Abstract
We (JMAAV [Japanese patients with MPO-ANCA-associated vasculitis] Study Group) performed a prospective, open-label, multi-center trial to evaluate the usefulness of severity-based treatment in Japanese patients with myeloperoxidase-anti-neutrophil cytoplasmic antibodies (MPO-ANCA)-associated vasculitis. Patients with MPO-ANCA-associated vasculitis received a severity-based regimen according to the appropriate protocol: low-dose corticosteroid and, if necessary, cyclophosphamide or azathioprine in patients with mild form; high-dose corticosteroid and cyclophosphamide in those with severe form; and the severe-form regimen plus plasmapheresis in those with the most severe form. We followed up the patients for 18 months. The primary end points were the induction of remission, death, and end-stage renal disease (ESRD). Fifty-two patients were registered, and 48 patients were enrolled in this study (mild form, n = 23; severe form, n = 23; most severe form, n = 2). Among the 47 patients who received the predefined therapies, 42 achieved remission within 6 months, 5 died, and 1 developed ESRD. Disease flared up in 8 of the 42 patients with remission during the 18-month follow-up period. The JMAAV trial is the first prospective trial for MPO-ANCA-associated vasculitis to be performed in Japan. The remission and death rates were comparable to those in several previous clinical trials performed in western counties. The regimen employed in this trial was tailor-made based on patients’ disease severity and disease type, and it seems that standardization can be consistent with treatment choices made according to severity.
Similar content being viewed by others
Introduction
Among small-vessel vasculitides, microscopic polyangiitis (MPA), Wegener’s granulomatosis (WG), and allergic granulomatous angiitis (AGA) are known collectively as anti-neutrophil cytoplasmic antibodies (ANCA)-associated vasculitis (AAV) because of the involvement of ANCA as the common pathogenesis [1]. The major target antigens of ANCA associated with vasculitis are myeloperoxidase (MPO) and proteinase 3 (PR3). MPO-ANCA is related to MPA and AGA, and PR3-ANCA is the marker antibody in WG [2, 3]. MPO-ANCA-associated vasculitis is more common in Japan [4], whereas PR3-ANCA-associated vasculitis is more common in Europe and the United Staates. Granulomatosis with polyangiitis (GPA) (Wegener’s) has been proposed as an alternative name for WG [5].
Untreated patients with severe AAV with multi-organ involvement have a poor prognosis, which can be improved by combination therapy with cyclophosphamide and high-dose corticosteroid [6]. Randomized controlled trials (RCTs) have indicated a rate of AAV remission induction of approximately 90% in 6 months with the standard regimen [7, 8]. As cyclophosphamide induces severe toxicity, there have been many attempts to develop less toxic regimens.
The European CYCAZAREM (cyclophosphamide vs. azathioprine as remission maintenance therapy for AAV) RCT compared the effectiveness of cyclophosphamide and azathioprine in the maintenance of remission [7]. The study population consisted of 155 patients (WG, n = 95; MPA, n = 60) who achieved remission after induction therapy with oral cyclophosphamide plus prednisolone. The patients were assigned randomly to one of two groups with continuation of either cyclophosphamide or azathioprine. The rates of relapse were not significantly different between the two groups at 18-month follow-up. Thus, this study clearly demonstrated that maintenance of remission could also be achieved with oral azathioprine.
Another European RCT, NORAM (non-renal vasculitis alternative treatment with methotrexate), compared methotrexate and cyclophosphamide with regard to remission induction and maintenance in patients with AAV without significant renal involvement [8]. In this trial, 95 patients with newly diagnosed AAV (89 with WG and 6 with MPA) were assigned to receive methotrexate or cyclophosphamide. At 6 months, 90 and 94% of patients in the methotrexate and cyclophosphamide groups, respectively, had achieved remission. Among the patients who achieved remission, the relapse rate at 18 months was significantly higher in the methotrexate group. Thus, methotrexate was as effective as cyclophosphamide for the induction of remission in patients with non-renal mild AAV, but was associated with a significantly higher relapse rate.
The two RCTs mentioned above included 250 patients with AAV, among whom 184 patients (74%) had WG, presumably related to the epidemiological background. This is a striking difference from the disease prevalence in Japan, where MPA and MPO-ANCA-associated vasculitis are more common [4]. Therefore, caution must be taken in applying the results of these RCTs to Japanese patients. In this regard, a prospective study was performed to clarify the effectiveness of the standard regimen in Japanese patients with MPO-ANCA-associated vasculitis.
