Abstract
The objective of the study was to assess the efficacy and tolerability of sodium valproate (VPA) on chronic daily headache (CDH) in a prospective, double-blind, randomized, placebo-controlled trial. Seventy patients were included in the study. Twenty-nine had chronic migraine (CM) and 41 had chronic tension-type headache (CTTH). VPA and placebo were applied for 3 months to 40 and 30 patients, respectively. Visual analog scale (VAS) and pain frequency (PF) were used for evaluation. VPA decreased the maximum pain VAS levels (MaxVAS) and PF at the end of the study (P = 0.028 and P = 0.000, respectively), but did not change general pain VAS (GnVAS) levels (P = 0.198). In CM patients, the decreases in MaxVAS, GnVAS and PF parameters were more in VPA treated patients (P = 0.006, P = 0.03, and P = 0.000, respectively). VPA treatment caused more reduction in PF than placebo in the CTTH subgroup (P = 0.000). VPA is effective in the prophylactic treatment of CDH by reducing MaxVAS levels and PF. It was more effective in CM than in CTTH.
Similar content being viewed by others
Introduction
Chronic daily headache (CDH) is defined as headache present more than 15 days per month. Patients with CDH often overuse analgesics, ergot derivates, sedatives or triptans [1]. CDH is a type of intractable headache that is seen frequently. Primary CDH can be subdivided into chronic migraine (CM), chronic tension-type headache (CTTH), hemicrania continua (HC), and new daily persistent headache (NDPH). Each of these types of CDH can occur with or without the overuse of medications [2]. CM consists of a daily headache lasting at least 4 h. Patients with CM have prior history of migraine with special features categorized by International Headache Society or a history of increasing frequency of migraine but decreasing severity of migraine-associated features. CM, compared with CTTH, has distinguishing features that are preservation of migraine-related symptoms, menstrual association, and a better response to antimigraine agents [3].
It is important to have a highly effective agent as well as one with good tolerability and an excellent safety profile in the treatment of CDH and migraine. VPA can be used for a prolonged period as a sole agent for the successful treatment of migraine [3]. Results from migraine clinical trials and a long-term extension studies have found that VPA achieves this standard of care. Open-label and placebo-controlled trials from 1980s and early 1990s demonstrated a positive response with divalproex sodium in migraine prevention [4–7]. The mechanism whereby VPA benefits migraine is unclear. VPA may affect many events in the migraine cascade [8, 9].
According to the literature, we thought that VPA could be used as an effective agent for the successful treatment of CDH. Therefore, we planned this study to evaluate the efficacy and tolerability of VPA in prophylactic monotherapy treatment of CDH and its subgroups in a placebo controlled, prospective, double-blind randomized trial.
Materials and methods
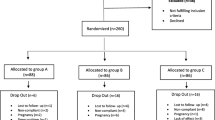
This trial is a prospective, randomized and double-blind research. The patients applied to Neurology Department of Suleyman Demirel University, School of Medicine between July 2003 and May 2004 and matching the criteria of the primary CDH were included in this study. Suleyman Demirel University, School of Medicine ethic committee approved the study. Detailed information has been given to all the patients, and those who accepted the treatment were included the study.
Detailed physical and neurological examinations have been applied to all the patients. Hematology, blood chemistry tests consisting of liver function tests, thyroid function tests, blood urea nitrogen, creatine, electrolytes, vitamin B12, folic acid, and ferritin were performed at the initial screening to evaluate secondary reasons of headache. Cervical X-rays and CT brain scan were also applied to some patients if necessary. At the end of these examinations, patients who have organic pathology such as anemia, malignancy, hemorrhagic diathesis, disthyrodism, hypertension and major depression were not included to the study. The patients were taking antidepressant and beta-blockers discontinued the medications. After 3 weeks, they were included to the study. Due to low number of patients, the subgroups of HC and NDPH were excluded. The final number of patients included in the study was 70. Twenty-nine of them had CM and 41 CTTH. Seventy patients consisting of 40 from VPA group and 30 from placebo group have been evaluated. Initial dose of the treatment was 500 mg per day. After one week, the dose was increased to 500 mg twice a day. Liver function tests and total blood count assay have been applied to all the patients at the end of 4th and 12th weeks of the study.
