Abstract
Based on the medical waste quantity and patient data during the corona virus disease 2019 (COVID-19) outbreak in China, this study used scenario analysis to quantitatively analyze the temporal and spatial evolution of medical waste generation during the pandemics. First, the results show that the estimated medical waste per capita reached 15.4 kg/day if only patients were considered in Scenario 1, while the figures were reduced to 3.2 kg/day in Scenario 2 and 2.5 kg/day in Scenario 3 when the effects of both the patient type and the number of medical staffs were considered. The estimated results also demonstrated that the per capita medical waste related to the epidemic showed the characteristics of a U-shaped and trailing phenomenon over time. Then, the amount of medical waste related to the COVID-19 generated that generated due to COVID-19 was estimated in Hubei, Heilongjiang, Zhejiang, Henan and Hunan provinces under Scenario 2 and Scenario 3. The results indicated that the spatiotemporal evolution characteristics of five provinces show the significant differences, and the patient type has a remarkable influence on the generation of medical waste. Finally, a novel decomposition-ensemble approach was designed to make a better short-term forecasting effect for future medical waste generation in different provinces.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Medical waste generally could be divided into two categories: non-hazardous waste and hazardous waste, of which about 15% is hazardous waste that may be infectious, chemical or radioactive [1]. Although the proportion of hazardous medical waste is not large, its harm is significant. It may infect hospital patients, health workers and the public, and even adversely affect the ecological environment [1]. Given this, more and more attention has been paid to the research on the factors affecting medical waste. The report of the World Health Organization (WHO) showed that the average hospital bed in high-income countries generates up to 0.5 kg of hazardous waste per day, while the average in low-income countries generates 0.2 kg per day [1]. Su and Chen [2] also concluded that income would have a positive impact on the generation of medical waste. According to the results of Tesfahun et al. [3], the generation rate of medical waste has a strong linear correlation with the number of inpatients and a weak linear correlation with the number of outpatients. Minoglou and Komilis [4] concluded that CO2 emissions and life expectancy at birth were positively correlated with the rate of medical waste generation. Cheng et al. [5] pointed out that insurance reimbursement and the number of beds were the main factors affecting the generation of infectious waste. Windfeld and Brooks [6] found that the increase in GDP and medical expenditure led to higher generation of healthcare waste based on the linear regression models. Minoglou et al. [7] observed that the life expectancy, the human development index, the mean years of education and the CO2 emissions had a positive impact on the rate of the healthcare waste generation. It is important to note that the above results focus on the impact of general socio-economic factors on the generation of medical waste, but ignore the impact of the outbreak of public health emergencies [8], such as severe acute respiratory syndrome (2003), the Marburg hemorrhagic fever (2007), H1N1 influenza (2009), the Ebola virus (2014), and the Middle East respiratory syndrome coronavirus (2014) [9].
Coronavirus disease (COVID-19) is the third major pandemic caused by a virus in the past two decades [10], with a total of 2397,217 confirmed cases and 162,956 deaths worldwide as of 21 April 2020 [11]. By mid-March 2021, COVID-19 had struck almost every country in the world, with about 122 million confirmed cases and about 2.7 million deaths [12]. At the same time, countries have reported to whom more than 35,000 health workers infected with COVID-19 [13]. This pandemic has led to a sudden increase in demand for personal protective equipment such as gloves, masks, and many other essential items [14], which may lead to explosive growth in the generation of hazardous medical waste and pose severe challenges to its disposal. In December 2019, several cases of COVID-19 had been reported in Wuhan, China [9], and then gradually spread across the country. In order to effectively manage medical waste related to COVID-19 in China, those waste, including medical waste and household garbage, shall be collected separately by a medical institution in the diagnosis and treatment of COVID-19 patients and suspected patients with fever in outpatient clinics and wards [15]. According to the latest data from the Ministry of ecology and environment, PRC., as of April 25, 2020, the national capacity of medical waste disposal was 6,122.8 tons/day, an increase of 1,220.0 tons/day over 4,902.8 tons/day before the epidemic. Among them, the ability of Hubei from before the outbreak of 180.0 tons/day increased to 658.4 tons/day, Wuhan’s capacity increased from 50.0 tons/day up to 280.1 tons/day, Mudanjiang’s capacity increased from 8.0 tons/days to 18.5 tons/day [16]. As it turns out, the epidemic has had a significant impact on the disposal capacity of medical waste in different regions.
Considering that estimating and forecasting the amount of medical waste generated in advance could help optimize medical waste management systems, develop guidelines and assess mainstream medical waste treatment and disposal [3], various achievements have been obtained. Patwary et al. [17] estimated the medical waste generated in Dhaka was 37 ± 5 tons per day via statistical sampling method. Komilis et al. [18] discussed the wastes generated in different medical institutions in Greece. They found that the infectious/toxic and toxic medical wastes accounted for 10 and 50% respectively of the wastes generated by the public cancer treatment and university hospitals. Maamari et al. [19] analyzed the amount of medical waste produced by 57 of Lebanon’s 163 hospitals over five years, and the results showed that large private hospitals produced an average of 2.5 kg per occupied bed−1 day−1, while other categories produced an average of 0.9 kg per occupied bed−1 day−1. Karpusenkaitė et al. [20] used Lithuania’s annual medical waste data to evaluate various mathematical models such as artificial neural networks, multiple linear regression, and support vector machines in predicting the amount of medical waste, and the results showed that kernel regression method performed best. Komilis et al. [21] estimated that the private medical microbiology laboratories in Greece might generate about 580 tons of infectious medical waste each year. Korkut [22] estimated the annual total amount of medical waste in hospitals and other healthcare institutions based on data from the medical waste collection, treatment and disposal facilities in Istanbul, Turkey, over the past 18 years. Parida et al. [23] pointed out that, on average, biomedical waste generation rates in high-income countries generally range from 2 to 4 kg/bed/day, lower than the 4 to 6 kg/bed/day in upper–middle and lower–middle income countries. However, epidemic outbreaks usually could lead to a dramatic increase in infections in a very short period [9], making it difficult to estimate the per capita medical waste related to the epidemic by traditional methods of long-term sampling. Although Yang et al. [24] directly calculated the amount of medical waste per capita related to COVID-19 and discussed different strategies for medical waste disposal in Wuhan, they ignored the impact of different proportions of patients and medical staff.
