Abstract
Background
Mizoribine (MZR) therapy after cyclophosphamide (CPM) therapy may be an attractive option in patients with steroid-dependent nephrotic syndrome (SDNS) for the purpose of maintaining remission. This is because CPM is administered only once due to its severe side effects such as gonadal toxicity. However, the long-term prognosis after the treatment regimen remains unknown.
Methods
We retrospectively analyzed the clinical course (median follow-up, 5.9 years) of 54 young children with SDNS (43 boys; age < 10 years) who had undergone 12-week CPM therapy. The patients were classified into two groups: group A, undergoing MZR therapy for > 12 months for maintaining remission after CPM therapy (N = 36), and group B, undergoing CPM monotherapy (N = 18).
Results
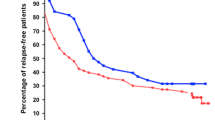
For 2 years after CPM therapy, 21 of the 36 group A patients were in sustained remission, whereas only 4 of the 18 group B patients had maintained remission (58% vs. 22%, p < 0.05). Furthermore, the rate of regression to SDNS after CPM was significantly lower in group A than in group B (6% vs. 39%, p < 0.05). At the last follow-up (mean age, 10.9 years), 27 of the 36 group A patients (75%) had not received any steroid-sparing agent after the treatment regimen.
Conclusions
Single daily high-dose MZR therapy after CPM therapy may have positive outcomes in young children with SDNS in the long term.




Similar content being viewed by others
References
Fujinaga S, Endo A, Ohtomo Y, Ohtsuka Y, Shimizu T. Uncertainty in management of childhood-onset idiopathic nephrotic syndrome: is the long-term prognosis really favorable? Pediatr Nephrol. 2013;28:2235–8.
Ishikura K, Matsumoto S, Sako M, Tsuruga K, Nakanishi K, Kamei K, Saito H, Fujinaga S, Hamasaki Y, Chikamoto H, Ohtsuka Y, Komatsu Y, Ohta T, Nagai T, Kaito H, Kondo S, Ikezumi Y, Tanaka S, Kaku Y, Iijima K, Japanese Society for Pediatric Nephrology, Japanese Society for Pediatric Nephrology. Clinical practice guideline for pediatric idiopathic nephrotic syndrome 2013: medical therapy. Clin Exp Nephrol. 2015;19:6–33.
Kidney Disease Improving Global Outcomes (KDIGO) Glomerulonephritis Work Group. KDIGO clinical practice guideline for glomerulonephritis: Steroid-sensitive nephrotic syndrome in children. Kidney Int Suppl. 2012;2:163–71.
Fujinaga S, Hirano D, Nishizaki N, Someya T, Ohtomo Y, Ohtsuka Y, Shimizu T, Kaneko K. Single daily high-dose mizoribine therapy for children with steroid-dependent nephrotic syndrome prior to cyclosporine administration. Pediatr Nephrol. 2011;26:479–83.
Fujinaga S, Endo A, Watanabe T, Hirano D, Ohtomo Y, Shimizu T, Kaneko K. Maintenance therapy with single-daily, high-dose mizoribine after cyclophosphamide therapy for prepubertal boys with severe steroid-dependent nephrotic syndrome. Clin Nephrol. 2012;78:251–2.
International Study of Kidney Disease in Children. Nephrotic syndrome in children: prediction of histopathology from clinical and laboratory characteristics at time of diagnosis. A report of the International Study of Kidney Disease in Children. Kidney Int. 1978;13:159–65.
Ishikura K, Yoshikawa N, Hattori S, Sasaki S, Iijima K, Nakanishi K, Matsuyama T, Yata N, Ando T, Honda M, for Japanese Study Group of Renal Disease in Children. Treatment with microemulsified cyclosporine in children with frequently relapsing nephrotic syndrome. Nephrol Dial Transpl. 2010;25:3956–62.
Iijima K, Sako M, Oba MS, Ito S, Hataya H, Tanaka R, Ohwada Y, Kamei K, Ishikura K, Yata N, Nozu K, Honda M, Nakamura H, Nagata M, Ohashi Y, Nakanishi K, Yoshikawa N, Japanese Study Group of Kidney Disease in Children. Cyclosporine C2 monitoring for the treatment of frequently relapsing nephrotic syndrome in children: a multicenter randomized phase II trial. Clin J Am Soc Nephrol. 2014;9:271–8.
Ishikura K, Yoshikawa N, Nakazato H, Sasaki S, Iijima K, Nakanishi K, Matsuyama T, Ito S, Yata N, Ando T, Honda M, Japanese Study Group of Renal Disease in Children. Two-year follow-up of a prospective clinical trial of cyclosporine for frequently relapsing nephrotic syndrome in children. Clin J Am Soc Nephrol. 2012;7:1576–83.
Ishikura K, Yoshikawa N, Nakazato H, Sasaki S, Nakanishi K, Matsuyama T, Ito S, Hamasaki Y, Yata N, Ando T, Iijima K, Honda M, Japanese Study Group of Renal Disease in Children. Morbidity in children with frequently relapsing nephrosis: 10-year follow-up of a randomized controlled trial. Pediatr Nephrol. 2015;30:459–68.
Trompeter RS, Lloyd BW, Hicks J, White RH, Cameron JS. Long-term outcome for children with minimal-change nephrotic syndrome. Lancet. 1985;16:368–70.
Lewis MA, Baildom EM, Davis N, Houston IB, Postlethwaite RJ. Nephrotic syndrome: from toddlers to twenties. Lancet. 1989;4:255–9.