During the treatment period, patients recorded their headache frequencies and intensities in diaries, which were reviewed at each follow-up visit.
Visual analog scale (VAS) was used to define the pain level. General pain VAS level (GnVAS), maximum pain VAS level (MaxVAS), and pain frequency (PF, number of days with pain in a month) were used to evaluate the efficacy of the treatment. Drugs with the same identical color and shape were given to patients randomly. The patients were followed up for 3 months.
Mann–Whitney U and Wilcoxon signed tests were performed via Statistical Package for the Social Sciences (SPSS) software for statistical analysis. P values less than 0.05 were considered statistically significant.
Results
Sodium valproate and placebo groups consisted of 5 male (12.5%), 35 female (87.5%), and 7 male (23.3%), 23 female (76.7%), respectively. As seen in Table 1, mean ages (minimum–maximum) of VPA and placebo groups were 40.0 ± 14.5 (14–76) and 40.3 ± 12.8 (14–66) years, respectively. The ages were not significantly different (P = 0.929).
The patients in VPA and placebo groups suffered from headache for the range of 6–240 and 6–120 months, respectively. Duration of disease between the two groups was not significantly different (P = 0.337).
At the beginning of the study, GnVAS, MaxVAS, and PF values were not significantly different when VPA and placebo groups compared (P = 0.05, P = 0.06, and P = 0.089 for GnVAS, MaxVAS, and PF, respectively).
Efficacy of VPA in the prophylactic monotherapy when compared with placebo group in CDH patients
Before treatment, GnVAS value was 6.8 ± 1.1 and it reduced to 4.0 ± 2.1 (P = 0.545) at the end of the first month and to 3.5 ± 2.0 (P = 0.198) at the end of the third month. Initial MaxVAS and PF values were 8.9 ± 0.9 and 22.8 ± 6, respectively. MaxVAS levels at the first and third month were 5.2 ± 2.5 and 4.8 ± 2.5, respectively (P = 0.020 and P = 0.028). PF values at the first and third month were 10.1 ± 6.0 and 8.3 ± 6.1, respectively (P = 0.000 and P = 0.000). There was no statistically significant difference between the VPA and placebo groups by means of decrement in GnVAS values at the end of the first and the third month of the treatment. But, decrements in MaxVAS levels and PF parameters were significant between the two groups (Table 2).
Efficacy of VPA in the treatment of CM patients
Sodium valproate (n = 17) and placebo (n = 12) groups in CM were compared. At the end of the first month, VPA caused to reduce the level of MaxVAS and PF parameters (P = 0.01 and P = 0.000, respectively). At the end of the third month, not only MaxVAS and PF parameters but also GnVAS levels significantly reduced (P = 0.03, P = 0.006 and P = 0.000 for GnVAS, MaxVAS, and PF, respectively). The efficacy of VPA in CM started after the first month of treatment (Table 2).
Efficacy of VPA in the treatment of CTTH patients
As seen in Table 2, VPA (n = 23) and placebo (n = 18) groups in CTTH were compared. No significant reduction was seen in GnVAS and MaxVAS at the end of the first month (P = 0.455 and P = 0.416, respectively). Only PF parameter was significantly reduced in VPA group when compared to placebo group at the end of the first and third months (P = 0.000, for both).
Adverse events
In the present study, the incidence of adverse effects of VPA was rare. Somnolence and tremor was shown in a patient; impotence occurred in a male patient; and hairy loss was seen in one subject. These symptoms disappeared by stopping the treatment of VPA. In placebo group one patient refused to continue treatment because of dizziness and nausea.
Hematology and blood chemistry assessments were performed for all the cases at the beginning, at the end of 4th and 12th week of the trial. All the tests were in normal range during the treatment period.