Patients, materials, and methods
Study design
The protocol for a prospective, open-label, multi-center trial was developed by the investigators of the Research Group of Intractable Vasculitis, the Research Group of Progressive Glomerular Disease, and the Research Committee of Complications and Treatment of Immunological Disorders, Ministry of Health, Labor, and Welfare (MHLW) of Japan. The trial was registered as “Prospective study of the severity-based treatment protocol for Japanese patients with MPO-ANCA-associated vasculitis (JMAAV)” at the University Hospital Medical Information Network, Clinical Trials Registry (UMIN-CTR; http://www.umin.ac.jp/ctr/index-j.htm, registration number ID 000000867). The members of the JMAAV Study Group other than the authors are listed in the “Acknowledgments”.
Patients positive for MPO-ANCA, who had newly diagnosed MPA according to the diagnostic criteria for MPA of the Research Group of Intractable Vasculitis, MHLW of Japan [9], were screened for eligibility. ANCA was tested by enzyme-linked immunosorbent assay (ELISA) for MPO or PR3. Eligible patients were included in the study after providing written informed consent, in accordance with the Declaration of Helsinki.
Exclusion criteria were as follows: (1) age >79 years, (2) peripheral leukocyte count <4000/mm3, (3) peripheral platelet count <120,000/mm3, (4) coexistence of active infection, (5) end-stage renal disease (ESRD) requiring hemodialysis, (6) respiratory failure with PaO2 <60 Torr, (7) liver cirrhosis, (8) malignancy diagnosed within 5 years, (9) pregnancy, or (10) history of cyclophosphamide therapy with a cumulative dose of >10 g.
All patients were stratified into one of three categories based on their disease severity and distribution of organ involvement. (1) Severe form: this form included a generalized type (MPA with involvement of more than two organs), a pulmo-renal type (glomerulonephritis plus either limited pulmonary hemorrhage or extended interstitial pneumonia), and a rapidly progressive glomerulonephritis (RPGN) type. (2) Most severe form: this form was defined as patients with diffuse alveolar hemorrhage, intestinal perforation, acute pancreatitis, cerebral hemorrhage, or concurrent anti-glomerular basement membrane antibodies. This form also included patients with the severe form who were resistant to the severity-based treatment protocol described below. (3) Mild form: this form included a renal-limited type (except for RPGN), a pulmonary-limited type (except for pulmonary hemorrhage), and other mild forms. Patients were treated according to the predefined protocol described below.
Severity-based treatment protocol for induction of remission
To induce remission, patients with the severe form were treated with a regimen consisting of high-dose prednisolone (0.6–1.0 mg/kg/day) plus oral cyclophosphamide (0.5–2.0 mg/kg/day). Intravenous methylprednisolone (0.5–1.0 g/day for 3 days) was also considered in these patients. Instead of oral administration, the use of intravenous cyclophosphamide (0.5–0.75 g/m2, monthly) was also allowed. In patients with impaired renal function (serum creatinine level >1.8 mg/dL) or those older than 60 years, the dose of cyclophosphamide was reduced to 75–50%. Patients with the RPGN type were further evaluated depending on their age, serum creatinine level, C-reactive protein (CRP), and presence of lung involvement. Details of this scoring system were described elsewhere [10]. Briefly, the scoring system employed was as follows. Score 1 included either serum creatinine ≥3 and <6 mg/dL, age 60–69 years, or CRP ≥2.6 and <10 mg/dL. Score 2 included either serum creatinine ≥6 mg/dL, age ≥70 years, or CRP ≥10 mg/dL, or the presence of lung involvement. Score 3 included the induction of hemodialysis. Patients were categorized into four clinical grades by the sum of the scores. Grades 1, 2, 3, and 4 are equivalent to the sums of the scores 0–2, 3–5, 6–7, and 8–9, respectively. The regimen for the patients classified as grade 1–2 and age ≥70 years or under hemodialysis consisted of prednisolone at 0.6–0.8 mg/kg/day. The regimen for patients classified as grade 3–4 and age ≥70 years or under hemodialysis consisted of intravenous methylprednisolone (0.5–1.0 g/day for 3 days) followed by prednisolone at 0.6–0.8 mg/kg/day. The use of oral cyclophosphamide (starting at 25 mg/day) was also allowed based on the disease activity. The regimen for the patients classified as any grade and age <70 years and without hemodialysis was the same as that for the generalized type and renal-pulmonary type of the severe form mentioned above. Cyclophosphamide, however, was not necessarily used, depending on the renal function.
Patients with the most severe form were treated with plasmapheresis (2.0–3.0 L/day for 3 days; several sessions) together with the regimen for the severe form described above.
Patients with the mild form were treated with oral prednisolone (0.3–0.6 mg/kg/day). Oral immunosuppressive agents (cyclophosphamide or azathioprine, 0.5–1.0 mg/kg/day or 25–75 mg/day, respectively) were also allowed.