Fakhouri F, Bocquet N, Taupin P, Presne C, Gagnadoux MF, Landais P, Lesavre P, Chauveau D, Knebelmann B, Broyer M, Grünfeld JP, Niaudet P. Steroid-sensitive nephrotic syndrome: from childhood to adulthood. Am J Kidney Dis. 2003;41:550–7.
Rüth EM, Kemper MJ, Leumann EP, Laube GF, Neuhaus TJ. Children with steroid-sensitive nephrotic syndrome come of age: long-term outcome. J Pediatr. 2005;147:202–7.
Kyrieleis HA, Levtchenko EN, Wetzels JF. Long-term outcome after cyclophosphamide treatment in children with steroid-dependent and frequently relapsing minimal change nephrotic syndrome. Am J Kidney Dis. 2007;49:592–7.
Cammas B, Harambat J, Bertholet-Thomas A, Bouissou F, Morin D, Guigonis V, Bendeddouche S, Afroukh-Hacini N, Cochat P, Llanas B, Decramer S, Ranchin B. Long-term effects of cyclophosphamide therapy in steroid-dependent or frequently relapsing idiopathic nephrotic syndrome. Nephrol Dial Transpl. 2011;26:178–84.
Vester U, Kranz B, Zimmermann S, Hoyer PF. Cyclophosphamide in steroid-sensitive nephrotic syndrome: outcome and outlook. Pediatr Nephrol. 2003;18:661–4.
Azib S, Macher MA, Kwon T, Dechartres A, Alberti C, Loirat C, Deschênes G, Baudouin V. Cyclophosphamide in steroid-dependent nephrotic syndrome. Pediatr Nephrol. 2011;26:927–32.
Ueda N, Kuno K, Ito S. Eight and 12 week courses of cyclophosphamide in nephrotic syndrome. Arch Dis Child. 1990;65:1147–50.
Kemper MJ, Altrogge H, Ludwig K, Timmermann K, Müller-Wiefel DE. Unfavorable response to cyclophosphamide in steroid-dependent nephrotic syndrome. Pediatr Nephrol. 2000;14:772–5.
Zagury A, de Oliveira AL, de Moraes CA, de Araujo Montalvão JA, Novaes RH, de Sá VM, de Carvalho DDBM, Matuck T. Long-term follow-up after cyclophosphamide therapy in steroid-dependent nephrotic syndrome. Pediatr Nephrol. 2011;26:915–20.
Takeuchi S, Hiromura K, Tomioka M, Takahashi S, Sakairi T, Maeshima A, Kaneko Y, Kuroiwa T, Nojima Y. The immunosuppressive drug mizoribine directly prevents podocyte injury in puromycin aminonucleoside nephrosis. Nephron Exp Nephrol. 2010;116:e3–10.
Nakajo A, Khoshnoodi J, Takenaka H, Hagiwara E, Watanabe T, Kawakami H, Kurayama R, Sekine Y, Bessho F, Takahashi S, Swiatecka-Urban A, Tryggvason K, Yan K. Mizoribine corrects defective nephrin biogenesis by restoring intracellular energy balance. J Am Soc Nephrol. 2007;18:2554–64.
Ohtomo Y, Fujinaga S, Takada M, Murakami H, Akashi S, Shimizu T, Kaneko K, Yamashiro Y. High-dose mizoribine therapy for childhood-onset frequently relapsing steroid-dependent nephrotic syndrome with cyclosporin nephrotoxicity. Pediatr Nephrol. 2005;20:1744–9.
Kawasaki Y, Suzuki J, Takahashi A, Isome M, Nozawa R, Suzuki H. Mizoribine oral pulse therapy for steroid-dependent nephrotic syndrome. Pediatr Nephrol. 2005;20:96–8.
Fujieda M, Ishihara M, Morita T, Hayashi A, Utsunomiya Y, Ohta T, Sakano T, Wakiguchi H. Effect of oral mizoribine pulse therapy for frequently relapsing steroid-dependent nephrotic syndrome. Clin Nephrol. 2008;69:179–84.
Yoshioka K, Ohashi Y, Sakai T, Ito H, Yoshikawa N, Nakamura H, Tanizawa T, Wada H, Maki S. A multicenter trial of mizoribine compared with placebo in children with frequently relapsing nephrotic syndrome. Kidney Int. 2000;58:317–24.
Takahashi S, Wakui H, Gustafsson JA, Zilliacus J, Itoh H. Functional interaction of the immunosuppressant mizoribine with the 14-3-3 protein. Biochem Biophys Res Commun. 2000;274(1):87–92.
Ito S, Ikeda H, Harada T, Kamei K, Takahashi E. Cyclophosphamide followed by mizoribine as maintenance therapy against refractory steroid dependent nephrotic syndrome. Pediatr Nephrol. 2011;26:1921–2.
Funding
SF received clinical research funding B at Saitama Children’s Medical Center.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest.
Ethical standards
All procedures performed in studies involving human participants were in accordance with the ethical standards of the Institutional Research Committee and/or National Research Committee at which the study was conducted (approval number 2018-02-19) with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all participants included in this study.
About this article
Cite this article
Mizutani, A., Fujinaga, S., Sakuraya, K. et al. Positive effects of single-daily high-dose mizoribine therapy after cyclophosphamide in young children with steroid-dependent nephrotic syndrome. Clin Exp Nephrol 23, 244–250 (2019). https://doi.org/10.1007/s10157-018-1628-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10157-018-1628-5