Discussion
The data demonstrate that VPA reduces pain level and PF in patients with CDH when compared with placebo. Furthermore, among the subgroups of CDH, it was more effective in CM than in CTTH.
Divalproex sodium (composed of sodium valproate and valproic acid) has been found to be useful for the treatment of migraine. The newer antiepileptic drugs (AEDs), including topiramate, divalproex sodium, and to a lesser extent, gabapentin, have shown efficacy in controlled trials of migraine prevention [10–17]. And also as mentioned in Pascual’s review [18] AEDs may have a role for the prevention of cluster headache. To date, only topiramate, gabapentin, tizanidine, fluoxetine, amitriptyline, and botulinum toxin typeA have been evaluated as prophylactic treatment of CDH in randomized, double-blind, placebo-controlled, or active comparator-controlled trials [19]. For that reason we aimed to evaluate the efficacy and safety of VPA compared with placebo in prophylactic monotherapy treatment of CDH and its subgroups in a prospective, double-blind, and randomized trial.
Long-duration CDH is a significant public health concern. Approximately 3–5% of the population worldwide have daily or near-daily headaches [20]. AEDs, especially VPA, have mechanisms of action that may be effective for the prevention of chronic headaches and migraine attacks.
In our study VPA has significantly positive effect on PF and MaxVAS level in patients with CDH. As there was no statistically significant difference between the VPA and placebo groups by means of decrement in GnVAS values in first and third months after the treatment, decrement in MaxVAS level and PF parameters occurred in the same period was significant. This means that there was a statistically significant decrease in MaxVAS levels and pain frequencies in VPA given group. Freitag et al. [3] in a retrospective study, reported that divalproex sodium can be used for a prolonged period as a sole agent for the successful treatment of CDH. In their report, nearly 75% of the patients had at least a 50% reduction in PF. Mathew and Ali [21] conducted an open-label trial of 30 patients using doses of divalproex sodium between 1,000 mg and 2,000 mg per day. Based on weekly headache index, headache-free days, dysfunctional days, patients’ general well-being rating and physicians’ global assessment were improved significantly in two-thirds of the patients. In another study, Rothrock et al. [22] consecutively recruited 75 patients with intractable headache syndromes, divided them into three groups as frequent migraine, transformed migraine, and tension type headache based on their headache symptoms and treated all the 75 patients with 500 mg divalproex sodium twice daily. Thirty-six patients (48%) reported a 50% or greater reduction in headache frequency. Contrarily, Vijayan and Spillane [23] reported that VPA was not significantly effective in the treatment of CDH in 16 patients.
We initiated treatment on 500 mg once daily for 1 week, and the dose was then increased to 500 mg twice daily as in the study of Freitag et al. [8]. Between CM and CTTH subgroups, we found that VPA was more effective in CM than in CTTH.
The patients with CM in VPA and placebo groups were compared. At the end of first month, there were significant decrements between the VPA and placebo groups in terms of MaxVAS and PF parameters. At the end of the third month, not only MaxVAS and PF parameters but also GnVAS levels significantly reduced. But in CTTH patients, VPA treatment is effective only on the PF parameter. The decrements in other parameters were not significant. Similarly, Lenaerts et al. [24] performed an open prospective study of the prophylactic efficacy of VPA in 56 patients among which 35 migraineurs, 7 CTTH patients and 14 patients with combined headaches. Sixty percent of migraineurs had a 75% or more improvement in the number of headache days under VPA treatment. There was no significant improvement in CTTH patients and only a mild effect in patients with combined headaches, almost exclusively on the migraine component. In another study, Rothrock et al. [25] prospectively evaluated 20 patients with transformed migraine and treated with divalproex sodium 500–1,500 mg/day for 12 weeks. Seventy-five percent of patients reported a positive response at the end of first month. In the study of Freitag et al. [3] it was reported that VPA was effective in the majority of patients and in those who could differentiate between migraine and tension-type headache components. The migraine component appeared to demonstrate the best response as appeared in our study.
