morning after the alcohol intake (hangover headache?), with the confounding effect of sleep on the interval determination.
This review concerns the studies on alcohol as a headache trigger after the 1988 IHS classification, prevalence of alcohol consumers in headache sufferers, and will discuss if alcohol, per se, or some components of alcoholic drinks were responsible for headache precipitation.
Alcohol as a trigger factor
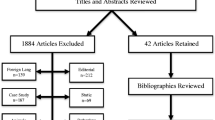
Many studies in different countries show that alcohol is a headache trigger in high percentage of migraine subjects, both in the general population [15–17] and headache clinic population [18–22]. About one-third of the patients (mean 34%) report alcohol as a trigger (Fig. 1). However these are retrospective studies, and until recently only a prospective study based exclusively on the subjective patients information exists [23]. Recent studies show that alcohol acts as a trigger at least occasionally in a percentage similar to that of the previous studies (37%), but as a frequent/consistent trigger in only 10% of the patients [22,24]. Curiously, in some countries, the percentages of alcohol or wine as migraine triggers were negligible, 6.1 [25] and 1.4% [26], perhaps depending on the degree of alcohol habits.
In many studies, no substantial differences between migraines with and without aura were described [22, 27, 28], even so both higher susceptibility to red wine [17], and a lower percentage of alcohol sensitivity in migraine with aura was reported [25, 26]. No differences exist between male and females [17, 22,27–29] in alcohol susceptibility.
No differences exist between migraine and tension headache in the frequency of alcohol as a trigger [17, 18, 20, 24–26, 29] (Table 1). Other studies show that only migraineurs had episodes of tension-type headache precipitated by alcohol [19,27].
Recently, a prospective study examining a wide spectrum of factors related to migraine, by applying a sophisticated statistical analysis, provides evidence for the limited importance of nutrition (comprising alcoholic beverages) in the precipitation of migraine [30], in contrast to a previous report of the same study group [24]. This work considered the alcoholic drinks and other triggering factors taken the day before onset of headache.
Moreover, there were significant trends of decreasing prevalence of migraine and non-migraine headache with the increasing number of alcohol units consumed [28, 31].
In conclusion, no significant association between alcohol consumption with migraine and tension headache was found in many studies [26, 28–30]. It is worth noting, however, that alcohol may precipitate individual attacks of migraine and tension-type headache; thus the lack of association may also be explained by change in the habits after experience of these factors provoking attacks, that is headache sufferers could tend to avoid alcohol in order to not aggravate their headache.
Alcohol consumption in headache patients
Since alcohol can trigger migraine and tension headache attack, only a low percentage of headache patients should drink alcoholic beverages. Few and often only descriptive studies exist on this topic, with marked differences in the percentage of consumers perhaps depending on the country habits [19, 24, 26, 31–33] (Table 2). No differences between migraine and tension headache were reported [24, 26] (Table 1).
A study performed in 1988 [34] on 100 Tuscan females with migraine without aura (age range 18–54, mean 34.3) show that 58% did not consume alcohol in the 3 months preceding the visit, 38% are regular consumers (at least once a week) and 4% occasional consumers (at least once in the period but less than once a week). In females with migraine, there was a significantly higher percentage of nonconsumers of alcohol than that reported in national studies on the population, using the same parameters, in females of the same region [35] (Fig. 2). Of the 58 nonconsumer patients, 16 were abstainers but the others have consumed some type of alcoholic drinks during their life without the development of headache. In this study, six subjects of the consumer group identified white wine as a trigger, while two subjects reported red wine and two both the types of wine in the nonconsumer group (Table 3).
Percentage of alcohol abstainers in women of general population and in female migraine patients. *P < 0.01 versus migraine females (95 or 99% confidence interval for a population proportion). In the Tuscan women of age range similar to that of migraine patients (15–54 years), the percentage of nonconsumers was even less (17–23%)
This study is in accordance with a larger population-based study performed to detect cardiovascular risk factor in migraine, showing significantly less alcohol consumption in migraine than in control subjects [33].
No differences (but data was not shown) were reported in another population study [31], and in a small study where, however, some bias is present, that is different periods of evaluation, controls with medical illnesses, etc [32].
Is alcohol per se or another component of alcoholic drinks the headache trigger?
In accordance with the previous reports [4, 12, 13], red wine was considered the main cause after the fundamental study of Littlewood et al. [36] showing that 300 ml of red wine and not vodka with an equivalent alcohol content provoked headache in red wine-sensitive-migraine patients and not in nonsensitive migraine-patients or controls. These findings suggest that red wine contains a migraine-provoking agent that is neither alcohol (because vodka is pure alcohol) nor tyramine (for the negligible content in wine). However the blinding of this study is uncertain. Recently another study group reported a high percentage of patients referring red wine as the most frequent trigger between alcoholic drinks [24] but subsequently it did not report any of them as a trigger [30].
Another study shows that of the 429 migraine patients, 17% are sensitive to all forms of alcohol, 11.2% to red wine but not to white wine or clear spirits, while 28% are sensitive to beer (none only to this alone) [19].