Treatment protocol for maintenance of remission and prophylaxis against infection
Patients with any form who had attained remission received maintenance therapy for an additional year, consisting of prednisolone (5–10 mg/day), and in most cases oral cyclophosphamide or azathioprine (25–75 mg/day). Prophylaxis against infection, if necessary, was considered for each patient, and therefore no systematic regimen for prophylaxis was predetermined.
Definitions
Remission was defined as the absence of clinical manifestations of active vasculitis and a Birmingham Vasculitis Activity Score 2003 (BVAS2003) of 0–1 point [11]. Relapses were defined as the recurrence or development of at least one manifestation of vasculitis. The involvement of each organ was diagnosed as follows: (a) localized pulmonary hemorrhage was defined as a hemorrhagic shadow in <30% of the whole lung area on chest X-rays. Generalized interstitial lung fibrosis was defined as a fibrotic shadow in >30% of the whole lung area on chest X-rays, but lacking pulmonary failure, with PaO2 <60 Torr. (b) Patients with RPGN were defined as those with hematuria, proteinuria, and/or urinary casts who developed renal failure within several weeks or months. Although not a necessary sign, increases in serum creatinine level more than twice in a month may aid in the diagnosis. (c) Cardiac involvement was defined as the occurrence of fresh myocardial infarction, pericarditis, or myocarditis. (d) Nervous system involvement was defined as fresh cerebral bleeding or infarction, mononeuritis multiplex, or organic consciousness disturbance. (e) Gastrointestinal involvement was defined as melena, pancreatic necrosis, or abnormal results on liver function tests. (f) Skin involvement was defined as multiple purpura or skin ulcers. (g) Involvement of the eyes and ear/nose/throat regions was defined as scleritis, uveitis, retinitis, optic neuritis, acute otitis media, acute internal otitis, or hemorrhagic rhinitis.
Evaluation
Study assessments were performed at entry, and at 6 weeks, 12 weeks, and 6 months, then every 3 months for 12 months, and at relapse. Assessments included complete blood count, measurement of the erythrocyte sedimentation rate (ESR), CRP, serum creatinine, liver enzymes, urinalysis, MPO-ANCA, and chest radiography. High-resolution computed tomography of the lung and pulmonary function tests such as forced vital capacity (FVC), forced expiratory volume in 1 s (FEV1), and carbon monoxide diffusion capacity (DLCO) were performed as required. BVAS was scored at every visit. The vasculitis damage index (VDI) [12] was scored at entry and then once every 6 months for 18 months. The Short-Form 36 functional questionnaire (SF-36) was also assessed at entry and then once every 6 months for 18 months. Adverse events were graded for severity according to predefined criteria, and their relationships to the trial medications were assessed.
Study end points
The primary end points were induction of remission at 6 months, and severe adverse events including death and ESRD. As secondary end points, the effectiveness and safety of the standard protocols, as well as health-related quality of life (HRQOL), were evaluated. With regard to the effectiveness, we evaluated time from initial treatment to remission; time from remission to relapse, if any; relapse rate; and VDI. With regard to safety and HRQOL, all adverse events and SF-36 were evaluated.
Statistical analysis
Quantitative variables were compared using Student’s t-test or the Mann–Whitney nonparametric test. Categorical variables were compared using the χ 2 test or Fisher’s exact test. In all analyses, P < 0.05 was taken to indicate statistical significance. Kaplan–Meier analysis was used to evaluate patient survival. SF-36 domain scores were calculated using the norm-based scoring algorithm, in which the scores were standardized to a mean of 50 and SD of 10 in the Japanese general population [13]. A one-sample t-test was used to determine whether the SF-36 domain scores of study subjects differed significantly from the Japanese general population norm. Repeated measures analysis of variance was used to test for changes with time in the SF-36 domain scores.
Results
Outcome of the study
Patients were enrolled in the study between July 2004 and September 2006. As illustrated in Fig. 1, 52 patients were screened, and 4 were excluded according to the criteria described above. The remaining 48 patients received the severity-based treatment: 2, 23, and 23 patients received treatment for the most severe, severe, and mild forms, respectively. One patient from the mild-form group was lost to follow-up within 6 weeks, and therefore the study population for further analysis consisted of the remaining 47 patients.