From this study, we clinically demonstrated that the incidence of adverse effects were less than those seen in previous studies. None of the following adverse effects such as hepatotoxicity, gastric intolerance and weight gain was observed. Interestingly, in one male patient, impotence occurred as a side effect after the first month. When the VPA was discontinued, his symptom was disappeared. No literature was found reporting impotence resulted from VPA use.
In summary, we report a randomized, placebo-controlled trial demonstrating that VPA is superior to placebo in prophylactic treatment of CDH. The clinical beneficial effect of VPA in CM was more than CTTH. VPA appears to be a worthwhile addition to the prophylactic treatment of CDH as a well tolerated drug.
References
Schwartz TH, Karpitskiy VV, Sohn RS (2002) Intravenous valproate sodium in the treatment of daily headache. Headache 42(6):519–522, 12167141, 10.1046/j.1526-4610.2002.02127.x
Silberstein SD, Lipton RB, Sliwinski M (1996) Classification of daily and near-daily headache: a field study of revised IHS criteria. Neurology 47:871–875, 8857711, 1:STN:280:DyaK2s%2FhtVKkug%3D%3D
Freitag FG, Diamond S, Diamond ML, Urban GJ (2001) Divalproex in the long-term treatment of chronic daily headache. Headache 41:271–278, 11264687, 10.1046/j.1526-4610.2001.111006271.x, 1:STN:280:DC%2BD3M7ms1ehtg%3D%3D
Sorensen KV (1988) Valproate: a new drug in migraine prophylaxis. Acta Neurol Scand 78:346–348, 3146862, 1:STN:280:DyaL1M7jtFKjtQ%3D%3D, 10.1111/j.1600-0404.1988.tb03667.x
Hering R, Kuritzky A (1992) Sodium valproate in the prophylactic treatment of migraine: a double-blind study versus placebo. Cephalalgia 12(2):81–84, 1576648, 10.1046/j.1468-2982.1992.1202081.x, 1:STN:280:DyaK383kvVOjtg%3D%3D
Hering R, Kuritzky A (1989) Sodium valproate in the treatment of cluster headache: an open clinical trial. Cephalalgia 9:195–198, 2507161, 10.1046/j.1468-2982.1989.0903195.x, 1:STN:280:DyaK3c%2FgtlWqug%3D%3D
Jensen R, Brinck T, Olesen J (1994) Sodium valproate has a prophylactic effect in migraine without aura: a triple-blind, placebo-controlled crossover study. Neurology 44(4):647–651, 8164818, 1:STN:280:DyaK2c3hslyqsg%3D%3D
Freitag FG, Collins SD, Carlson HA, Goldstein J, Saper J, Silberstein S, Mathew N, Winner PK, Deaton R, Sommerville K; Depakote ER Migraine Study Group (2002) A randomized trial of divalproex sodium extended-release tablets in migraine prophylaxis. Neurology 11(58):1652–1659
Taylor K, Goldstein J (1996) High-dose versus low-dose valproic acid as a prophylactic medication. Headache 36(8):514–515, 8824009, 10.1046/j.1526-4610.1996.3608514.x, 1:STN:280:DyaK28vitFensg%3D%3D
Klapper J (1997) Divalproex sodium in migraine prophylaxis: a dose-controlled study. Cephalalgia 17:103–108, 9137847, 10.1046/j.1468-2982.1997.1702103.x, 1:STN:280:DyaK2s3otlOluw%3D%3D
Hering R, Kuritzky A (1992) Sodium valproate in the prophylactic treatment of migraine: a double-blind study versus placebo. Cephalalgia 12:81–84, 1576648, 10.1046/j.1468-2982.1992.1202081.x, 1:STN:280:DyaK383kvVOjtg%3D%3D
Kaniecki RG (1997) A comparison of divalproex with propanolol and placebo for the prophylaxis of migraine without aura. Arch Neurol 54:1141–1145, 9311358, 1:STN:280:DyaK2svlslGnuw%3D%3D
Jensen R, Brinck T, Olesen J (1994) Sodium valproate has a prophylactic effect in migraine without aura: a triple-blind, placebo controlled crossover study. Neurology 44:647–651, 8164818, 1:STN:280:DyaK2c3hslyqsg%3D%3D