Thus, this study intends to estimate the per capita medical waste related to the COVID-19 in China via scenario analysis based on the published data at the national level, considering the patient structure in China as the typical subjects, estimating the generation of their COVID-19 related medical waste, and the spatiotemporal evolution characteristics under different scenarios are also discussed. Finally, inspired by the principle of “decomposition ensemble”, a novel approach titled HP–ESM by integrating the Hodrick–Prescott filter (HP) algorithm and Exponential Smoothing Model (ESM) is proposed for predicting the future trend of medical waste in different provinces.
Methods
Scenario analysis
Scenario analysis, a process of analyzing future events by considering other possible outcomes, has been widely used in waste management [25]. Geng et al. [26] designed four different scenarios to simulate and evaluate Kawasaki’s innovative waste management initiative. Ferri et al. [27] introduced six scenarios to validate the reverse logistics network for the municipality of São Mateus. Seng et al. [28] carried out five scenarios to discuss the benefits of organic waste recycling. Ripa et al. [29] proposed three scenarios based on the source separation extent and destination of waste for treatment to identify the weak links in the waste management chain and to test the influence of potential improvements. Kosai et al. [30] set up three different scenarios to estimate the amount of e-waste produced in Vietnam to solve the uncertainty of the life cycle of electronic products. We can see that researchers have used scenario analysis to produce positive results in the prediction of waste generation in future phases that are full of uncertainties. This indicates that the tool of scenario analysis can be widely used in the estimation of multiple types of waste and shows a good performance. Therefore, three scenarios were set up in order to adequately describe and analyze the situation of medical waste in the future period. Since the medical waste associated with the outbreak is mainly generated by patients and medical staff, three different scenarios are designed to estimate the amount of medical waste per capita in this study. Scenario 1 (direct assessment) is that in which only the waste generated by patients with different levels of illness is considered. When there is a shortage of medical resources, it will affect the proportion of patients in charge of medical staff and the scheduling time. We thus set up Scenario 2 and Scenario 3, which correspond to the two scenarios of inadequacy and sufficiency, respectively.
Scenario 1: Direct estimation
This is a scenario in which all medical waste associated with the outbreak is generated by patients. In this study, six different patient types are considered, including existing confirmed cases (ECc), existing suspected cases (ESc), severe cases (Sc), medical observation cases (MOc), death cases (Dc), cured cases (Cc) and asymptomatic infected cases (AIc). The six patient types we have established are derived from the statistics of the Chinese government's public health department for the latest situation of the corona pneumonia outbreak on that day [31].
The amount of medical waste produced is not only related to patients, but also the waste generated by the rotation of medical staff during the outbreak. According to the survey conducted by the Institute of Asclepius Hospital Management, medical staff worked 8.2 h a day on average during the epidemic period, with 81.5% working more than 8 h and 5.7% working more than 12 h [32]. So, Scenario 2 and Scenario 3 are designed based on the working hours of medical staff.
Scenario 2: Inadequate medical resources
This is a scenario in which the working hours of medical staff have to be extended due to the shortage of medical resources. In this situation, it is reasonable to assume that the medical staff rotates every 12 h, moreover, for different types of patients with different proportions of medical staff.
Scenario 3: Sufficient medical resources
This is a scenario in which the medical staff worked for eight hours due to sufficient medical resources. In this situation, it is reasonable to assume that the medical staff rotates three times a day. As in Scenario 2, for different types of patients with different proportions of medical staff.
Medical resources would normally be understood as the resources of goods used to provide medical services. In the context of an outbreak defined as a public health emergency, additional resources are often added to the treatment of patients, such as the need for protective clothing and disinfection supplies to deal with viral transmission measures, etc. As a result, when resources are scarce, medical staff often choose to reduce the frequency of rotations, which also results in longer hours for a single person. This is to ensure that patients are cared for while having the necessary hygienic protection for themselves. This is the reason for the different number of rotations of medical staff in Scenarios 2 and 3. In addition, the ratio of medical staff to individual patients differs due to the different medical treatments required for patients undergoing treatment and for patients who have died (see Table S3).
Exponential smoothing method
The exponential smoothing method has been the most popular forecasting method in business and industry since its introduction in the 1950s [33]. In this study, Holt’s linear exponential smoothing method (HESM), Brown’s linear exponential smoothing method (BESM) and damped trend exponential smoothing method (DESM) are mainly used.
(1) Holt’s linear method [33]
where lt denotes an estimate of the level of the series at time t and at denotes an estimate of the growth of the series at time t. ρ and σ* are two smoothing constants. A forecast of yt+h based on all the data up to time t is denoted by \(\widehat{y}_{t + h\left| t \right.}\). In the special case where ρ = σ*, Holt’s method is equivalent to “Brown’s double exponential smoothing”.