However, in other countries (France, Italy) white wine (in France also champagne) is viewed as the major culprit [5, 6]. In addition, another study reported a surprisingly higher correlation of spirits and sparkling wine to migraine attack, compared to other alcoholic drinks. Low doses of alcohol during meals significantly lower the frequency of induced-attacks and the alcoholic consumption during stress was related to higher migraine attack frequency [37]. While some report beer as a trigger [19, 24], others found no association [30, 31, 34, 37].
Wine does not need to be ingested in excessive quantities to produce headache. The interval between drinking red wine and developing headache varied from 30 min to 3 h, and only one or two glasses need to be ingested. Wine contains some ingredients such biogenic amines (histamine, tyramine, phenylethylamine etc), sulphites, phenolic flavonoids that theoretically could provoke headache. The possibility that dietary biogenic amines might cause adverse reactions was initially proposed when it was noticed that foods that caused symptoms in patient taking drugs inhibiting monoamine-oxidase (MAO) were the same as those believed to cause migraine attack in some patients [3]. A good review of the controlled studies on intolerance of dietary biogenic amines was recently performed, showing no evidence for the hypothesis that histamine, tyramine or phenylethylamine can cause food intolerance reactions in susceptible subjects [38].
It is possible that alcohol itself can trigger headache, especially when ingested in large quantities such as in hangover headache, and some components of the alcoholic drinks can reinforce alcohol action or vice versa.
The principal substances of the alcoholic drinks thought to be involved in headache provoked by alcoholic drinks are successively discussed.
Histamine
Jarisch et al. [39] sustained that histamine in wine can induce headache in patients suffering from histamine intolerance, a disease characterized by impaired histamine degradation based on a reduced diamine oxidase activity or a lack of this enzyme. Red wine usually contains up to 20- to 200-fold more histamine than white wine. They analyzed 52 different wines and 17 beers by radioimmunoassay: histamine level ranged from 3 to 120 μg/l in white wine, 21 to 52 μg/l in beer, 15 to 670 μg/l in sparkling wine and champagnes and 60 to 3,800 μg/l in red wine. In the red wine provocation test, 50 μg histamine in 125 ml red wine was sufficient to induce headache in histamine-intolerant patients, but viewing their data, in only 5 out of 28 tested subjects [40].
Histamine intolerance, which results from a disequilibrium of accumulated histamine and the capacity for histamine degradation, has been recently reviewed [41]. This good review reports no major differences in histamine content in the principal drinks (white wine, red wine, beer) and shows that various foods contain much more histamine concentrations, particularly in products of microbial fermentation; therefore histamine is an indicator of hygienic food quality. Many foods are considered to have the capacity to release histamine from tissue mast cells, even if they themselves contain only small amounts of histamine. However, alcohol potently inhibited, in itself, diamine oxidase and may activate the release on histamine from mast cells.
Headache is one of the symptoms of histamine intolerance: the other symptoms such as facial flushing, rhinoconjunctival symptoms, asthma, urticaria, pruritus, hypotension, arrhythmia, and diarrhoea are unlikely to be present in the attacks of migraine induced by wine. In their review on controlled studies, Jansen et al. [38] reported one conclusive negative study on the relation between histamine in red wine and wine intolerance and no conclusive positive results. However, in this review, one study was considered negative because no differences were found between histamine-rich and histamine-poor wine, but both provoked reactions in a very high percentage. The histamine-poor wine challenge contains about 80 μg of histamine, a dose sufficient to induce headache in other studies [40].
In red wine-sensitive patients, there was no difference between histamine antagonists and placebo on headache induced by red wine, and also the level of plasma diamine-oxidase was no different between red wine sensitive and nonsensitive migraine patients [42].
Intravenous histamine infusion (0.16–0.66 μg/Kg/min for 20 min) provokes headache in migraine and tension headache patients but not in controls; moreover 0.5 μg/Kg/min for 20 min (which provokes a plasma concentration of approximately 50 nM), provokes headache in migraine patients which can rapidly disappear in most patients, but some patients continued to have or developed headaches for 1–12 h after the infusion (delayed headache) at a mean time of 5 h after the infusion. In most patients with delayed headache and also sometimes with immediate headache, the headache fulfilled IHS diagnostic criteria for migraine [43, 44].
In conclusion, histamine can certainly provoke migraine, but it is not certain if it is the factor responsible for headache induced by alcoholic drinks.
Tyramine
The relation between tyramine and migraine has been studied most extensively. Half were pioneering studies performed by Hanington et al. (see [37]) which showed that oral tyramine provoked headaches in dietary migraine patients but not in nondietary migraine or controls. However, two conclusive negative studies were found on the relation between oral tyramine and headache attack in dietary and nondietary migraine. No conclusive positive studies were found [37].
The tyramine content of both the red and white wine was negligible 1–2 mg/L (9) in comparison with the tyramine doses utilized in oral challenge studies (100–200 mg).