One patient in the severe-form group, with an RPGN type, started hemodialysis on day 4 and developed ESRD. Three patients died without remission, at 9 days, 2.5 months, and 3 months, respectively. At 6 months, 42 patients had achieved remission; 1, 20, and 21 of these patients were from the most severe form, severe form, and mild-form groups, respectively. One patient in the severe-form group died after achieving remission, without relapse, at 10 months. Eight patients showed relapse (3 and 5 from the severe-form group and the mild-form group, respectively). Among the relapsed patients, re-remission occurred in 7, while the remaining patient from the severe-form group died of sepsis due to opportunistic infection at 11 months. At the last observation, 32 patients had maintained remission without death or relapse; 1 in the most severe-form group, 15 in the severe-form group, and 16 in the mild-form group.
Baseline characteristics of patients
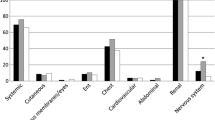
Patients were further stratified based on their organ involvement as described above. Table 1 shows the numbers of patients with each type and their baseline characteristics. One of the 2 patients in the most severe-form group had a cerebral bleeding type, and the other had resistant severe disease. No other types defined above were included in the most severe form group. RPGN type was most frequent among the severe-form group. The mean age of the patients was 66.6 years, and the majority of the patients (all except for two patients) ranged in age between 56 and 79 years. The patients were predominantly female. Males were more common in the severe-form group (52.2%) and much less common in the mild-form group (21.7%). In total, 75% of the patients showed renal involvement, and 45.8% showed pulmonary involvement.
The mean BVAS new/worse of the 48 patients enrolled in this study was 12.2 at baseline. The BVAS in the severe-form group was significantly higher than that in the mild-form group (P < 0.05). In the severe-form group, the generalized type showed the highest BVAS, followed by the pulmo-renal type, and the RPGN type.
The mean titer of MPO-ANCA at baseline was 423 EU/mL. The highest average titer was detected in the severe-form group; in the patients in this group, the RPGN type showed the highest average titer, followed by the generalized type, and the pulmo-renal type. PR3-ANCA was tested in 25 patients, all of whom showed negative results.
The mean serum creatinine level at baseline was 2.2 mg/dL. The highest average level was detected in the severe-form group; in these patients, the RPGN type showed the highest average level, followed by the pulmo-renal type, and the generalized type.
Time courses of changes in BVAS, MPO-ANCA, and serum creatinine
Figure 2a shows the time courses of changes in BVAS in the severe- and mild-form groups in the present study population. The scores declined rapidly during the first 6 weeks. However, even at 6 weeks, the mean BVAS in the severe-form group was significantly higher than that in the mild-form group (P < 0.05). The scores in the severe- and mild-form groups were increased at 6 months and thereafter, reflecting the 8 patients showing relapse described above. On the other hand, there were no significant differences in BVAS scores for persistent disease between the baseline and any other examination time points (data not shown). Among the forms, however, the BVAS persistent scores in the severe-form group were significantly higher than those in the mild-form group at all examination time points (data not shown).
Time courses of changes in the Birmingham vasculitis activity score (BVAS), myeloperoxidase-anti-neutrophil cytoplasmic antibodies (MPO-ANCA) titer, and serum creatinine. The mean values of a BVAS, b ANCA titers, and c serum creatinine in each group stratified according to severity are plotted at 6 weeks, 3 months, 6 months, 9 months, 12 months, 15 months, and 18 months. Open squares/solid lines and closed circles/dotted lines indicate severe- and mild-form groups, respectively. The data for the most severe-form group were omitted from the figure as this group included only a single patient
Figure 2b shows the time courses of changes in the MPO-ANCA titers in the severe- and mild-form groups. In both forms, the titer declined quickly during the first 6 weeks, and became negative at 9 months.
Figure 2c shows the time courses of changes in serum creatinine levels in the severe- and mild-form groups. In the severe-form group, the level decreased rapidly to 1.8 mg/dL during the first 6 weeks, and remained relatively constant thereafter. In contrast, the creatinine level in the mild-form group remained within the normal range throughout the observation period.
VDI
The mean ± SD VDI values at the baseline and at 18 months were 2.2 ± 2.1 (median 2, range 0–12) and 3.2 ± 2.9 (median 2, range 0–12), respectively. Compared with VDI values in the CYCAZAREM trial [7], where the mean VDI (95% confidence interval) values at baseline and at 18 months were 1.3 (1.0–1.6) and 2.5 (2.1–3.0), respectively, those in the present trial were higher by 0.9 and 0.7, respectively.
Both the baseline VDI and the VDI at 18 months were significantly higher in the severe-form group than in the mild-form group (P = 0.004 for baseline and P = 0.001 for 18 months). The baseline VDI in patients with remission (n = 42) was 1.71 ± 1.55, which was significantly lower than that in patients without remission (n = 5), 2.61 ± 1.52 (P < 0.001).