(2) Damped trend method [33]
The growth for the one-step forecast of yt+1 is θat, and the growth is dampened by a factor of θ for each additional future period. Further information about the ESM can be found in the work of Hyndman et al. [33].
HP–ESM method
The Hodrick–Prescott (HP) filter is a mathematical tool used in macroeconomics to separate long-term trends in a data series from short-term fluctuations [34, 35]. Given T observations on a variable yt, τt is the trend component, and the residual yt-τt is then commonly referred to as the business cycle component [34]. The tendency of the amount of medical waste could be decomposed through optimization:
where λ is a (nonnegative) smoothing parameter, and its default value of EViews 8 (λ = 100) is used in this study. Then, the ESM is used to predict both the trend component (smoothed series) and cycle component (cycle series), respectively. The final predicted results of medical waste can be obtained by summing up the prediction results of each component. Fig.S1. shows the implementation flowchart of the proposed HP–ESM method.
Results
Estimate of medical waste per capita related to COVID-19
Considering the shortage of direct statistical data on the per capita medical waste related to COVID-19 (i.e., MWRCV19), information on the total amount of MWRCV19 was collected from the Ministry of Ecology and Environment of the People’s Republic of China (http://www.mee.gov.cn/). In addition, data on COVID-19 related cases (CRCs), including ECc, ESc, Sc, MOc, Dc, Cc and AIc, were obtained from the Wind database. These data will be used to estimate the medical wastes in different scenarios. This section will estimate the amount of MWRCV19 per capita under three scenarios.
Scenario 1: Direct estimation
The amount of MWRCV19 has been disclosed irregularly since 11 February 2020, and the related information is shown in Table S1. As shown in Table S1, the amount of MWRCV19 shows a trend of increasing first and then decreasing continuously. On February 11, 489.0 tons of MWRCV19 were collected nationwide, accounting for 18.4% of the total medical waste collection. Then the volume of MWRCV19 had increased to 587.6 tons on February 24, accounting for 21.6% of the total medical waste collected in China. While data on March 3 showed that the amount of MWRCV19 was 17.2 tons less than that on February 24. Furthermore, the quantity on March 9 was 101.5 tons less than that on March 3. By April 25, the volume of MWRCV19 had dropped to 186.4 tons. During the same period, the total number of CRCs showed a continuous decline, from 240,745 cases on February 11 to 10,169 cases on April 25. To test the correlation between the total number of CRCs and the volume of MWRCV19, the Pearson correlation value is calculated, and the result is shown in Table S2. The conclusion shows that their Pearson correlation coefficient is 0.60*, which means a strong correlation [36].
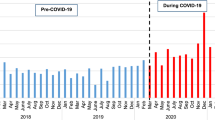
The estimated average per capita of MWRCV19 is 15.4 kg/day, and its trend is shown in Fig. 1. The per capita level of MWRCV19 rose first and then stabilized. As the total number of CRCs continues to decrease, the quantity of the per capita of MWRCV19 shows a trend of rapid growth between February 11th and March 9. It can be calculated from Table S1 that the total number of CRCs fell by an average of 46.6%, while the average decrease of the per capita of MWRCV19 is less than 1%. One possible reason is that with the steady progress of China’s fight against COVID-19, various medical-related enterprises have resumed work and production. Thus, the increasing supply capacity of medical supplies would also increase the amount of the per capita of MWRCV19. According to the data from 22 key provinces on February 10, the recovery rate of mask enterprises has exceeded 76%, and that of protective clothing enterprises is 77% [37]. Another possible reason is that the total number of CRCs has fallen rapidly, but the number of staff involved (i.e., doctors, nurses, police and so on) has not declined at the same time. News reports have shown that medical teams from different provinces supporting Hubei, such as Hunan, Jilin and Zhejiang, began leaving Wuhan in mid-March [38].
Meanwhile, Fig. 1 shows that since mid-March, the per capita of MWRCV19 has fluctuated at 19.6 kg/day, which may be affected by combining the following four factors. Firstly, the total number of CRCs continues to decrease. However, the resource (staff, equipment and so on.) input of medical institutions will maintain a certain scale in the short term to cope with emergencies that may occur at any time. In this case, the remaining CRCs could enjoy relatively abundant medical resources, producing more medical waste. Secondly, the amount of medical waste per capita is significantly larger, mainly because the medical resources (staff, equipment and so on.) that also produce medical waste invested in CRCs are not considered. For example, a critically ill patient needs six medical staff [39]. Thirdly, since March, the hospital has gradually returned to normal status, and a large number of suspected patients with fever and cough have been monitored, which also creates much medical waste [40]. Finally, with the effective suppression of the epidemic, more and more enterprises began to resume work and production, which has led to a huge demand for nucleic acid testing for COVID-19.
Scenario 2: Inadequate medical resources
In order to obtain more accurate estimates, Scenario 2 considers the correction of the denominator in terms of the number of medical staff and different types of cases under inadequate medical resources. Considering the high risk of severe cases in nursing care, its adjustment coefficient is determined according to four hours each time and six staff each shift [39]. The parameters of Dc and Cc are estimated by expert consultation. The medical staff of other types of patients refer to the standards for secondary general hospitals [41]. Based on Table S3 and Table S4, the adjusted total number of CRCs and the per capita of MWRCV19 can be calculated, and the results are shown in Table 1. Equation (8) is used to calculate the adjusted total number of CRCs.
Take the data of February 11 as an example to illustrate the calculation process.