Phenylethylamine
In contrast to previous studies that have suggested that chocolate, which is rich of phenylethylamine, provoked migraine in chocolate-sensitive patients, Marcus et al. [45] performing the same study in a large migraine and tension headache sample produced conclusive negative results.
However, contrary to previous views, chocolate has a low concentration of tyramine and phenylethylamine, while it is rich in flavonoid phenols [1].
Flavonoid phenols
Phenols are the substrate for the enzyme phenolsulphotransferase (PST), which exists in two forms and is particularly active in the gut: PST-M, which inactivates phenolic monoamines such as tyramine and dopamine, and PST-P, which degrades phenol itself and p-cresol. Ethyl acetate extracts of red wine contained very potent inhibitors of PST, particularly the P form, but also white wine and other drinks (spirits and vodka) show some degree of this activity [46]. The main difference between red and white wine is their flavonoid component: red wine contains typically 1,200 mg/l, while white wine only 50 mg/l. This fraction inhibits potently and specifically PST-P, at a dilution consistent with a consumption in vivo of a single glass. Catechins and anthocyanins (responsible for the color of red wine), which comprise about 30% of flavonoid fraction and are absorbed through the gastrointestinal tract, are potent inhibitors of PST-P in vitro. To study if red wine also has this metabolic effect in vivo, p-cresol that is a specific substrate of PST-P was determined in urine after the oral challenge with red wine, vodka or water: p-cresol increased significantly after red wine with respect to controls. This suggests the possibility that red wine inhibition of conjugation by PST-P of p-cresol and other phenols could result in a build up of free phenols in the circulation, which may be toxic in several ways [9]. In dietary migraine, a deficit of PST-P was identified [47]. Other studies show that in migraine patients, the activity of PST-M responsible for inactivation of dopamine and 5HT was reduced, but not that of PST-P, without any significant difference in dietary migraine. Moreover, the selective inhibition of PST-P by red wine is much more potent than previously thought, with 2,000-fold dilution of dealcoholized red wine having the ability to inhibit sulphation by this enzyme by 50% [48]. Phenol flavonoids were contained in beer [49] and also in the chocolate, which impair endothelial function [50].
Sulphites
Sulphites have not been shown convincingly to lead to headache in individuals with sulphite sensitivity. Sulphites are considered to be the cause of red wine intolerance, particularly asthma [51]. Nevertheless, other studies have confirmed the sensitivity to the sulphites in wine in limited number of individuals, and in wine-sensitive asthmatic subjects there was no major role for sulphite additives in inducing asthmatic response [52,53].
It must be stressed that red wine contains much less sulphite than white wine.
Sulphites could trigger headache through the release of histamine, as they cause symptoms only during a period of enhanced histamine sensitivity [51].
On the other hand, there are many foods such as dried fruits, chips, raisins, soy sauce, pickles and juice fruits containing concentration of sulphites even ten times higher than that of wine.
Action on 5-hydroxytryptamine (5-HT)
Red wine diluted 1:20 is a powerful releaser of 5-HT from platelet and this property varied widely among different types of wine and even in the sample of the same type: the releasing ability lies mainly in two flavonoid fractions with molecular weight greater than 500 Da [47,54]. Neither white wine nor beer had any releasing effect [55]. No significant differences in platelet 5-HT release were found in red-wine sensitive migraine patients, migraine patients not sensitive to red wine and controls [56]. Moreover, there were no differences between red wine Chianti (a potent 5-HT releaser) and Valpolicella (poor releaser) in inducing headache [42], but Valpolicella sample proved to have relatively high releasing properties with respect to earlier experiments [47]. Red wine, but not white wine, causes an increase of whole blood 5-HT levels in controls, probably caused by flavonoid fraction [57]. However, white wine and champagne were shown to increase 5-HT in subjects with low basal 5-HT level and to decrease 5-HT in those with higher basal 5-HT levels: these variations appear to depend on the alcoholic content of the beverage [58]. Other interesting pharmacological properties of wine are the inhibition of 5-HT and noradrenaline reuptake and MAO activity through its polyphenolic component resveratrol [59] and an action on 5-HT receptors.
Red wine strongly inhibits the binding of 5-HT to 5-HT1 receptors; white wine possesses this ability to a much lesser extent [47]. Studies on red wine-sensitive subjects, in order to show a mediation of induced headache by some types of 5-HT2 receptors, give inconclusive results [42]. In this light, direct or indirect (by 5-HT release) stimulation of 5-HT2 receptors was supposed to be the mechanism of headache induced by some serotonergic agonists ([60], for review).
Therefore, the release of 5-HT possibly from central stores could represent a plausible mechanism for wine induced headache.
In fact, it was also suggested that dural mast cells could promote headache by releasing 5-HT, prostaglandin I and histamine [61].
