Abstract
Background
In patients with chronic kidney disease (CKD), dysbiosis in the gastrointestinal microbiome is thought to be associated with increased production of uremic toxins, such as indoxyl sulfate (IS) and p-cresyl sulfate (PCS). Sucroferric oxyhydroxide (SFO), an iron-based phosphate binder, may affect the gastrointestinal microbiome and the production of uremic toxins. We aimed to examine whether SFO administration affected distribution of gastrointestinal microbiome and serum uremic toxin levels in CKD patients undergoing hemodialysis.
Methods
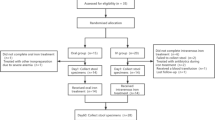
In this single-center, open-label, interventional study, 18 maintenance hemodialysis patients with hyperphosphatemia were prescribed with SFO. We collected serum samples before and after 3 months of administration, and serum levels of IS and PCS were measured. A control group of 20 hemodialysis patients without SFO was evaluated. We evaluated gastrointestinal microbiome of patients pre- and post-SFO administration by 16S rDNA sequencing and bioinformatics analysis.
Results
Serum IS and PCS levels were significantly elevated after administration of SFO (IS before 2.52 ± 1.60 mg/dl vs. after 3.13 ± 1.51 mg/dl, P = 0.008; PCS before 2.32 ± 2.44 mg/dl vs. after 3.45 ± 2.11 mg/dl, P = 0.002), while serum IS and PCS levels did not change in the control group. Microbiome analysis in the SFO group showed no significant change in diversity and major components in phylum, class, order, family, gene, and species.
Conclusion
Administration of SFO increased the serum levels of IS and PCS with no change of major components of gastrointestinal microbiome.




Similar content being viewed by others
References
Han JL, Lin HL. Intestinal microbiota and type 2 diabetes: from mechanism insights to therapeutic perspective. World J Gastroenterol. 2014;20:17737–45.
Festi D, Schiumerini R, Eusebi LH, Marasco G, Taddia M, Colecchia A. Gut microbiota and metabolic syndrome. World J Gastroenterol. 2014;20:16079–94.
Monleón D, Morales JM, Barrasa A, López JA, Vázquez C, Celda B. Metabolite profiling of fecal water extracts from human colorectal cancer. NMR Biomed. 2009;22:342–8.
Qin N, Yang F, Li A, Prifti E, Chen Y, Shao L, et al. Alterations of the human gut microbiome in liver cirrhosis. Nature. 2014;513:59–64.
Frank DN, St Amand AL, Feldman RA, Boedeker EC, Harpaz N, Pace NR. Molecular-phylogenetic characterization of microbial community imbalances in human inflammatory bowel diseases. Proc Natl Acad Sci USA. 2007;104:13780–5.
Moayyedi P, Surette MG, Kim PT, Libertucci J, Wolfe M, Onischi C, et al. Fecal microbiota transplantation induces remission in patients with active ulcerative colitis in a randomized controlled trial. Gastroenterology. 2015;149(102–109):e6.
Vaziri ND, Wong J, Pahl M, Piceno YM, Yuan J, DeSantis TZ, et al. Chronic kidney disease alters intestinal microbial flora. Kidney Int. 2013;83:308–15.
Natarajan R, Pechenyak B, Vyas U, Ranganathan P, Weinberg A, Liang P, et al. Randomized controlled trial of strain-specific probiotic formulation (Renadyl) in dialysis patients. Biomed Res Int. 2014;2014:568571.
Meyer TW, Hostetter TH. Uremic solutes from colon microbes. Kidney Int. 2012;81:949–54.
Lin CJ, Wu V, Wu PC, Wu CJ. Meta-analysis of the associations of p-Cresyl sulfate (PCS) and indoxyl sulfate (IS) with cardiovascular events and all-cause mortality in patients with chronic renal failure. PLoS ONE. 2015;10:e0132589.
Mishima E, Fukuda S, Shima H, Hirayama A, Akiyama Y, Takeuchi Y, et al. Alteration of the intestinal environment by lubiprostone is associated with amelioration of adenine-induced CKD. J Am Soc Nephrol. 2015;26:1787–94.
Heyer CM, Weiss E, Schmucker S, Rodehutscord M, Hoelzle LE, Mosenthin R, et al. The impact of phosphorus on the immune system and the intestinal microbiota with special focus on the pig. Nutr Res Rev. 2015;28:67–82.