Table 1 shows that the adjusted per capita of MWRCV19 is 3.2 kg/day, which is not much different from the one calculated by Nanjing Zhongchuan Oasis Environmental Protection Co., LTD [42]. Chen Jisai, a researcher and deputy general manager of the company, estimated that a patient generates about 1.5 kg–2.0 kg of pure medical waste a day. If medical waste generated by medical staff is added, it is possible to reach 3.2 kg/day. In this case, the estimated per capita of MWRCV19 based on Scenario 2 is more reliable than that based on Scenario 1. Similar to Scenario 1, the per capita of MWRCV19 also showed a characteristic of increasing first and then stable fluctuation. In addition, the Pearson correlation value is also calculated between the adjusted total number of CRCs and the volume of MWRCV19. The result shows that the correlation coefficient of Scenario 2 is larger (see Table 1) and more significant than that of Scenario 1, which indicates that it is necessary to consider the impact of both the medical staff and different types of patients when estimating the per capita of MWRCV19.
Scenario 3: Sufficient medical resources
When medical resources are abundant, medical staff could be rotated according to the normal shift system. In this case, the adjustment coefficients are determined, as shown in Table S5. It is easy to find that the estimated amount of the per capita of MWRCV19 in Scenario 3 is 2.5 kg/day, which is smaller than that in Scenario 2. The overall trend is similar to that of Scenario 2, and the per capita medical waste first increased and then fluctuated around 3.0 kg/day. Moreover, the Pearson correlation coefficient value in Scenario 3 is between Scenario 1 and Scenario 2. Although the significance is less than that of Scenario 2, it is still within the acceptable range. Meanwhile, the results indicate that there is still a strong correlation (0.69*) between the adjusted total number of CRCs and the volume of MWRCV19 in Scenario 3.
As can be seen from Table S5, since March 28, the average medical waste per capita is more than 3.0 kg/day, with an average of 3.6 kg/day. Based on the data in Table S4, it is not diffficult to find that the number of ECc has been declining rapidly since March 28, and the number of Sc has also decreased significantly. Especially, the reduction in the number of Sc has led to a decrease in the need for medical staff, which has reduced the denominator in which the per capita of MWRCV19 is estimated. At the same time, as analyzed in Scenario 1, with the medical institutions gradually returning to normal level, the monitoring demands of enterprises, schools and other patients (excluding CRCs) on COVID-19 are increasing, and the medical waste they produce is also contained in the numerator. So, under the combined influence of these factors, the estimated per capita medical waste did not reduce with the decrease in the number of CRCs. Furthermore, the estimated differences in the amount of medical waste per capita in Scenario 2 and Scenario 3 are diagnosed by the paired samples test, and the result is shown in Table S6. There is a significant difference between them (t = 4.649, Sig. = 0.001), reflecting the sensitivity of the results to parameters (i.e., adjusted coefficient). Therefore, it is necessary to estimate the amount of MWRCV19 in different scenarios.
The time evolution characteristics of medical waste generation related to the COVID-19
The empirical study shows that there is a significant linear relationship between the amount of medical waste generated and the factors such as the number of beds [22], income [2], and life expectancy [7].To analyze the time evolution characteristics of the amount of medical waste generated during the epidemic trend, it is necessary to find an appropriate model to fit the limited data. In this study, the total number of CRCs in Scenario 1, the adjusted total numbers of CRCs in both Scenario 2 and Scenario 3 are considered as independent variables. At the same time, the per capita of MWRCV19 is placed on the y axis. Based on the data in Table S1, Table 1 and Table S5, the Eqs. (9–11) in different scenarios are obtained via the polynomial fitting method, respectively. The coefficient of determination, denoted as R2, is used to select the order of the polynomial model. The closer the coefficient of determination is to 1, the better the model fitting degree is [22]. It is worth noting that the higher the order of the polynomial model could improve the value of R2, but it may lead to the overfitting problem. Therefore, under the rule of pursuing the maximum value of R2 and ensuring that the estimated value of medical waste per capita is not negative, the orders of the polynomial models in different scenarios are finally determined.
The R2 values of fitting polynomials obtained under the three scenarios are all greater than 0.9, indicating that the equations can be used to estimate the amount of medical waste per capita. Additionally, the R2 values in Scenario 2 and Scenario 3 are both greater than that in Scenario 1, which further verified that it is necessary to consider different types of patients and their medical staff allocation when estimating the amount of medical waste per capita. Then, Eq. (9) introduces the total number of CRCs from January 20 to May 1 in Scenario 1. The variation trend of medical waste per capita is estimated, and the result is shown in Fig. 2 (Scenario 1). Similarly, Fig. 2 (Scenario 2) and Fig. 2 (Scenario 3) can be obtained by using Eqs. (10 and 11) based on the adjusted total number of CRCs from January 20 to May 1, respectively.
In multiple scenarios (i.e., Scenario 1, Scenario 2, and Scenario 3) with patient and medical resources, we obtained the data for per capita medical waste: 15.4 kg/day for MWRCV19 in Scenario 1 with a patient factor only, 3.2 kg/day in Scenario 2 with inadequate medical resources, and 2.5 kg/day in Scenario 3 with sufficient medical resources. It can be seen that the data under Scenario 1 differ significantly from the corresponding values in Scenarios 2 and 3, due to the reduced fit resulting from the background assumptions of only establishing the patient factor and ignoring the situation of the medical resources. In the more densely populated India, this data is only 7.6 kg/day, which is about one-half of that in Scenario 1, despite the differences in medical practices [43]. In the several studies with some regions of Turkey, the MWRCV19 values are mostly in single digits, more similar to the values in Scenarios 2 and 3 [44, 45]. The degree of fit of the assumptions and parameter settings for these two scenarios is thus further established.