Vasodilating action
Wine (more red than white) and other grape products have been shown to have an endothelium-dependent vaso-relaxing activity, probably via nitric oxide (NO)-mediated pathway; ethanol and resveratrol cause no relaxation [62]. Alcohol free grape-skin extracts have the same effects [63]. Alcohol-free red wine polyphenol extract increases endothelial NO release [64]. However in vivo studies show that only the ingestion of red wine with alcohol, but not of dealcoholized red wine, provokes arterial dilatation and thus the effect of wine is due to ethanol [65]. Also oral intake of pure alcohol (at a dose corresponding to a two drink equivalent) produces significant vasodilatation in man [66].
Histamine is known to liberate NO from endothelium, and it was suggested that the release of NO from cerebral blood vessels, perivascular nerve endings or from brain tissue is an important molecular trigger of spontaneous headache pain [67].
Recently, it was shown that ethanol, at low concentrations not dissimilar from those found in blood following low to moderate consumption of alcoholic beverages, releases calcitonin gene-related peptide (and also tachykinins), one of the most vasodilating agents ever found in man, from periarterial sensory nerve ending of arteries leading neurogenic vasodilatation [68].
Conclusion
Various retrospective studies show that a high percentage (about one-third) of migraine patients refer alcohol as a trigger factor. However, this factor is frequently reported at about 10%, which is a percentage more plausible. No significant differences appeared between the migraines with or without aura and between migraine and tension headache. Some studies on the alcohol habits in migraine patients show a low percentage of drinkers in migraine patients. This was supposed to be due to previous experiences of alcohol as headache trigger, but one study does not agree [34]. Certainly, if a less alcohol preference in migraine patients will be confirmed in large controlled studies, it merits a correlation with 5-HT system, which is involved in migraine pathogenesis in some way. In fact, an inverse relationship between density and metabolic functioning of regional brain 5-HT system and alcohol preference was repeatedly reported in animal studies [69–72].
Studies concerning red wine as a principal trigger of migraine in susceptible migraine patients, has led others to perform various studies to identify a substance contained in red wine, but not in other alcoholic drinks. However, other studies report that white wine is more frequently a migraine trigger, and some others, sparkling wine and spirits. Therefore, all the discussions based on the different composition of various alcoholic beverages are inconclusive (Table 4). Experiments with wine are extremely difficult to undertake. The wine composition is affected by many variables: bio-climatic, oenological methods, stabilizing process, ageing, cultivar etc. Therefore a major objective is to perform a study in order to show if it is alcohol per se which provokes migraine and tension headache in susceptible and nonsusceptible migraine patients.
The role of dietary triggers has been well reviewed previously [1, 2]. In the conclusion of their review, in agreement with other expert authors such as Lance, Clifford Rose [1] stated that he had little doubt that red wine will trigger migraine attack in sensitive patients and that all forms of alcohol can provoke headache. Other dietary triggers have negligible importance. Some studies show that patients in whom alcohol or wine/beer acts as a trigger factor also had significantly more other foods as a trigger [19,73]. Certainly, some headache patients cannot tolerate some alcoholic drinks, although not frequently, and perhaps only in combination in the presence of other trigger factors (stress, for example). However, a few negative experiences cannot justify the media and scientific information on alcohol as a major headache trigger and the suggestion of abstinence. In fact, to deny the beneficial effect of a low dose of alcohol in a wide number of people, who can also have a higher risk of cardiovascular disease like migraine patients [74, 75], is not medically appropriate.