The correlation between VDI and BVAS was studied. Patients with baseline BVAS persistent of ≥4 (n = 22) showed a significantly higher VDI (4.32 ± 3.70) at 18 months than those with BVAS persistent of <4 (n = 25), in whom VDI was 2.29 ± 1.61 at 18 months (P = 0.024). However, there was no significant correlation between VDI and BVAS new/worse (data not shown). Therefore, the baseline value of BVAS persistent seemed to be important for indicating organ damage during the course of treatment of AVV.
SF-36
Of the 48 patients enrolled in the study, 32 had completed the SF-36 questionnaire at baseline. The mean norm-based scores for SF-36 domains at baseline were significantly lower than the Japanese general population norm. The lowest value (mean ± SD) was found in physical functioning (27.3 ± 18.9), followed by role physical (31.5 ± 15.3), role emotional (37.4 ± 15.3), social functioning (39.0 ± 13.8), general health (41.5 ± 10.5), and mental health (43.9 ± 11.2). Patients with remission showed significant improvements in all SF-36 domains, except for general health and role emotional. The physical components had improved significantly but remained considerably impaired at the 18-month follow-up, whereas the mental components approximated to the Japanese general population norm by 6 months.
Remission
As described above, 42 patients achieved remission. As illustrated in Fig. 3a, the majority of patients (n = 36) had achieved remission by the first 6 weeks, followed by 6 patients within 3 months, and the last patient by 6 months. The overall remission induction rate was 89.4% (42/47).
Kaplan-Meier estimates of time to remission induction, survival, and relapse. a Time to remission induction within 6 months after the start of treatment. The vertical axis indicates the percentage of patients with remission among 47 patients receiving predefined treatment protocols. b Survival during the 18-month observation period. The vertical axis indicates the percentage of patients who survived among 47 patients receiving predefined treatment protocols. c Time from remission to relapse. The vertical axis indicates the percentage of relapse-free patients among 42 patients who achieved remission. The horizontal axes indicate time from the start of treatment in a and b, and time from remission in c
Table 2 presents a summary of the remission induction therapy employed in each form/type of patient. All patients received oral prednisolone, with a mean initial dose of 37.5 mg/day. The highest and lowest mean initial doses were observed in the generalized type of the severe form and the pulmonary-limited type of the mild form, respectively. Sixteen patients received only glucocorticoid without any immunosuppressive agents (7 of 23 patients in the severe-form group and 9 of 23 patients in the mild-form group). Six of 16 patients with the RPGN type and 3 of 6 patients with the pulmonary-limited type received no additional immunosuppressive agents.
Death and ESRD
A total of 5 patients died in this prospective study. As shown in Fig. 3b, death occurred at 9 days, 2.5 months, 3 months, 10 months, and 11 months after the start of the treatment in these 5 patients. Of the 5 deaths, only one was considered to be disease-associated; this death occurred on day 9 in a patient with the most severe form, cerebral bleeding type, despite intensive treatment including high-dose glucocorticoid and intravenous cyclophosphamide, but no plasmapheresis. In the 4 remaining patients who died the disease was the severe form in 3 and mild form in 1. Two patients died after remission: one due to opportunistic infection, and the other due to pulmonary failure, presumably associated with Pneumocystis jirovecii pneumonia (PCP). The remaining two patients died without remission, at 2.5 and 3 months: one due to cerebral hemorrhage as an atherosclerotic event and the other due to interstitial lung disease of undetermined origin. In this trial, one patient with severe form, RPGN type, underwent hemodialysis on day 4 and developed ESRD despite high-dose glucocorticoid therapy.
Relapse
Table 3 shows the remission-maintenance therapy administered in the 42 patients after achieving remission. Thirty patients (71.4%) received only glucocorticoid, and the remaining 12 patients also received immunosuppressive agents: 5 patients received intravenous cyclophosphamide and 5 received azathioprine. Relapse occurred in 8 of the 42 patients (relapse rate = 19.0%); relapse occurred in 3 of 20 patients with the severe form (relapse rate = 15.0%), but 5 cases of relapse occurred among the 21 patients with the mild form (relapse rate = 23.8%). Of the latter 5 relapses, 4 occurred in 17 patients who received no immunosuppressant. As shown in Fig. 3c, all relapses occurred between 12 and 30 weeks after the induction of remission. The relapse group had significantly higher BVAS new/worse values at 6 months than the non-relapse group (3.75 ± 5.78 vs. 0.125 ± 0.554, respectively; P = 0.0001). However, there was no significant difference in BVAS persistent values between the relapse and non-relapse groups (3.75 ± 3.73 vs. 3.34 ± 2.72, respectively). There were no significant differences in several serological markers, such as CRP and ANCA titers, between the relapse and non-relapse groups (data not shown).