As shown in Fig. 2, the per capita medical waste related to the epidemic shows three main characteristics. In the first place, the per capita amount of medical waste associated with the epidemic showed a “U” shape over time. At the initial stage of the outbreak, medical resources were relatively abundant, and the amount of medical waste per capita was relatively large. However, with the rapid increase of the total number of CRCs, the medical resources will be extremely scarce in a short period, which will lead to a significant decline in the amount of medical waste per capita. As the epidemic is gradually under the effective control and the supply capacity of medical resources is further improved, the amount of medical waste per capita will show an upward trend. In the second place, the per capita amount of medical waste related to the epidemic showed an obvious trailing phenomenon. In other words, with the decrease of the total number of CRCs, the per capita medical waste related to the epidemic showed the characteristic of stable fluctuation around a specific value after a period of increase. The underlying reason may be that, as analyzed in Scenario 1, with the resumption of work and production, a large number of non-epidemic related cases will produce a certain amount of medical waste related to the epidemic [24]. In the third place, the trailing points of Scenario 2 and Scenario 3 appear later than that of Scenario 1, which may be derived from the consideration of different patient types, such as ECc, ESc, Sc, ESc, MOc, Dc, Cc, and AIc. According to the analysis of the original data, the total number of CRCs continued to drop from February 13 to March 21, while ECc, ESc and Sc declined persistently between 19 February and 10 April. So, perhaps it is for this reason that the trailing points of Scenario 2 and Scenario 3 were pushed back from March of Scenario 1 to April.
The spatiotemporal evolution of COVID-19 medical waste
In Sects. 3.1.1 and 3.1.4, we have analyzed and examined the results obtained for Scenario 1, respectively. We found that because Scenario 1 only considered the patient factors, the MWRCV19 data did not perform as well as Scenarios 2 and 3 for the simulation of the actual situation, although they also possessed a fit that met the criteria. This analysis is also consistent with the findings of other researchers in different regions: the average daily amount of medical waste generated from individual beds was typically in the single digits in multiple countries with different levels of epidemic development, which is much smaller than the 15.4 kg/day for MWRCV19 given in Scenario 1 [43,44,45].
Based on the above discussions, we believe that Scenario 2 and Scenario 3 may be consistent with the actual situation. To highlight the spatiotemporal evolution characteristics of medical wastes, those provinces with more than 1000 confirmed COVID-19 cases in China, including Zhejiang, Henan, Hunan, Hubei and Guangdong, can be selected for further investigation under different scenarios. Among them, Zhejiang and Guangdong are both coastal provinces with rapid economic development. Considering the data shortage of AIc in Guangdong, while Heilongjiang is an important overland route from Asia and the Pacific to Russia and Europe, we would like to collect relevant data of Heilongjiang for analysis in this section. In addition, the selected five provinces also have their unique geographical characteristics. Zhejiang is located on the southeast coast of China. Heilongjiang is located in the northeast of China, facing Russia across the river. Hubei that is located in central China, has the largest number of confirmed COVID-19. Meanwhile, Hunan and Henan provinces border Hubei.
The spatiotemporal evolution characteristics under Scenario 2
The amount of medical waste related to the epidemic in five provinces is estimated under Scenario 2, and the results are shown in Table S7 and Fig. 3. In general, the amount of medical waste associated with the epidemic presents three spatiotemporal evolution characteristics in five provinces. Firstly, different from the other four provinces, the changes in the medical waste amount in Hubei shows a unique characteristic, that is, the medical waste amount related to the epidemic increased first. It then declined with the decrease of the adjusted total number of CRCs. Secondly, in the context of the second outbreak of the epidemic, there has been a significant secondary increase in medical waste, such as in Heilongjiang and Zhejiang. Finally, with the effective control of the epidemic, the amount of medical waste has been on the decline, such as in Henan and Hunan.
Figure 3 shows that the volume of medical waste related to the epidemic in Hubei peaked at 553.5 tons on March 3, followed by a continuous decline. As of March 3, the daily disposal capacity of medical waste in Hubei province increased from 180 tons before the outbreak to 663.7 tons [46]. In this case, the amount of medical waste related to the epidemic would account for 83.4% of the total medical waste disposal capacity of Hubei. If 180 tons of general medical waste needs to be disposed of every day, plus medical waste at the peak of the epidemic, it is necessary for Hubei to increase its medical waste disposal capacity to 733.5 tons per day. Figure 3 indicates that since the end of March in Heilongjiang, the volume of medical waste related to the epidemic has increased rapidly, from 3.8 tons on March 28 to 47.2 tons on April 25, and the trend is still on the rise. From the available information, the capacity of medical waste disposal in Mudanjiang city in Heilongjiang increased from 8.0 tons per day before the outbreak to 18.5 tons per day [16], which means that the disposal capacity of medical waste in other parts of Heilongjiang should be far more than 28.7 tons/day. When the medical waste related to the epidemic accounted for 30% of the total medical waste at the peak, the medical waste disposal capacity of Heilongjiang should be 157.3 (47.2/0.3) tons per day. If the proportion is expected to be reduced to 20%, the daily handling capacity should be increased to 236.0 tons/day. The change of medical waste in Zhejiang showed a trend of decreasing first, then rising, and finally declining continuously. On February 11, the volume of medical waste related to the epidemic in Zhejiang was 20.7 tons, which gradually declined to 3.6 tons on March 3, but then increased to a peak of 40.5 tons on March 28. On April 25, the figure fell to 8.3 tons in Zhejiang. As shown in Fig. 3, Henan and Hunan, which are adjacent to Hubei, generated the most medical waste related to the epidemic during the outbreak stage. With the effective control of the virus, medical waste rapidly decreased. The amount of medical waste related to the epidemic in Henan dropped from 18.7 tons on February 11 to 0.4 tons on April 25, while that in Hunan fell from 12.3 tons to 0.02 tons.