References
Clifford Rose F (1997) Food and headache. Headache Q 8:319–329
Martin VT, Behbehani MM (2001) Toward a rational understanding of migraine trigger factors. Med Clin North Am 85:911–941, 11480265, 10.1016/S0025-7125(05)70351-5, 1:STN:280:DC%2BD3MvjtlWqtQ%3D%3D
Hanington E (1967) Preliminary report on tyramine headache. BMJ 2:550–551, 10.1136/bmj.2.5551.550
Peatfield RC, Glover V, Littlewood JT, Sandler M, Clifford Rose F (1984) The prevalence of diet-induced migraine. Cephalalgia 4:179–183, 6498931, 10.1046/j.1468-2982.1984.0403179.x, 1:STN:280:DyaL2M%2FkvV2hug%3D%3D
Pradalier A, Weinman S, Launay JM, Baron JF, Dry J (1983) Total IgE, specific IgE and prick-tests against foods in common migraine—a prospective study. Cephalalgia 3:231–234, 6640656, 10.1046/j.1468-2982.1983.0304231.x, 1:STN:280:DyaL2c%2FlsFektw%3D%3D
Relja G, Nider G, Chiodo-Grandi F, Kosica N, Musco G, Negro C (1993) Is red or white wine an important inducing factor in migraine attacks? Cephalalgia 13(suppl 13):129
Headache Classification Committee of the International Headache Society (2004) The international classification of headache disorders. Cephalalgia 24(suppl 1):1–160
Evans RW, Sun C, Lay C (2007) Alcohol hangover headache. Headache 47:277–279, 17300369, 10.1111/j.1526-4610.2006.00694.x
Littlewood JT, Gibb C, Glover V, Hannah P, Sandler M, Davies PTG, Clifford Rose F (1987) Red wine as a migraine trigger. In: Clifford Rose FC (ed) Advances in headache research. John Libbey & Co Ltd, London, pp 123–127
Olesen J (1984) The significance of trigger factors in migraine. In: Clifford Rose F (ed) Progress in migraine research 2. Pitman, London, pp 18–29
Raskin NH (1981) Chemical headaches. Annu Rev Med 32:63–71, 6784668, 10.1146/annurev.me.32.020181.000431, 1:CAS:528:DyaL3MXhsFWitrc%3D
Glover V, Littlewood J, Sandler M, Peatfield R, Petty R, Clifford Rose F (1984) Dietary migraine: looking beyond tyramine. In: Clifford Rose F (ed) Progress in migraine research 2. Pitman, London, pp 113–119
Pryse-Phillips W (1987) Dietary precipitation of vascular headaches. In: Chandra RK (ed) Food allergy. Nutrition Research Education Foundation St John’s, Newfoundland, pp 237–252
Blau JN, Diamond S (1985) Dietary factors in migraine precipitation: the physicians’ view. Headache 25:184–187, 4019177, 10.1111/j.1526-4610.1985.hed2504184.x, 1:STN:280:DyaL2M3mtVKnsw%3D%3D
Russell MB, Rasmussen BK, Fenger K, Olesen J (1996) Migraine without aura and migraine with aura are distinct clinical entities: a study of four hundred and eighty-four male and female migraineurs from the general population. Cephalalgia 16:239–245, 8792035, 10.1046/j.1468-2982.1996.1604239.x, 1:STN:280:DyaK28zosVWgug%3D%3D
Bank J, Marton S (2000) Hungarian migraine epidemiology. Headache 40:164–169, 10759917, 10.1046/j.1526-4610.2000.00023.x, 1:STN:280:DC%2BD3cvivVansg%3D%3D
Zivadinov R, Willheim K, Sepic-Grahovac D, Jurjevic A, Bucuk M, Brnabic-Razmilic O, Relja G, Zorzon M (2003) Migraine and tension-type headache in Croatia: a population-based survey of precipitating factors. Cephalalgia 23:336–343, 12780762, 10.1046/j.1468-2982.2003.00544.x, 1:STN:280:DC%2BD3s3ls1emtw%3D%3D
Scharff L, Turk DC, Marcus DA (1995) Triggers of headache episodes and coping responses of headache diagnostic groups. Headache 35:397–403, 7672956, 10.1111/j.1526-4610.1995.hed3507397.x, 1:STN:280:DyaK2MvgtlWhtw%3D%3D
Peatfield RC (1995) Relationships between food, wine, and beer-precipitated migrainous headaches. Headache 35:355–357, 7635722, 10.1111/j.1526-4610.1995.hed3506355.x, 1:STN:280:DyaK2Mzmt1Ggsg%3D%3D
Spierings ELH, Ranke AH, Honkoop PC (2001) Precipitating and aggravating factors of migraine versus tension-type headache. Headache 41:554–558, 11437890, 10.1046/j.1526-4610.2001.041006554.x, 1:STN:280:DC%2BD38%2FhvFKnsA%3D%3D
Ierusalimschy R, Moreira Filho PF (2002) Precipitating factors of migraine attacks in patients with migraine without aura. Arq Neuropsiquiatr 60:609–613, 12244400