Adverse events
During the 18-month observation period, 29 events of infection of grade 3 or higher were observed. Among these, bacterial infection was noted in 11 events (10 patients): 8 events were grade 3, 2 were grade 4, and the remaining 1 was grade 5. Fungal infection was observed in 6 events (5 patients): 3 cases of aspergillosis and 3 cases of candidiasis (1 patient developed both aspergillosis and candidiasis). Of these 6 events, 3 were associated with aspergillus pneumonia without prophylactic antifungal agents. In total, however, fungal infection was observed in 1 of 13 patients with prophylaxis and 4 of 35 without prophylaxis (no significant difference, P > 0.05).
There were 7 viral infection events (in 7 patients): 4 with varicella-zoster virus (VZV), 2 with cytomegalovirus (CMV) (1 encephalitis and 1 positive antigenemia), and 1 with hepatitis C virus (HCV) (the hepatitis occurred in an HCV carrier). All patients with VZV developed herpes zoster and one patient with CMV developed encephalitis while receiving cyclophosphamide.
There were 3 PCP events (in 3 patients). Of the 48 patients enrolled in this study, 31 received prophylactic trimethoprim-sulfamethoxazole (TMP-SMX), while the remaining 17 did not. Two patients with PCP did not receive prophylaxis, and the other patient developed PCP 2 months after prophylaxis was stopped due to liver damage. Thus, no patients who received prophylaxis developed PCP.
Other adverse events included diabetes mellitus (9 events), bone fracture (3 events), cerebral vascular events (3 events), and cardiac vascular event (1 event). Two of the cerebral vascular events were of grade 5.
Discussion
We performed a prospective, open-label, multicenter trial (JMAAV) to evaluate the usefulness of a severity-based regimen for Japanese patients with MPO-ANCA-associated vasculitis. In this trial, patients were stratified into 3 severity groups and 12 disease types, and then received predetermined severity- and type-based protocols. These protocols were designed to choose an appropriate treatment regimen and to promote prediction of the outcome for each patient. The rates of remission, death, ESRD, and relapse obtained in the trial were comparable to those reported previously in European RCTs [7, 8] with minor differences. Thus, tailor-made treatment based on patients’ disease severity and disease type seemed to be useful in determining treatment regimens. The validity of the stratification we used, however, is also a matter of investigation in that it is related to other severity-based classifications, such as the five-factor score used by the French study group [14, 15].
Another finding of this trial was the concept of pulmonary-limited vasculitis. To date, the only organ-limited ANCA-associated vasculitis has been renal-limited vasculitis [16]. Six patients with only pulmonary involvement were included in the JMAAV trial. These patients were positive for MPO-ANCA, and showed interstitial lung disease without other major organ involvement. It may be possible to designate this type as pulmonary-limited vasculitis, another type of organ-limited vasculitis. As renal-limited vasculitis includes a wide spectrum of renal damage, from mild glomerulonephritis to RPGN, pulmonary-limited vasculitis may also include pulmonary lesions of varying severity. Further prospective studies are required to clarify these points.
Recently, the British Society of Rheumatology (BSR)/British Health Professionals in Rheumatology (BHPR) and the European League Against Rheumatism (EULAR) issued guidelines and recommendations, respectively, dividing patients with ANCA-associated vasculitis into 3 (localized/early systemic, generalized, and severe) [17] and 5 categories (localized, early systemic, generalized, severe, and refractory) [18], respectively, and recommended category-based treatment. These recommendations were based on several RCTs dealing with large numbers of patients with WG, and therefore caution is required in applying them to Japanese patients with MPO-ANCA-associated vasculitis. However, these recommendations also referred to precise dose reduction of cyclophosphamide and adjunctive therapy including prophylaxis against opportunistic infections, which must also be considered in the treatment of Japanese patients.
In our trial, two cases of grade 4 and 1 case of grade 5 infection (death) were observed as treatment-related severe infections. All of these patients showed urinary tract infection by Escherichia coli, which occurred during remission-maintenance treatment with glucocorticoid and cyclophosphamide. Oral cyclophosphamide or azathioprine was indicated as an immunosuppressive agent during remission maintenance in the JMAAV protocol, but the agents were employed at the discretion of the attending physician. As the CYCAZAREM, WEGENT (Wegener’s granulomatosis-entretien trial) [19], and IMPROVE (international mycophenolate protocol to reduce outbreaks of vasculitides randomized trial) trials [20] have indicated that azathioprine is the best adjunctive immunosuppressant during maintenance treatment, the use of this agent for MPA patients should be analyzed in future trials. In addition, a tapering protocol was not determined in the JMAAV trial, and therefore the total amounts of glucocorticoid administered were greater than those outlined in the European recommendations (data not shown). This greater amount seemed to be associated with several glucocorticoid-associated adverse events, including infection.