The spatiotemporal evolution characteristics under Scenario 3
The estimated coronavirus related medical waste in Scenario 3 is the same as the spatiotemporal evolution characteristics of Scenario 2, see Fig. 4. However, it should be noted that in Scenario 3, the estimated amount of medical waste in each province is significantly different from that in Scenario 2. Compared with Scenario 2, the total amount of medical waste in Hubei province showed a decreasing trend, while Heilongjiang, Hunan, Henan and Zhejiang provinces showed a certain increase. Specifically, it is mainly due to the difference between the adjusted per capita of MWRCV19 and the adjusted total number of CRCs in different provinces. According to the calculation, the adjusted per capita of MWRCV19 in Scenario 3 is down by an average of 19.3% from Scenario 2. In contrast, on average, the adjusted total number of CRCs rose by only 16.8% in Hubei. In contrast, the adjusted total number of CRCs, averagely increased by 31.2% in Heilongjiang, 34.1% in Zhejiang, 34.9% in Henan, and 31.6% in Hunan. It is not difficult to find from Table S8 to Table S12 that the fundamental reason for the different results between Hubei and other provinces is the significant difference in patient structure. In particular, severe cases account for more than 40 percent in Hubei, while about 10 percent in Heilongjiang and even less in other provinces. Therefore, when estimating the amount of medical waste in different regions, it is necessary to consider the patient type in different regions.
Figure 4 shows that the amount of medical waste related to the epidemic in Hubei province was 537.8 tons on March 3, which is a reduction of 2.8% compared with the value of Scenario 2. Figure 4 shows that 47.9 tons of medical waste related to the epidemic was generated in Heilongjiang on April 25. Similarly, Fig. 4 shows that medical waste related to the outbreak in Zhejiang, Henan and Hunan provinces peaked at 43.7, 19.7 and 13.0 tons on March 28, February 11 and February 11, respectively. Thus, in Scenario 3, assuming that the medical waste related to the epidemic accounted for 30% of the total medical waste, the disposal capacity of medical waste in Hubei, Heilongjiang, Zhejiang, Henan and Hunan should reach 1792.7 tons/day, 159.6 tons/day, 145.6 tons/day, 65.6 tons/day and 43.3 tons/day, respectively. Considering that Hubei is the province with the most serious epidemic situation in China, the proportion of medical waste related to the epidemic of the total medical waste could be adjusted to 80%, so the revised daily treatment capacity of medical waste in Hubei should be 672.3 tons/day.
The prediction of the spatiotemporal evolution of COVID-19 medical waste
Aiming to predict the future trend of medical waste related to the epidemic under Scenario 3, 8 sample data from March 14 to April 25 are used for modeling. The specific data is shown in Table S13. Since the amount of medical waste associated with the outbreak in Henan and Hunan after April 25 is much less than 1.0 ton, we will focus on the future trends in Hubei, Heilongjiang and Zhejiang. The training sample and test sample are selected according to the principle of 8:2; that is, the training sample data from March 14 to April 11 and the data from April 18 to April 25 is used as the test sample. To evaluate the forecasting performance of our proposed HP–ESM method, three univariate models including BESM, HESM, and DESM are used as benchmark models. In these models, ESM can be implemented using SPSS Statistics V25.0, and Hodrick–Prescott filter can be conducted in EViews 8. The performance evaluation results, including the sum of square error (SSE), mean absolute error (MAE), mean absolute percentage error (MAPE), root mean square error (RMSE) and R2 of different models, are shown in Table S14. The metrics in Table S14 and Table S15 show that the HP–ESM approach has better performance. Then, the HP algorithm is used to decompose 8 sample data from March 14 to April 25, and each component is modeled by ESM. The predicted results are shown in Fig. 5.
It is not difficult to find from Fig. 5 that, as time goes on, the amount of medical waste in Hubei and Zhejiang shows a rapid decline, while that in Heilongjiang increased significantly. If the outbreak in Heilongjiang is not brought under control, the daily output of medical waste related to the epidemic will reach 70.6 tons by May 16. As Heilongjiang is adjacent to Russia, the epidemic situation in Russia has become increasingly severe recently, which makes the development trend of the epidemic in Heilongjiang more uncertainty. As of April 13, a total of 322 confirmed cases and 38 asymptomatic infected persons had been reported from Suifenhe port [47]. Therefore, for Heilongjiang, medical waste disposal facilities should be planned to improve the daily treatment capacity to cope with the possible sudden and rapid growth of medical waste.
Conclusions
In this study, COVID-19 was taken as an example to discuss the impact mechanism of public health emergencies on the generation of medical waste. Three different scenarios were set to estimate the per capita medical waste related to the COVID-19 based on the data released by China. The results showed that the per capita medical waste related to the epidemic showed a unique pattern, that is, the U-shaped and trailing phenomenon over time. Then, the medical waste related to the epidemic was also estimated in Hubei, Heilongjiang, Zhejiang, Henan and Hunan provinces under different scenarios, and the corresponding result indicates that the structure of patients and shift frequency of medical staff have a significant influence on the generation of medical waste. The five experimental results also show that the HP–ESM method proposed in this study is better than the ESM method alone, which means that the method has the advantage of short-term prediction of future medical waste quantity. In fact, the HP–ESM method has the same modeling idea as that in literature [48,49,50], which are all based on the characteristics of the existing time series for predictive modeling. Therefore, for diseases with different infectious rates, it is necessary to re-estimate the model parameters to describe the spread trend of different infectious diseases.