Kelman L (2007) The triggers or precipitants of the acute migraine attack. Cephalalgia 27:394–402, 17403039, 10.1111/j.1468-2982.2007.01303.x, 1:STN:280:DC%2BD2s3jvFKlsw%3D%3D
Chabriat H, Danchot J, Michel P, Joire JE, Henry P (1999) Precipitating factors of headache. A prospective study in a national control-matched survey in migraineurs and nonmigraineurs. Headache 39:335–338, 11279913, 10.1046/j.1526-4610.1999.3905335.x, 1:STN:280:DC%2BD3M7ovFajsQ%3D%3D
Wober C, Holzhammer J, Zeitlhofer J, Wessely P, Wober-Bingol C (2006) Trigger factors of migraine and tension-type headache: experience and knowledge of the patients. J Headache Pain 7:188–195, 16897622, 10.1007/s10194-006-0305-3
Karli N, Zarifoglu M, Calisir N, Akgoz S (2005) Comparison of pre-headache phases and trigger factors of migraine and episodic tension-type headache: do they share similar clinical pathophysiology? Cephalalgia 25:444–451, 15910569, 10.1111/j.1468-2982.2005.00880.x, 1:STN:280:DC%2BD2M3mvVGitA%3D%3D
Takeshima T, Ishizaki K, Fukuhara Y, Ijiri T, Kusumi M, Wakutani Y, Mori M, Kawashima M, Kowa H, Adachi Y, Urakami K, Nakashima K (2004) Population-based door-to-door survey of migraine in Japan: the Daisen study. Headache 44:8–19, 14979878, 10.1111/j.1526-4610.2004.04004.x
Ulrich V, Russell MB, Jensen R, Olesen J (1996) A comparison of tension-type headache in migraineurs and in non-migraineurs: a population-based study. Pain 67:501–506, 8951947, 10.1016/0304-3959(96)03164-8, 1:STN:280:DyaK2s7gvFKltQ%3D%3D
Ulrich V, Olesen J, Gervil M, Russell MB (2000) Possible risk factors and precipitants for migraine with aura in discordant twin-pairs: a population-based study. Cephalalgia 20:821–825, 11167911, 10.1046/j.1468-2982.2000.00135.x, 1:STN:280:DC%2BD3M3isFahsQ%3D%3D
Rasmussen BK (1993) Migraine and tension-type headache in a general population: precipitating factors, female hormones, sleep pattern and relation to lifestyle. Pain 53:65–72, 8316392, 10.1016/0304-3959(93)90057-V, 1:STN:280:DyaK3szgt12mug%3D%3D
Wober C, Brannath W, Schmidt K, Kapitan M, Rudel E, Wessely P, Wober-Bingol C, the PAMINA Study Group (2007) Prospective analysis of factors related to migraine attacks: the PAMINA study. Cephalalgia 27:304–314, 17376107, 10.1111/j.1468-2982.2007.01279.x, 1:STN:280:DC%2BD2s7ns1egtQ%3D%3D
Aamodt AH, Stovner LJ, Hagen K, Brathen G, Zwart J (2006) Headache prevalence related to smoking and alcohol use. The head-hunt study. Eur J Neurol 13:1233–1238, 17038038, 10.1111/j.1468-1331.2006.01492.x, 1:STN:280:DC%2BD28ngs1SltA%3D%3D
Mannix LK, Frame JR, Solomon GD (1997) Alcohol, smoking, and caffeine use among headache patients. Headache 37:572–576, 9385756, 10.1046/j.1526-4610.1997.3709572.x, 1:STN:280:DyaK1c%2Fks1yltA%3D%3D
Scher AI, Terwindt GM, Picavet HSJ, Verschuren WMM, Ferrari MD, Launer LJ (2005) Cardiovascular risk factors and migraine. The GEM population-based study. Neurology 64:614–620, 15728281, 1:STN:280:DC%2BD2M%2FpvVyjsg%3D%3D
Panconesi A, Capodarca C (2007) Migraine and alcohol: how many consumers? J Headache Pain 8(suppl):S32-S33 (abstract), (abstract)
Italians and alcohol. Consumption, trend and attitudes in Italy and in the Regions (2001) Fourth DOXA National Survey. Risa, Rome
Littlewood JT, Gibb C, Glover V, Sandler M, Davies PTG, Clifford Rose F (1988) Red wine as a cause of migraine. Lancet 1:558–559, 2894493, 10.1016/S0140-6736(88)91353-0, 1:STN:280:DyaL1c7ls1Cntg%3D%3D
Nicolodi M, Sicuteri F (1999) Wine and migraine: compatibility or incompatibility. Drugs Exp Clin Res XXV:147–153
Jansen SC, van Dusseldorp M, Bottema KC, Dubois AEJ (2003) Intolerance to dietary biogenic amines: a review. Ann Allergy Asthma Immunol 91:233–241, 14533654, 1:CAS:528:DC%2BD3sXotF2kt7o%3D, 10.1016/S1081-1206(10)63523-5
Jarisch R, Wantke F (1996) Wine and headache. Int Arch Allergy Immunol 110:7–12, 8645981, 1:STN:280:DyaK283hvVSjsA%3D%3D, 10.1159/000237304
Wantke F, Gotz M, Jarisch R (1994) The red wine provocation test: intolerance to histamine as a model for food intolerance. Allergy Proc 15:27–32, 8005453, 10.2500/108854194778816599, 1:STN:280:DyaK2c3nsVSmsQ%3D%3D
Maintz L, Novak N (2007) Histamine and histamine intolerance. Am J Clin Nutr 85:1185–1196, 17490952, 1:CAS:528:DC%2BD2sXls1KitLY%3D