Prophylaxis is another countermeasure to cope with opportunistic infection. In the JMAAV trial, prophylactic protocols such as the use of TMP-SMX for PCP and the use of antifungal agents for fungal infection were not precisely determined. Three patients without prophylaxis suffered from PCP, whereas there were no cases of PCP among patients with prophylactic TMP-SMX. This result indicated that TMP-SMX should be recommended to prevent PCP in future trials in Japan. Although there were no significant differences in the incidences of fungal infection between those who received and those who did not receive prophylactic antifungal agents, patients at high risk of severe pulmonary fungal infection should receive prophylactic antifungal agents.
The relapse rate in the JMAAV trial was 19%, which was higher than that in the MPA subgroup (8%) and as high as that in the WG subgroup (18%) in the CYCAZAREM trial [7]. In our trial, the relapse rate was highest in patients with the mild form, especially in those with the pulmonary-limited type (3 cases of relapse in 6 patients), followed by those with the renal-limited type (1 relapse in 3 patients). Although all patients in the CYCAZAREM trial were treated with oral cyclophosphamide as well as glucocorticoid to induce remission, the use of cyclophosphamide was not obligatory in our trial, especially in our regimen for patients in the mild-form group. This may explain the differences in relapse rates between the trials. Further prospective studies are required to evaluate whether cyclophosphamide and azathioprine may be essential for the induction and maintenance of remission, respectively, for a certain population of patients in the mild-form group.
Health-related quality of life (HRQOL) in our trial showed considerable deterioration in patients with MPO-ANCA-associated vasculitis before treatment. During 18 months of follow-up, there were significant improvements in all SF-36 domains, except for general health and role emotional, in patients who achieved and sustained remission during the follow-up period. Therefore, the development of more effective treatment strategies for MPO-ANCA-associated vasculitis may be required to achieve better HRQOL.
In conclusion, the first prospective trial for Japanese patients with MPO-ANCA-associated vasculitis, the JMAAV trial, revealed the usefulness of severity-based treatment, and indicated the possible disease entity of “pulmonary-limited vasculitis” as a type of organ-limited ANCA-associated vasculitis. To achieve better outcomes, we propose several points to improve the treatment protocol: i.e., a glucocorticoid-tapering protocol, the use of less toxic immunosuppressants such as azathioprine in remission-maintenance therapy, and intensive prophylaxis for PCP or profound fungal infection.
References
Jennette JC, Falk RJ. Clinical and pathological classification of ANCA-associated vasculitis: what are the controversies? Clin Exp Immunol. 1995;101(Suppl 1):18–22.
van der Woude FJ, Rasmussen N, Lobatto S, Wiik A, Permin H, van Es LA, et al. Autoantibodies against neutrophils and monocytes: tool for diagnosis and marker of disease activity in Wegener’s granulomatosis. Lancet. 1985;1(8426):425–9.
Falk RJ, Jennette JC. Anti-neutrophil cytoplasmic autoantibodies with specificity for myeloperoxidase in patients with systemic vasculitis and idiopathic necrotizing and crescentic glomerulonephritis. N Engl J Med. 1988;318(25):1651–7.
Suzuki Y, Takeda Y, Sato D, Kanaguchi Y, Tanaka Y, Kobayashi S, et al. Clinicoepidemiological manifestations of RPGN and ANCA-associated vasculitides: an 11-year retrospective hospital-based study in Japan. Mod Rheumatol. 2009;20(1):54–62.
Falk RJ, Gross WL, Guillevin L, Hoffman G, Jayne DR, Jennette JC, et al. Granulomatosis with polyangiitis (Wegener’s): an alternative name for Wegener’s granulomatosis. Ann Rheum Dis. 2011;70(4):704.
Hoffman GS, Kerr GS, Leavitt RY, Hallahan CW, Lebovics RS, Travis WD, et al. Wegener granulomatosis: an analysis of 158 patients. Ann Intern Med. 1992;116(6):488–98.
Jayne D, Rasmussen N, Andrassy K, Bacon P, Tervaert JW, Dadoniene J, et al. A randomized trial of maintenance therapy for vasculitis associated with antineutrophil cytoplasmic autoantibodies. N Engl J Med. 2003;349(1):36–44.
De Groot K, Rasmussen N, Bacon PA, Tervaert JW, Feighery C, Gregorini G, et al. Randomized trial of cyclophosphamide versus methotrexate for induction of remission in early systemic antineutrophil cytoplasmic antibody-associated vasculitis. Arthritis Rheum. 2005;52(8):2461–9.