However, the limitation of this study is that it only considers the medical staff, but not the policemen, volunteers, government workers and other staff working on the front line of the fight against the epidemic, which would make the result overestimate. In addition, only ESM is considered as a prediction method and it is not sufficient for prediction tasks. There are many excellent single models, such as artificial neural networks, linear regression, support vector machines, and gray prediction model, which could be considered to combine with the HP algorithm to further improve the accuracy of medical waste quantity prediction. All these questions deserve further study and discussion in the future.
References
World Health Organization (WHO). Health-care Waste. 2018 [cited 2020 4.25]; Available from: https://www.who.int/en/news-room/fact-sheets/detail/health-care-waste
Su ECY, Chen YT (2018) Policy or income to affect the generation of medical wastes: an application of environmental Kuznets curve by using Taiwan as an example. J Clean Prod 188:489–496
Tesfahun E, Kumie A, Beyene A (2016) Developing models for the prediction of hospital healthcare waste generation rate. Waste Manage Res 34(1):75–80
Minoglou M, Komilis D (2018) Describing health care waste generation rates using regression modeling and principal component analysis. Waste Manage 78:811–818
Cheng YW et al (2009) Medical waste production at hospitals and associated factors. Waste Manage 29(1):440–444
Windfeld ES, Brooks MS-L (2015) Medical waste management–A review. J Environ Manage 163:98–108
Minoglou M, Gerassimidou S, Komilis D (2017) Healthcare waste generation worldwide and its dependence on socio-economic and environmental factors. Sustainability 9:2
Zhang HW et al (2020) Corona virus international public health emergencies: implications for radiology management. Acad Radiol 27(4):463–467
Yu H et al (2020) Reverse logistics network design for effective management of medical waste in epidemic outbreaks: insights from the coronavirus disease 2019 (COVID-19) outbreak in Wuhan (China). Int J Environ Res Public Health 17:5
Anand U et al (2022) SARS-CoV-2 and other pathogens in municipal wastewater, landfill leachate, and solid waste: A review about virus surveillance, infectivity, and inactivation. Environ Res 203:111839
World Health Organization (WHO). WHO calls for healthy, safe and decent working conditions for all health workers amidst the COVID-19 pandemic. 2020 [cited 2020 5.20]; Available from: https://www.who.int/news-room/detail/28-04-2020-who-calls-for-healthy-safe-and- decent-working- conditions- for-all-health-workers-amidst-covid-19-pandemic
Elsaid K et al (2021) Effects of COVID-19 on the environment: an overview on air, water, wastewater, and solid waste. J Environ Manage 292:112694
World Health Organization (WHO). Situation report—92, Coronavirus disease 2019 (COVID-19), 21 April 2020. 2020 [cited 2020 5.20]; Available from: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200421-sitrep- 92-covid-19.pdf?sfvrsn=38e6b06d_8
Iyer M et al (2021) Environmental survival of SARS-CoV-2–a solid waste perspective. Environ Res 197:111015
National Health Commission, PRC. Notification on the management of medical waste in medical institutions during coronavirus disease 2019 outbreak. 2020 [cited 2020 5.20]; Available from: http://www.nhc.gov.cn/yzygj/s7659/202001/ 6b7bc23a44624ab28 46b127d146be758.shtml
Ministry of ecology and environment, PRC. The ministry of ecology and environment reported on the disposal of medical waste, medical sewage and environmental monitoring. 2020 [cited 2020 5.20]; Available from: http://www.mee.gov.cn/xxgk2018/xxgk/ xxgk15/202004/t20200427_776588.html
Patwary MA et al (2009) Quantitative assessment of medical waste generation in the capital city of Bangladesh. Waste Manage 29(8):2392–2397
Komilis D, Fouki A, Papadopoulos D (2012) Hazardous medical waste generation rates of different categories of health-care facilities. Waste Manage 32(7):1434–1441
Maamari O et al (2015) Health care waste generation rates and patterns: the case of Lebanon. Waste Manage 43:550–554
Karpusenkaite A, Ruzgas T, Denafas G (2016) Forecasting medical waste generation using short and extra short datasets: case study of Lithuania. Waste Manage Res 34(4):378–387
Komilis D, Makroleivaditis N, Nikolakopoulou E (2017) Generation and composition of medical wastes from private medical microbiology laboratories. Waste Manage 61:539–546
Korkut EN (2018) Estimations and analysis of medical waste amounts in the city of Istanbul and proposing a new approach for the estimation of future medical waste amounts. Waste Manage 81:168–176
Parida VK et al (2022) An assessment of hospital wastewater and biomedical waste generation, existing legislations, risk assessment, treatment processes, and scenario during COVID-19. J Environ Manage 308:114609
Yang L et al (2021) Emergency response to the explosive growth of health care wastes during COVID-19 pandemic in Wuhan, China. Resour, Conserv and Recy 164:105074
Allesch A, Brunner PH (2014) Assessment methods for solid waste management: a literature review. Waste Manage Res 32(6):461–473
Geng Y, Tsuyoshi F, Chen XD (2010) Evaluation of innovative municipal solid waste management through urban symbiosis: a case study of Kawasaki. J Clean Prod 18(10–11):993–1000
Ferri GL, Chaves GDD, Ribeiro GM (2015) Reverse logistics network for municipal solid waste management: The inclusion of waste pickers as a Brazilian legal requirement. Waste Manage 40:173–191