Peatfield RC, Fletcher G, Rhodes K, Gardiner IM, de Belleroche J (2003) Pharmacological analysis of red wine-induced migrainous headaches. J Headache Pain 4:18–23, 10.1007/s101940300023, 1:CAS:528:DC%2BD3sXjsF2ktL0%3D
Lassen LH, Christiansen I, Iversen HK, Jansen-Olesen I, Olesen J (2003) The effect of nitric oxide synthase inhibition on histamine induced headache and arterial dilatation in migraineurs. Cephalalgia 23:877–886, 14616929, 10.1046/j.1468-2982.2003.00586.x, 1:STN:280:DC%2BD3srlsFeguw%3D%3D
Olesen J, Lassen LH (1995) Experimental headache induced by histamine, meta-chlorphenylpiperazine, and reserpine. In: Olesen J, Moskowitz A (eds) Experimental headache models. Lippincott-Raven, Philadelphia, pp 259–265
Marcus DA, Scharff L, Turk D, Gourley LM (1997) A double-blind provocative study of chocolate as a trigger of headache. Cephalalgia 17:855–862, 9453274, 10.1046/j.1468-2982.1997.1708855.x, 1:STN:280:DyaK1c7hsVSiuw%3D%3D
Littlewood JT, Glover V, Sandler M (1985) Red wine contains a potent inhibitor of phenolsulphotransferase. Br J Clin Pharmacol 19:275–278, 3857069, 1:CAS:528:DyaL2MXitF2mur0%3D
Sandler M, Li N-Y, Jarrett N, Glover V (1995) Dietary migraine: recent progress in the red (and white) wine story. Cephalalgia 15:101–103, 7641242, 10.1046/j.1468-2982.1995.015002101.x, 1:STN:280:DyaK2MzmvVKrtQ%3D%3D
Jones AL, Roberts RC, Colvin DW, Rubin GL, Coughtrie MWH (1995) Reduced platelet phenolsulphotransferase activity towards dopamine and 5-hydroxytryptamine in migraine. Eur J Clin Pharmacol 49:109–114, 8751031, 10.1007/BF00192368, 1:CAS:528:DyaK2MXmvVyntbo%3D
Vinson JA, Mandarano M, Hirst M, Trevithick JR, Bose P (2003) Phenol antioxidant quantity and quality in foods: beers and the effect of two type of beer on animal model of atherosclerosis. J Agric Food Chem 51:5528–5533, 12926909, 10.1021/jf034189k, 1:CAS:528:DC%2BD3sXlvVyksLc%3D
Engler MB, Engler MM, Chen CY, MalloY MJ, Browne A, Chiu EY, Kwak HK, Milbury P, Paul SM, Blumberg J, Mietus-Snyder ML (2004) Flavonoid-rich dark chocolate improves endothelial function and increase plasma epicatechin concentrations in healthy adults. J Am Coll Nutr 23:194–204
Dahl R, Henriksen JM, Harving H (1986) Red wine asthma: a controlled challenge study. J Allergy Clin Immunol 78:1126–1129, 3782677, 10.1016/0091-6749(86)90261-7, 1:STN:280:DyaL2s%2FlvVKitA%3D%3D
Vally H, Thompson PJ (2003) Allergic and asthmatic reactions to alcoholic drinks. Addict Biol 8:3–11, 12745410, 10.1080/1355621031000069828, 1:CAS:528:DC%2BD3sXitlegsr8%3D
Vally H, Thompson PJ, Misso NL (2007) Changes in bronchial hyperresponsiveness following high- and low-sulphite wine challenges in wine-sensitive asthmatic patients. Clin Exp Allergy 37:1062–1066, 17581200, 10.1111/j.1365-2222.2007.02747.x, 1:CAS:528:DC%2BD2sXos12hsrk%3D
Pattichis K, Louca LL, Jarman J, Sandler M, Glover V (1995) 5-Hydroxytryptamine release from platelets by different red wines: implications for migraine. Eur J Pharmacol 292:173–177, 7720790, 1:CAS:528:DyaK2MXjt1Smtr0%3D
Jarman J, Glover V, Sandler M (1991) Release of (14C) 5-hydroxytryptamine from human platelets by red wine. Life Sci 48:2297–2300, 2046460, 10.1016/0024-3205(91)90265-D, 1:CAS:528:DyaK3MXksVOktr0%3D
Jarman J, Pattichis K, Peatfield R, Glover V, Sandler M (1996) Red wine-induced release of [14C] 5-hydroxytryptamine from platelets of migraine patients and controls. Cephalalgia 16:41–43, 8825698, 10.1046/j.1468-2982.1996.1601041.x, 1:STN:280:DyaK28vitlSqtQ%3D%3D
Pattichis K, Louca L, Jarman J, Glover V (1994) Red wine can cause a rise in human whole blood 5-hydroxytryptamine levels. Med Sci Res 22:381–382, 1:CAS:528:DyaK2cXmtVertLg%3D
Boyer JC, Bancel E, Perray PF, Pouderoux P, Balmes JL, Bali JP (2004) Effect of champagne compared to still white wine on peripheral neurotransmitter concentrations. Int J Vitam Nutr Res 74:321–328, 15628669, 10.1024/0300-9831.74.5.321, 1:CAS:528:DC%2BD2MXhvFemsg%3D%3D
Yanez M, Fraiz N, Cano E, Orallo F (2006) Inhibitory effects of cis- and trans-resveratrol on noradrenaline and 5-hydroxytryptamine uptake and on monoamine oxidase activity. Biochem Biophys Res Comm 344:688–695, 16631124, 10.1016/j.bbrc.2006.03.190, 1:CAS:528:DC%2BD28XjvFWnsrg%3D