Ozaki S. ANCA-associated vasculitis: diagnostic and therapeutic strategy. Allergol Int. 2007;56(2):87–96.
Koyama A, Yamagata K, Makino H, Arimura Y, Wada T, Nitta K, et al. A nationwide survey of rapidly progressive glomerulonephritis in Japan: etiology, prognosis and treatment diversity. Clin Exp Nephrol. 2009;13(6):633–50.
Flossmann O, Bacon P, de Groot K, Jayne D, Rasmussen N, Seo P, et al. Development of comprehensive disease assessment in systemic vasculitis. Ann Rheum Dis. 2007;66(3):283–92.
Exley AR, Bacon PA, Luqmani RA, Kitas GD, Gordon C, Savage CO, et al. Development and initial validation of the Vasculitis Damage Index for the standardized clinical assessment of damage in the systemic vasculitides. Arthritis Rheum. 1997;40(2):371–80.
Fukuhara S, Suzukamo Y. Manual of SF-36v2 Japanese version. Kyoto: Institute for Health Outcomes and Process Evaluation Research; 2004.
Guillevin L, Lhote F, Gayraud M, Cohen P, Jarrousse B, Lortholary O, et al. Prognostic factors in polyarteritis nodosa and Churg–Strauss syndrome. A prospective study in 342 patients. Medicine. 1996;75(1):17–28.
Guillevin L, Pagnoux C, Seror R, Mahr A, Mouthon L, Le Toumelin P. The Five-Factor Score revisited: assessment of prognoses of systemic necrotizing vasculitides based on the French Vasculitis Study Group (FVSG) cohort. Medicine. 2011;90(1):19–27.
Weidner S, Geuss S, Hafezi-Rachti S, Wonka A, Rupprecht HD. ANCA-associated vasculitis with renal involvement: an outcome analysis. Nephrol Dial Transpl. 2004;19(6):1403–11.
Lapraik C, Watts R, Bacon P, Carruthers D, Chakravarty K, D’Cruz D, et al. BSR and BHPR guidelines for the management of adults with ANCA associated vasculitis. Rheumatology (Oxford). 2007;46(10):1615–6.
Mukhtyar C, Guillevin L, Cid MC, Dasgupta B, de Groot K, Gross W, et al. EULAR recommendations for the management of primary small and medium vessel vasculitis. Ann Rheum Dis. 2009;68(3):310–7.
Pagnoux C, Mahr A, Hamidou MA, Boffa JJ, Ruivard M, Ducroix JP, et al. Azathioprine or methotrexate maintenance for ANCA-associated vasculitis. N Engl J Med. 2008;359(26):2790–803.
Hiemstra TF, Walsh M, Mahr A, Savage CO, de Groot K, Harper L, et al. Mycophenolate mofetil vs azathioprine for remission maintenance in antineutrophil cytoplasmic antibody-associated vasculitis: a randomized controlled trial. JAMA. 2010;304(21):2381–8.
Acknowledgments
This study was supported by a grant-in-aid from the Ministry of Health, Labor, and Welfare of Japan. We thank Professor Loic Guillevin, Department of Internal Medicine, Hôspital Cochin, Paris, for critical reading of the manuscript and advice. The physicians participating in this study other than the authors were as follows: K. Amano (Saitama Medical Center, Kawagoe), Y. Arimura (Kyorin University, Mitaka), K. Hatta (Tenri Hospital, Tenri), S. Ito (Tsukuba University, Tsukuba), H. Kikuchi (Teikyo University, Tokyo), E. Muso (Kitano Hospital, Osaka), H. Nakashima (Fukuoka University, Fukuoka), Y. Ohsone (Kawasaki Municipal Kawasaki Hospital, Kawasaki), and Y. Suzuki (Tokai University, Isehara). The other members of the JMAAV Study Group included H. Hashimoto (Department of Internal Medicine and Rheumatology, Juntendo University), A. Koyama (Department of Nephrology, Graduate School of Comprehensive Human Sciences, University of Tsukuba), S. Matsuo (Department of Nephrology, Nagoya University Graduate School of Medicine), and H. Kato (Division of Clinical Proteomics and Molecular Medicine, St. Marianna University Graduate School of Medicine).
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
For the JMAAV Study Group.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Ozaki, S., Atsumi, T., Hayashi, T. et al. Severity-based treatment for Japanese patients with MPO-ANCA-associated vasculitis: the JMAAV study. Mod Rheumatol 22, 394–404 (2012). https://doi.org/10.1007/s10165-011-0525-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10165-011-0525-5