Seng B et al (2013) Scenario analysis of the benefit of municipal organic-waste composting over landfill Cambodia. J Environ Manag 114:216–224
Ripa M et al (2017) The relevance of site-specific data in life cycle assessment (LCA). The case of the municipal solid waste management in the metropolitan city of Naples (Italy). J Clean Product 142:445–460
Kosai S, Kishita Y, Yamasue E (2020) Estimation of the metal flow of WEEE in Vietnam considering lifespan transition. Resour Conserv and Recy 154:104621
National Health Comission of the People's Republic of China. Update on the Corona virus pneumonia outbreak as of 24:00 on August 13. 2020 [cited 2020 8.14]; Available from: http://www.nhc.gov.cn/cms-search/xxgk/getManuscriptXxgk.htm?id=24faef5f4c154984ab9234363e93a368
Institute of Asclepius Hospital Management. Health care workers’ work stress and psychological status under covid-19 outbreak. [cited 2020 4.25]; Available from: https://www.sohu.com/a/376969753_389597
Hyndman R et al (2008) Forecasting with exponential smoothing: the state space approach. Springer, Berlin, Heidelberg
Ravn MO, Uhlig H (2002) On adjusting the Hodrick-Prescott filter for the frequency of observations. Rev Econ Stat 84(2):371–376
de Jong RM, Sakarya N (2016) The econometrics of the Hodrick-Prescott filter. Rev Econ Stat 98(2):310–317
Yang J, Guo YQ, Zhao WL (2019) Long short-term memory neural network based fault detection and isolation for electro-mechanical actuators. Neurocomputing 360:85–96
China Economic Net. Multiple departments introduced the resumption of work and production of enterprises to actively and steadily promote the “two-line” operation. 2020; Available from: http://news.china.com.cn/live/2020-02/12/content_701252.htm
CCTV Net. Support Hubei medical teams from all over the country have returned, and friendship forever. 2020 [cited 2020 4.25]; Available from: http://jiankang.cctv.com/2020/03/23/ ARTIJFhgH3hQNaYmzru ZPN9f200323. shtml
National Health Commission, PRC. Care practices for severe and critical covid-19 patients. 2020 [cited 2020 4.25]; Available from: http://www.nhc.gov.cn/xcs/zhengcwj/202003/ 8235a35f35574ea79cdb7c261b1e666e.shtml
National Health Commission, PRC. Notification on further consolidating the achievements and improving the prevention, control and treatment capacity of covid-19 in medical institutions. 2020 [cited 2020 4.25]; Available from: http://www.nhc.gov.cn/yzygj/ s7659/202004/9ceeac520d944e1a94301d06d1e9dcce.shtml
National Health Commission, PRC. Basic standards for medical institutions (trial). 1994 [cited 2020 4.25]; Available from: http://www.nhc.gov.cn/ewebeditor/uploadfile/2017/06/2017 0614162520548.docx
Modern Express. Practical investigation of medical waste disposal in Wuhan, ‘vehicled’ cabin is about to leave for Huoshenshan Hospital. [cited 2020 4.25]; Available from: https://xw.qq.com/cmsid/20200220A0SFPO00
Gowda NR et al (2021) War on waste: Challenges and experiences in COVID-19 waste management. Disaster Med Public 1–5
Hanedar A et al (2022) The impact of COVID-19 pandemic in medical waste amounts: a case study from a high-populated city of Turkey. J Mater Cycles Waste Manage 24(5):1760–1767
Kalantary RR et al (2021) Effect of COVID-19 pandemic on medical waste management: a case study. J Environ Health Sci Eng 19(1):831–836
Ministry of ecology and environment, PRC. National treatment and disposal of medical wastewater in a stable, orderly and strict implementation of disinfection measures. 2020 [cited 2020 4.28]; Available from: http://www.mee.gov.cn/ywdt/ hjywnews/ 202003/t20200312_768680.shtml
Minnan Network. Why is Suifenhe so serious? How are imported cases infected? 2020 [cited 2020 4.28]; Available from: http://www.mnw.cn/news/shehui/2271450.html
Arora P, Kumar H, Panigrahi BK (2020) Prediction and analysis of COVID-19 positive cases using deep learning models: A descriptive case study of India. Chaos, Solitons & Fract 139:110017
Hernandez-Matamoros A et al (2020) Forecasting of COVID19 per regions using ARIMA models and polynomial functions. Appl Soft Comput 96:106610
Khan FM, Gupta R (2020) ARIMA and NAR based prediction model for time series analysis of COVID-19 cases in India. J Safety Sci Resil 1(1):12–18
Funding
This work was supported by the National Natural Science Foundation of China [Grant No. 72001165]; Shaanxi Province Innovation Capacity Support Program [Grant No. 2022SR5016]; Major Theoretical and Practical Research Project of Philosophy and Social Sciences in Shaanxi Province [Grant No. 2022ND0389].
Author information
Authors and Affiliations
Contributions
FW: methodology, simulation, data collection, visualization, writing-original draft preparation; LY: conceptualization, methodology, writing reviewing and editing; JL: data collection, empirical validation; HB: writing—reviewing and editing; CH: data visualization; AW: methodology, writing—reviewing and editing.
Corresponding author
Ethics declarations
Conflict of interests
The authors declare no competing interests.
Ethics approval
Not applicable.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
10163_2022_1523_MOESM1_ESM.doc
Supplementary file1 Supplementary materials Supplementary material associated with this article can be found in the online version. (DOC 426 KB)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wang, F., Yu, L., Long, J. et al. Quantifying the spatiotemporal evolution characteristics of medical waste generation during the outbreak of public health emergencies. J Mater Cycles Waste Manag 25, 221–234 (2023). https://doi.org/10.1007/s10163-022-01523-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10163-022-01523-5