Miao YY, Xu CM, Xia M, Zhu HQ, Chen YQ. Relationship between gut microbiota and phosphorus metabolism in hemodialysis patients: a preliminary exploration. Chin Med J (Engl). 2018;131:2792–9.
Dostal A, Lacroix C, Pham VT, Zimmermann MB, Del'homme C, Bernalier-Donadille A, Chassard C. Iron supplementation promotes gut microbiota metabolic activity but not colitis markers in human gut microbiota-associated rats. Br J Nutr. 2014;111:2135–45.
Pereira DI, Aslam MF, Frazer DM, Schmidt A, Walton GE, McCartney AL, et al. Dietary iron depletion at weaning imprints low microbiome diversity and this is not recovered with oral nano Fe(III). Microbiologyopen. 2015;4:12–27.
Jaeggi T, Kortman GA, Moretti D, Chassard C, Holding P, Dostal A, et al. Iron fortification adversely affects the gut microbiome, increases pathogen abundance and induces intestinal inflammation in Kenyan infants. Gut. 2015;64:731–42.
Zimmermann MB, Chassard C, Rohner F, N’goran EK, Nindjin C, Dostal A, et al. The effects of iron fortification on the gut microbiota in African children: a randomized controlled trial in Cote d'Ivoire. Am J Clin Nutr. 2010;92:1406–15.
Dostal A, Chassard C, Hilty FM, Zimmermann MB, Jaeggi T, Rossi S, Lacroix C. Iron depletion and repletion with ferrous sulfate or electrolytic iron modifies the composition and metabolic activity of the gut microbiota in rats. J Nutr. 2012;142:271–7.
Floege J, Covic AC, Ketteler M, Rastogi A, Chong EM, Gaillard S, Lisk LJ, Sprague SM, PA21 Study Group (2014) A phase III study of the efficacy and safety of a novel iron-based phosphate binder in dialysis patients. Kidney Int 86:638–647
Uemura M, Hayashi F, Ishioka K, Ihara K, Yasuda K, Okazaki K, et al. Obesity and mental health improvement following nutritional education focusing on gut microbiota composition in Japanese women: a randomised controlled trial. Eur J Nutr. 2018. https://doi.org/10.1007/s00394-018-1873-0.
Poesen R, Windey K, Neven E, Kuypers D, De Preter V, Augustijns P, et al. The influence of CKD on colonic microbial metabolism. J Am Soc Nephrol. 2016;27:1389–99.
Natoli M, Felsani A, Ferruzza S, Sambuy Y, Canali R, Scarino ML. Mechanisms of defence from Fe(II) toxicity in human intestinal Caco-2 cells. Toxicol In Vitro. 2009;23:1510–5.
Lau WL, Vaziri ND2, Nunes ACF, Comeau AM, Langille MGI, England W, Khazaeli M, Suematsu Y, Phan J, Whiteson K (2018) The phosphate binder ferric citrate alters the gut microbiome in rats with chronic kidney disease. J Pharmacol Exp Ther 367:452–460
Kortman GA, Dutilh BE, Maathuis AJ, Engelke UF, Boekhorst J, Keegan KP, Nielsen FG, Betley J, Weir JC, Kingsbury Z, Kluijtmans LA, Swinkels DW, Venema K, Tjalsma H. Microbial metabolism shifts towards an adverse profile with supplementary iron in the TIM-2 in vitro model of the human colon. Front Microbiol. 2016;6:1481.
Macfarlane GT, Macfarlane S. Bacteria, colonic fermentation, and gastrointestinal health. J AOAC Int. 2012;95:50–60.
Nyangale EP, Mottram DS, Gibson GR. Gut microbial activity, implications for health and disease: the potential role of metabolite analysis. J Proteome Res. 2012;11:5573–85.
Funding
This study was supported by a grant from The Kidney Foundation, Japan.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Ethical approval
The study protocol was performed in accordance with the ethical guidelines of the Declaration of Helsinki and was approved by the human research committee at our institution (authorization No. 1849). Written informed consent was obtained from all participants. The study is registered with the UMIN Clinical Trials Registry (No. 000026667). This study was a prospective, open-label interventional study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Iguchi, A., Yamamoto, S., Oda, A. et al. Effect of sucroferric oxyhydroxide on gastrointestinal microbiome and uremic toxins in patients with chronic kidney disease undergoing hemodialysis. Clin Exp Nephrol 24, 725–733 (2020). https://doi.org/10.1007/s10157-020-01892-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10157-020-01892-x