Silberstein SD, Neto W, Schmitt J, Jacobs D, MIGR-001 Study Group (2004) Topiramate in migraine prevention: results of a large controlled trial. Arch Neurol 61:490–495, 15096395, 10.1001/archneur.61.4.490
Brandes JL, Saper JR, Diamond M, et al MIGR-002 Study Group (2004) Topiramate for migraine prevention: a randomized controlled trial. JAMA 291:965–973
Diener HC, Tfelt-Hansen P, Dahlof C, Lainez MJ, Sandrini G, Wang SJ, Neto W, Vijapurkar U, Doyle A, Jacobs D, The MIGR-003 Study Group (2004) Topiramate in migraine prophylaxis: results from a placebo-controlled trial with propranolol as an active control. J Neurol 251:943–950, 15316798, 10.1007/s00415-004-0464-6, 1:CAS:528:DC%2BD2cXosVSrtLc%3D
Mathew NT, Rapoport A, Saper J et al (2001) Efficacy of gabapentin in migraine prophylaxis. Headache 41:119–128, 11251695, 10.1046/j.1526-4610.2001.111006119.x, 1:STN:280:DC%2BD3MzmvVKktw%3D%3D
Pascual J, Lainez MJ, Dodick D, Hering-Hanit R (2007) Antiepileptic drugs for the treatment of chronic and episodic cluster headache. Headache 47(1):81–89, 17355498, 10.1111/j.1526-4610.2007.00653.x
Mathew NT (2006) The prophylactic treatment of chronic daily headache. Headache 46(10):1552–1564, 17115988, 10.1111/j.1526-4610.2006.00621.x
Silberstein SD (2005) Chronic daily headache. JAOA 105(4 Suppl 2):23S–29S, 15928350
Mathew NT, Ali S (1991) Valproate in the treatment of persistent chronic daily headache. An open label study. Headache 31(2):71–74, 2030076, 10.1111/j.1526-4610.1991.hed3102071.x, 1:STN:280:DyaK3M3jtFCjsA%3D%3D
Rothrock JF (1999) Management of chronic daily headache utilizing a uniform treatment pathway. Headache 39:650–653, 11279960, 10.1046/j.1526-4610.1999.3909650.x, 1:STN:280:DC%2BD3M7ovFWmsw%3D%3D
Vijayan N, Spillane T (1995) Valproic acid treatment of chronic daily headache. Headache 35:540–543, 8530278, 10.1111/j.1526-4610.1995.hed3509540.x, 1:STN:280:DyaK28%2FosVCrtg%3D%3D
Lenaerts M, Bastings E, Sianard J, Schoenen J (1996) Sodium valproate in severe migraine and tension-type headache: an open study of long-term efficacy and correlation with blood levels. Acta Neurol Belg 96(2):126–129, 8711985, 1:STN:280:DyaK28zjslCjsg%3D%3D
Rothrock JF, Mendizabal JE (2000) An analysis of the “carry-over effect” following successful short-term treatment of transformed migraine with divalproex sodium. Headache 40(1):17–19, 10759897, 10.1046/j.1526-4610.2000.00002.x, 1:STN:280:DC%2BD3c3itlemtg%3D%3D
Author information
Authors and Affiliations
Corresponding author
Additional information
This study was presented as a poster at “8th Headache Congress Of The European Headache Federation” in Valencia, Spain, between 26–29 April, 2006 and published as an abstract in The Journal of Headache and Pain, Vol 7, Suppl 1 S39 April 2006.
An editorial commentary on this article can be found at http://doi.dx.org/10.1007/s10194-008-0010-5.
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License ( https://creativecommons.org/licenses/by-nc/2.0 ), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Yurekli, V.A., Akhan, G., Kutluhan, S. et al. The effect of sodium valproate on chronic daily headache and its subgroups. J Headache Pain 9, 37–41 (2008). https://doi.org/10.1007/s10194-008-0002-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10194-008-0002-5