Panconesi A, Sicuteri R (1997) Headache induced by serotonergic agonists—a key to the interpretation of migraine pathogenesis? Cephalalgia 17:3–14, 9051329, 10.1046/j.1468-2982.1997.1701003.x, 1:STN:280:DyaK2s3gtlOmtQ%3D%3D
Zhang XC, Strassman AM, Burnstein R, Levy D (2007) Sensitization and activation of intracranial meningeal nociceptors by mast cell mediators. J Pharmacol Exp Ther 322:806–812, 17483291, 10.1124/jpet.107.123745, 1:CAS:528:DC%2BD2sXoslSju7w%3D
Fitzpatrick DF, Hirschfield SL, Coffey RG (1993) Endothelium-dependent vasorelaxing activity of wine and other grape products. Am J Physiol 265:H774–H778, 8396352, 1:CAS:528:DyaK3sXmsVKltbk%3D
Madeira SV, de Castro Resende A, Ognibene DT, de Sousa MA, Soares de Moura R (2005) Mechanism of the endothelium-dependent vasodilator effect of alcohol-free extract obtained from a vinifera grape skin. Pharmacol Res 52:321–327, 16023862, 10.1016/j.phrs.2005.05.005, 1:CAS:528:DC%2BD2MXos1ahsr0%3D
Leikert JF, Rathel TR, Wohlfart P, Cheynier V, Vollmar AM, Dirsch VM (2002) Red wine polyphenols enhance endothelial nitric oxide synthase expression and subsequent nitric oxide release from endothelial cells. Circulation 106:1614–1617, 12270851, 10.1161/01.CIR.0000034445.31543.43, 1:CAS:528:DC%2BD38XntVyntrw%3D
Agewall S, Wright S, Doughty RN, Whalley GA, Duxbury M, Sharpe N (2000) Does a glass of red wine improve endothelial function? Eur Heart J 21:74–78, 10610747, 10.1053/euhj.1999.1759, 1:STN:280:DC%2BD3c%2FnvFSksQ%3D%3D
Vlachopoulos C, Tsekoura D, Tsiamis E, Panagiotakos D, Stefanidis C (2003) Effect of alcohol on endothelial function in healthy subjects. Vasc Med 8:263–265, 15125487, 10.1191/1358863x03vm505oa
Thomsen LL, Olesen J (2001) Nitric oxide in primary headaches. Curr Opin Neurol 14:315–321, 11371754, 10.1097/00019052-200106000-00009, 1:STN:280:DC%2BD3M3nslOgug%3D%3D
Gazzieri D, Trevisani M, Tarantini F, Bechi P, Masotti G, Gensini GF, Castellani S, Marchionni N, Geppetti P, Harrison S (2006) Ethanol dilates coronary arteries and increases coronary flow via transient receptor potential vanilloid 1 and calcitonin gene-related peptide. Cardiovasc Res 70:589–599, 16579978, 10.1016/j.cardiores.2006.02.027, 1:CAS:528:DC%2BD28Xks1Wlu7g%3D
Mc Bride WJ, Murphy JM, Lumeng L, Li TK (1989) Serotonin and ethanol preference. Recent Dev Alcohol 7:187–209, 1:CAS:528:DyaL1MXkslamt7o%3D
Mc Bride WJ, Chernet E, Russel RN, Wong DT, Guan XM, Lumeng L, Li TK (1997) Regional CNS densities of monoamine receptors in alcohol-naïve alcohol-preferring P and -nonpreferring NP rats. Alcohol 14:141–148, 10.1016/S0741-8329(96)00117-6, 1:CAS:528:DyaK2sXisVegtbg%3D
Portas CM, Devoto P, Gessa GL (1994) Effect of ethanol on extracellular 5-hydroxytryptamine output in rat frontal cortex. Eur J Pharmacol 270:123–125, 8157078, 1:CAS:528:DyaK2cXhsFKntrc%3D
Smith AD, Weiss F (1999) Ethanol exposure differentially alters central monoamine neurotransmission in alcohol-preferring versus –nonpreferring rats. J Pharmacol Exp Ther 288:1223–1228, 10027862, 1:CAS:528:DyaK1MXhs1Kis74%3D
Van den Bergh V, Amery WK, Waelkens J (1987) Trigger factors in migraine: a study conducted by the Belgian Migraine Society. Headache 27:191–196, 3597073, 10.1111/j.1526-4610.1987.hed2704191.x
Kurth T, Graziano JM, Cook NR, Logroscino G, Diener H-C, Buring JE (2006) Migraine and risk of cardiovascular disease in women. JAMA 296:283–291, 16849661, 10.1001/jama.296.3.283, 1:CAS:528:DC%2BD28XntVWqsLg%3D
Kurth T, Graziano JM, Cook NR, Bubes V, Logroscino G, Diener HC, Buring JE (2007) Migraine and risk of cardiovascular disease in men. Arch Intern Med 167:795–801, 17452542, 10.1001/archinte.167.8.795
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License ( https://creativecommons.org/licenses/by-nc/2.0 ), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Panconesi, A. Alcohol and migraine: trigger factor, consumption, mechanisms. A review. J Headache Pain 9, 19–27 (2008). https://doi.org/10.1007/s10194-008-0006-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10194-008-0006-1